Dear Members (a note from Bob Marckini):
If someone had told me a year ago that someday soon, the necessities of life would include toilet paper and hand sanitizer; that I wouldn’t be allowed to shake hands with friends or hug my granddaughter; that I’d be putting on a mask to enter a bank; that I’d be practicing something called “social distancing;” that I’d have to make reservations to attend church services; that I’d eat dinner in the parking lot of my favorite restaurant in a tent; and that I’d be sanitizing my daily newspaper and mail with an ozonator, I’d have told them they’re out of their minds. But here we are … well, I’m sure you’re not ozonating your mail, but you’re probably doing all the other things I mentioned. It’s amazing how the world can change in a heartbeat when a virus attacks our planet.
Fortunately, the measures our local, state, and federal governments are taking, and the rules they’ve imposed – for the most part – seem to be working, as COVID-19 infection rates and deaths are leveling off within the U.S. and around the world.
But even after we gain control of the spread of coronavirus, the economy fully opens, and the pharmaceutical companies have developed therapeutic drugs and vaccines to treat and prevent the virus, the world will never be the same. That saddens me. In some ways, it reminds me of how the events of 9-11 changed the world … forever. But we’re resilient; we’ll get through this; and everything will be okay. As Deb said in last month’s opening memo, “This too shall pass.”
In this month’s BOB Tales, we report on some exciting breakthrough technologies that are greatly improving the way doctors can detect prostate cancer. These new blood tests and imaging developments represent a quantum leap in prostate cancer detection and will likely result in a significant reduction in invasive and painful biopsies. Also, cancer detection certainly could improve from today’s 25 to 40 percent to as much as 99 percent with these new technologies.
The Spotlight on Members article this month is a departure from our usual reporting. It’s a heartwarming story about one of our members, Mike Sayles, and his son, Evan, and their journey across the U.S. on a tandem bicycle. There’s nothing ordinary about this escapade, which took them 12 years to complete.
During the adventure, Evan grew from a small, pudgy-cheeked, 10-year-old boy – two-thirds his 59-year-old father’s height – to a 22-year-old man with a full beard, a foot taller than his 71-year-old dad at the end of this odyssey. Both father and son endured serious health challenges during the journey and their lives were forever changed by this extraordinary adventure, which they call, Me, My Dad and America.
To me, this is just one more example of how proton therapy helped one man heal, and a father-son team complete the adventure of a lifetime. I think you’ll enjoy reading their story.
September is National Prostate Cancer Awareness Month. Prostate cancer affects more than three million men every year worldwide. Roughly one in nine men in the U.S. will be diagnosed with prostate cancer this year. We’re among the lucky ones who discovered proton therapy. This month is a good time to remind our male family members and friends to learn about diet and lifestyle steps they can take to help prevent prostate cancer; to make sure they’re having annual physicals; and to pay attention to their PSA results, particularly over time.
Finally, Sept. 20 is “Wife Appreciation Day.” Need I say more?
We hope you enjoy this issue of BOB Tales and as always, we welcome and encourage your feedback. Please send an email to [email protected].
Bob Marckini
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
In This Issue:
- Non-invasive MRI Detects Significant Prostate Cancer
- Newest PET/CT Scan for Recurrent Prostate Cancer
- More Reasons to Continue PSA Screening
- New/Modified PSA Test Predicts Need for Biopsy
- New CTC Test Improves Early Detection
- New Prostate Cancer Risk Calculator
- Prostate Cancer Drug Used to Treat COVID19
- Body Weight Influences Cancer Recurrence
- Aspirin Against Migraines and Cancer
- Recap: 2020 Virtual Proton Conference


Non-invasive MRI: Prostate Cancer Detection Breakthrough
An extremely important study, reported in Medscape Medical News, has shown that advanced MRI imaging technology has greatly improved the ability to detect clinically significant prostate cancers.
Analysis of data from the Prostate MR Imaging Study (PROMIS) suggests that multiparametric MRI (mp-MRI) can deliver crucial information about a man’s risk of dying from prostate cancer before a biopsy is done. “This may mean that we can finally move prostate cancer to a position in which we can use imaging as the primary tool to direct further investigations, treatment, and prediction of risk,” said Joseph Norris, BM BS, from University College London. “This is a position that all other solid organ cancers have reached,” he said.
The mp-MRI had a 93 percent sensitivity for clinically significant cancer vs. the conventional TRUS (trans-rectal ultrasound guided) biopsy, which showed a 48 percent sensitivity. Researchers concluded that mp-MRI can be used as a first-line diagnostic tool that could prevent at least 27 percent of invasive biopsies.
Further study showed that the 7 percent of cancers missed by mp-MRI were lower grade cancers than the 52 percent that were missed by TRUS biopsy. “No highly aggressive prostate cancers were missed by MRI,” said researcher Joseph Norris.
Bad News/Good News
“The elephant in the room remains the considerable variation in technique and interobserver interpretation of prostate mp-MRI,” said Steven Mondola, MD, and Marc Dall’Era, MD, from UC Davis Health in Sacramento, CA. This means that the application of the technology and the interpretation of the results are heavily influenced by the training and expertise of the medical practitioners doing the testing.
The good news is that the excellent results reported above were obtained using 1.5 Tesla mp-MRI. Today’s state-of-the-art is 3T mp-MRI, a much greater precision imaging technology, where even better diagnostic results can be expected. Even so, the experience and skill of the medical practitioner are still critically important in interpreting results.
We reported in our February 2020 BOB Tales that in November 2019, Deb Hickey and Bob Marckini traveled to Alpharetta, GA to attend the grand opening of the Busch Center, a facility that specializes in 3T mp-MRI prostate imaging. Dr. Joseph Busch is a world leader in this imaging technology application and interpretation.
.jpg)
.jpg)
Newest PET/CT Scan for Recurrent Prostate Cancer Shows Much Promise
 According to a recent study, reported in Diagnostic Imaging, 30 to 40 percent of men who are treated for prostate cancer have a biochemical recurrence when their PSA levels rise after initial treatment. This 30 to 40 percent statistic hasn’t been our observation or experience with proton therapy, but may be the case for those who undergo surgery or other treatments.
According to a recent study, reported in Diagnostic Imaging, 30 to 40 percent of men who are treated for prostate cancer have a biochemical recurrence when their PSA levels rise after initial treatment. This 30 to 40 percent statistic hasn’t been our observation or experience with proton therapy, but may be the case for those who undergo surgery or other treatments.
Typically, doctors use different imaging techniques to identify the location of the recurrence and then prescribe one of many treatment options to either destroy the cancer, in the case of a small number of lesions, or manage the cancer systemically, in the case of multiple metastases.
One of the newest imaging technologies is called 18F-DCFPyL prostate-specific membrane antigen (PSMA) PET/CT.
At a recent meeting of the Society of Nuclear Medicine and Molecular Imaging 2020, investigators at the University of Toronto reported that 18F-DCFPyL PSMA PET/CT scan has proven to be much more effective at identifying specific lesions than other PET/CT techniques.
Researchers conducted a large-scale, multi-center clinical trial with 410 men with biochemical failure post-primary therapy. The 18F-DCFPyL PSMA PET/CT scan found disease in more than half of the men who had negative CT and bone scans. This led to changes in treatment in 66 percent of patients, including conversion from active surveillance or systemic therapy to surgery, radiation, or nodal-directed therapy to salvage surgery or radiation.
PSMA PET is still considered investigational in North America, but this new evidence could result in regulatory approval to make 18F-DCFPyL more widely available in the U.S.

.jpg)
The Long-term Benefits of PSA Screening
Routine PSA testing may have benefits that aren’t evident in short-term studies, according to new commentary published in The New England Journal of Medicine. Experts suggest the advantages of widespread screening, including reduced mortality and the potential to avoid metastases, are likely greater than previously gauged.
The PSA Timeline
.jpg) The PSA test was developed in the 1980s. In 1994, the Food and Drug Administration approved it as a screening tool for prostate cancer.
The PSA test was developed in the 1980s. In 1994, the Food and Drug Administration approved it as a screening tool for prostate cancer.
In 2002, the U.S. Preventive Services Task Force (USPSTF) claimed there wasn’t enough evidence to recommend either for or against routine PSA testing. They were confident that PSA screening could detect early-stage prostate cancer, but found mixed and inconclusive evidence that early detection improved health outcomes. A concern was that PSA screening was associated with important harms including false-positive results, unnecessary biopsies, infection, and potential complications from treatment of cancer that may never have affected a patient’s health.
In 2008, the USPSTF recommended against prostate cancer screening for men age 75 and older. At the same time, they concluded that for men younger than 75, the benefits of PSA testing were uncertain as the balance of benefits and harms couldn’t be determined.
In 2012, the USPSTF recommended against routine PSA screening for men in the general population regardless of age. As a result, the use of PSA testing declined significantly. At the same time, metastatic prostate cancer in older men began to rise after reaching an all-time low in 2011.
In April 2017, the task force reevaluated its stance against routine PSA testing and asked clinicians to “individualize decision making” about screening.
In May 2018, the USPSTF released their final recommendation on PSA testing recommmending men ages 55 to 69 make an individual decision after discussing the potential benefits and harms and their specific clinical circumstances with their clinician. For men 70 and older, they condcluded the potential benefits don’t outweigh the harms, and these men shouldn’t be routinely screened for prostate cancer.
The Latest Research
Investigators from Weill Cornell Medicine, New York Presbyterian, University of Washington School of Medicine and the Fred Hutchinson Cancer Research Center aimed to better understand the benefits of PSA testing and help more men receive the right treatment at the right time, while reducing the risk of metastasis. They suggest the recommendations by the USPSTF and some others are based on “problematic estimates of the benefits and harms of screening.” They believe the evidence indicates that more widespread screening would reduce mortality rates and help patients avoid metastatic disease.
The authors of this latest analysis say current decision aids are based on an incomplete picture and that the time frame examined – generally 13 years from screening – isn’t long enough. “Most men who begin screening in their 50s will live much longer than 13 years. We need to look over a lifetime to understand the risks and benefits of screening,” says co-lead author Dr. Jonathan Shoag.
After analyzing data from previous studies and making conservative assumptions, researchers suggest the survival benefits of screening became more apparent with longer follow-up. “Our results show that continued accrual of benefit over time creates a significantly more favorable picture of the value of screening,” said co-author Yaw Nyame, MD.
“More men should have the opportunity to get the benefits of screening. In my opinion, these outweigh the potential harms over a longer, more realistic time horizon for most healthy men,” said Shoag.

.jpg)
The Future of Prostate Cancer Screening
PSA testing has its benefits – including reducing the death rate due to prostate cancer in men who are screened and reducing the need for treatment of metastatic disease. However, it has limitations. For example, the PSA test can’t distinguish between non-cancerous prostate enlargement and prostate cancer.
IsoPSA®
In 2015, the Cleveland Clinic partnered with Cleveland Diagnostics, Inc. to develop a
more comprehensive PSA test. IsoPSA® can search out molecular structural changes in PSA protein instead of focusing on just the concentration of PSA in the blood. IsoPSA® can more accurately predict whether or not someone has prostate cancer and help physicians determine whether or not a biopsy is needed.
Promising Studies
A preliminary study showed that IsoPSA® was a better predictor of the overall risk of prostate cancer and the risk of clinically significant prostate cancer than the traditional PSA test.
A follow-up study revealed that when used in a clinical setting, IsoPSA® reduced unnecessary prostate biopsies by more than 40 percent while accurately determining the presence of aggressive disease. Furthermore, the test’s ability to identify high-grade tumors when used in conjunction with multiparametric magnetic resonance imaging (mpMRI)-guided biopsy could help physicians develop better diagnostic treatment plans for prostate cancer patients.
FDA Approval
The IsoPSA® received breakthrough device designation – a program for medical products that provide for more effective treatment or diagnosis of life-threatening or irreversibly debilitating diseases or conditions – from the U.S. Food & Drug Administration late last year. This distinction is expected to accelerate the regulatory process so the test can be made widely available.
What’s Next?
The IsoPSA® will be implemented at the Cleveland Clinic health system’s Ohio locations. A team of researchers will continue to examine best practices and efficiencies for the test’s clinical application and trial process.
CTC Test
Australian researchers also revealed a new method for improving early detection of prostate cancer – the ISET-CTC test. The findings are published in the journal Frontiers in Oncology.
What is CTC?
CTC stands for Circulating Tumor Cells. An increase in CTCs is associated with cancer progression and a CTC decrease with cancer containment or remission. Several technologies have been developed to identify CTC. The ISET-CTC identifies abnormal cells circulating in the blood from any origin. Monitoring the presence of CTC cells may help detect prostate cancer earlier.
Research Findings
Researchers at the National Institute of Integrative Medicine (NIIM) used the ISET-CTC test plus the PSA marker test to evaluate the risk of developing prostate cancer in a group of Australian men. Their findings suggest that the combination of ISET-CTC testing and PSA marker testing offers a much greater certainty about diagnosis (99 percent) than the standard PSA test (25 percent).
What’s Next?
Researchers at NIIM plan to launch a population study. They’re looking for 50- to 75-year-old males to participate in the research to further evaluate the clinical benefits of the ISET-CTC test. They expect the next phase of research to provide more significant results as they hope to engage with a much larger population group.
Me, My Dad, and America
Mike Sayles contacted Bob Marckini in 2011 to learn about proton therapy as a possible treatment option for his prostate cancer. Shortly thereafter, Mike was treated at Loma Linda University Cancer Center and became a member of our group.
A few years later, Mike and his wife Joyce moved their summer residence to Bob’s little seaside neighborhood in Mattapoisett, MA and he and Bob became good friends. These days, they regularly play golf together (Mike beats Bob most of the time).
As mentioned in the opening memo, Mike did something that most of us can only dream about – beginning in 2006, he bicycled across the country with his son. Because their ride was done in multiple segments, this adventure-of-a-lifetime lasted 12 years.
Bob asked if he could interview Mike and his son, Evan, about their trip and they agreed. Following is their story in their own words.
How did this odyssey come about?
 Mike: Shortly after my divorce from Evan’s mother, they moved to Texas. It soon became clear that being an occasional fly-in weekend father wasn’t enough and we needed something special to do together – something long-term – an activity we could plan for and look forward to.
Mike: Shortly after my divorce from Evan’s mother, they moved to Texas. It soon became clear that being an occasional fly-in weekend father wasn’t enough and we needed something special to do together – something long-term – an activity we could plan for and look forward to.
Evan: Dad proposed the idea when I was 9 or 10, and I thought it sounded cool (though I wasn’t sure if it would last more than a couple trips). He’s always had a penchant for making fabulous, elaborate plans. I didn’t fully appreciate the scale of the adventure until a few years later.
Can you explain your slogan, “Me, My Dad, And America”?
Mike: Two years into the adventure (2008), Evan started writing a blog at the end of each day we rode. It’s what he named the blog. Originally, I wanted to name our trip “4 Legs, 2 wheels, 1 Dream!”
Evan: I’m a numbers guy, but “4 Legs, 2 Wheels, 1 Dream” was a bit much, even for me.
Why a tandem bike?
Mike: A longtime friend and bike store owner in Providence, RI suggested we ride a tandem. As I look back, that idea probably saved our ride. My two key roles were safety and logistics. From a safety perspective, knowing exactly where Evan was while we were riding, especially in the first few years, was very important. And having to deal with only one bike was good too. Plus, it was easy to talk to each other!
Evan: I was in favor right away as well. Photos of me from that time reveal that I wasn’t much of an athlete, so I was perfectly okay with having my dad haul me up and down the Continental Divide. The only downside was being inches behind him after he’d had a spicy lunch.
When and where did you start and complete this adventure?
Mike: It began on Oct. 26, 2006, just west of Astoria, OR near the mouth of the Columbia River with our rear tire dipped in the Pacific. We finished the journey June 2, 2018 in Newport, RI with our front tire dipped in the Atlantic.
How many bike changes did you make during the 12 years?
Mike: It became apparent, following our third year, that Evan’s significant growth spurt would mean a new bicycle would be needed. We ordered one from a bike shop in Spokane, WA. A few summers later, additional modifications were made at another bike shop in Rapid City, SD. That change lasted the rest of the trans-America ride.
Evan: The modifications were mostly extensions of the back seatpost. Usually the taller tandem rider takes the front seat, so we may have looked a bit silly with me leaning over him as I grew – not that I’m calling him short!
What states did you pass through, and how many segments to your trip?
Mike: We passed through Oregon, parts of Washington state, Idaho, Montana, Northeast Wyoming, South Dakota, Northeast Nebraska, Iowa, Illinois, Indiana, Ohio, Northwest Pennsylvania, New York, Massachusetts, Northeast Connecticut, Rhode Island. There were 12 segments – the longest being 414 miles in one week. We typically rode in the summer or early fall, and each segment was between four and seven days. As Evan grew older, it became more difficult to find those “free days” for us to travel and ride.
Evan: I take after my dad in that I like to jam-pack my vacation time. Between summer camp and pre-season activities in high school, I started to present a lot of scheduling challenges.
Where did you sleep?
Mike: As I was responsible for logistics, I worked hard to space out our riding so we could stay in hotels or local motels most nights. On our ride across Iowa, we camped out as part of a “supported” group of trans-state riders during an event called “RAGBRAI.” More on that later.
Evan: I would’ve been fine camping roadside for most of our segments, but I don’t think Dad’s much of a camper. We were lucky to be able to test out pretty much every Hampton Inn waffle iron along our route.
What was the biggest challenge of the adventure?
Mike: The Bitterroot Mountain Range in Idaho – 99 miles of steep, twisting, narrow road that we shared with a lot of rented campers and large oil drilling equipment heading to North and South Dakota.
Evan: The semi-trucks piled high with logs were pretty scary too. I remember one narrow bridge where we were getting approached from ahead and behind by two of those rigs – definitely a “hold-your-breath-and-pray” moment.
Any weather challenges?
Mike: Overall, we were extremely fortunate weather-wise. We did, however, have to out-run a number of summer thunderstorms and one nasty hailstorm.
Evan: Another advantage of the tandem is I could look at radar on my phone while we were biking. We were able to make quick adjustments on the move.
Any accidents or injuries along the way?
Mike: I’m proud that with the exception of just two flat tires, on back-to-back days in Illinois, we had no accidents or injuries.
Evan: Though there were a few moments where I may have wanted to cause one …
Most memorable event from your journey?
Mike: The largest “trans-state” and bike touring event in the world, RAGBRAI, is an acronym for Register’s (The Des Moines Register) Annual Great Bicycle Ride Across Iowa. It’s a non-competitive west to east (better winds) started by two writers from Iowa’s largest newspaper in 1973.
We scheduled our 2013 ride to coincide with this event. Great fun, but so unlike all our other segments when we were riding by ourselves and not with thousands of others. It took a bit of getting used to!
Evan: RAGBRAI was so much fun every single day. All the towns on the route were so hospitable, and there was a ton of amazing food. That ride is also where my parents first met!
Details of your final day?
 Mike: On Saturday, June 2, 2018 we rode our victory lap – just 3.5 miles from a parking lot at Fort Adams State Park in Newport, RI to a pre-selected location on Ocean Drive to dip our front tire into the Atlantic and officially complete our trans-America bicycle ride. We arranged to have rented bicycles available for any of our invited friends, and over 25 joined, including Bob and Pauline Marckini. Others brought their own bikes. It was a beautiful morning and smiles were everywhere. Following a very brief ceremony and lots of picture taking, the bikes were returned to the rental company and the riders were taken back to Fort Adams in a sightseeing bus. The entire entourage was invited to a celebratory luncheon at Sardella’s Italian Restaurant in the heart of Newport.
Mike: On Saturday, June 2, 2018 we rode our victory lap – just 3.5 miles from a parking lot at Fort Adams State Park in Newport, RI to a pre-selected location on Ocean Drive to dip our front tire into the Atlantic and officially complete our trans-America bicycle ride. We arranged to have rented bicycles available for any of our invited friends, and over 25 joined, including Bob and Pauline Marckini. Others brought their own bikes. It was a beautiful morning and smiles were everywhere. Following a very brief ceremony and lots of picture taking, the bikes were returned to the rental company and the riders were taken back to Fort Adams in a sightseeing bus. The entire entourage was invited to a celebratory luncheon at Sardella’s Italian Restaurant in the heart of Newport.
Evan: We were so fortunate to be joined by our friends and family for the last ride. I think having them ride along for the last few miles really helped them see what a great bonding experience Dad and I had the whole way.
Was the trip’s purpose/objective achieved?
Mike: For me, the father who wanted something of significance to share with his son, the answer is a resounding “absolutely.” The young boy who started out with me on a cool blustery late afternoon on the Pacific became the tall, strong “engine” of our trip and kept us moving forward. I observed his resiliency, his keen sense of humor, and above all his profound ability to live in the moment. We both discovered that we live in a beautiful country populated with some terrific people. We stood on the roof of America (The Rockies), traveled next to fast-moving rivers, past miles of sparse terrain, followed by days of lush fields of wheat and corn. There was a life parallel with our adventure which will remain a part of us.
We each had other difficulties that needed to be addressed. In my case, my prostate issues where heading in the wrong direction and decisions needed to be made. Having done all the research I possibly could uncover, the end result was the proton facility at Loma Linda University Cancer Center – a truly life-changing positive experience for me and my wife. My son was diagnosed with type 1 diabetes in the fall of 2015 when he was a sophomore in college. In both instances, the desire to continue our ride was additional motivation and commitment.
 Evan: As a 10-year-old, my goal was initially just to get on the bike and move east. As I got older and we kept at it, I started to recognize what a special experience we were sharing. I’m proud of us both for keeping at it through the health challenges we faced. We had a fantastic adventure; saw so many great sights; and met some amazing people along the way. Those years on the bike helped make me the person I am today — and kept me close with my amazing dad. Whatever the original purpose or objective may have been, our journey together was a complete success.
Evan: As a 10-year-old, my goal was initially just to get on the bike and move east. As I got older and we kept at it, I started to recognize what a special experience we were sharing. I’m proud of us both for keeping at it through the health challenges we faced. We had a fantastic adventure; saw so many great sights; and met some amazing people along the way. Those years on the bike helped make me the person I am today — and kept me close with my amazing dad. Whatever the original purpose or objective may have been, our journey together was a complete success.
Watch a video of Mike and Evan’s trip.

.jpg)
Love Your Urologist?
Over the years we’ve collected a list of physicians from our members as they’ve completed treatment and went on to search for urologists who are open-minded and/or knowledgable about proton therapy as a viable treatment option. These doctors appreciate the fact that patients have done their own homework, moved forward with a treatment based on their own research and comfort level, and are doing well after treatment.
If you have a urologist you’re fond of and you think BOB members in your area may benefit from his/her services, please send an email to [email protected].

You Can Beat Prostate Cancer:
And You Don’t Need Surgery to Do It – Second Edition
In the MRI Prostate Cancer Detection Breakthrough article above, we noted that Bob and Deb had the opportunity to meet Dr. Joseph Busch and his wife Kathy at the grand opening of their new state-of-the-art prostate cancer diagnostic facility in Alpharetta, GA. Both were trained in 3T mp-MRI technology by world-leading experts, Professors Jelle Barenstz, Jurgen Futterer and Anwar Padhani in Europe. Dr. Busch has also lectured and taught mp-MRI at the Radiological Society of North America (RSNA) and Johns Hopkins, and is a member of ESUR, the International Cancer Imaging Society and RSNA.
 When Bob and Deb visited the Busches in November last year, they presented them with a copy of the manuscript of Bob’s new book asking for feedback and suggestions. The two were extremely impressed with the book, provided comments/suggestions, and agreed to endorse it. Following is a copy of the Busches endorsement which appears at the beginning of Bob’s new book along with several others by prominent medical professionals:
When Bob and Deb visited the Busches in November last year, they presented them with a copy of the manuscript of Bob’s new book asking for feedback and suggestions. The two were extremely impressed with the book, provided comments/suggestions, and agreed to endorse it. Following is a copy of the Busches endorsement which appears at the beginning of Bob’s new book along with several others by prominent medical professionals:
“For any patient faced with the diagnosis of prostate cancer, there will be fear and anxiety. Most men will do well if they are educated on the nature and status of their disease. In easy-to-read language, Robert Marckini’s book does an excellent job of informing patients on their prostate cancer diagnosis, treatment options, life after treatment, and much more. ‘You Can Beat Prostate Cancer’ is a practical and comprehensive guide for men at risk for prostate cancer or for men recently diagnosed with the disease. This is a book that every prostate cancer patient should read before making a decision on treatment or surveillance.”
-Joseph J. Busch Jr. MD Oncological Radiologist, Busch Center, Kathy Busch BS, RT (N) (MR), (CT), CNMT (PET)
The book is doing well on Amazon, sitting in the first or second position out of 4,000 books on a “prostate cancer” search. It’s also being distributed by proton centers to patients making inquiries about proton therapy for prostate cancer.
We’re thrilled the book is helping men and their loved ones understand their diagnosis and treatment options, as well as learn about the benefits of proton therapy for prostate cancer.
Reminders
The second edition of You Can Beat Prostate Cancer includes a complete update on prostate cancer prevention, imaging technology, diagnostic technology, treatment options, and virtually all aspects of the latest developments in proton therapy.
Proton centers are beginning to acquire the new book and send it to patients making inquiries about proton therapy. We have no doubt this will educate patients on the benefits of proton therapy and help them with their treatment decisions.
We are happy to discount books in quantity (minimum 20) to anyone who is interested spreading the word on proton therapy. Just send an email to [email protected]. Proceeds from book sales are used to help fund our efforts and to support proton therapy research.
Please note: The Kindle version is free to Kindle Unlimited members or can be purchased for only $9.99, for non-members. The soft-cover price is $22.45

Buy You Can Beat Prostate Cancer second edition on Amazon or Lulu Press.


Body Weight Influences Prostate Cancer Recurrence and Mortality
Obesity will soon overtake tobacco as the leading cause of preventable cancer in the U.S. where approximately 40 percent of people are considered obese. The Journal of Clinical Oncology recently reported that obesity has been associated with a higher risk of prostate cancer recurrence, developing metastatic disease and dying from prostate cancer. Even modest weight gain can increase chances of prostate cancer recurrence and cancer-related mortality.
In one study involving more than 8,000 men, researchers found a significantly positive association between post diagnostic obesity and prostate cancer mortality among men with low-risk tumors (T1-T2, or Gleason ≤ 7). And men who gained more than 5 percent of body weight after diagnoses, had a higher risk of death from prostate cancer than men who maintained a stable weight.
This data prompt the question, “If obesity and weight gain are significant risk factors for death from prostate cancer, can weight loss be protective?” While one would think, this might be the case, unfortunately there have been no studies to specifically address this question. However, we do know studies have shown that weighing what you ought to weigh can significantly benefit overall health, preventing cancers of all types as well as reducing the chances of death from cardiovascular, autoimmune and other diseases.

.jpg)
Rising from Bed Too Quickly Can Be Hazardous
A viral social media message has been circulating the Web for some time, reportedly from a cardiologist, suggesting the “one-and-a-half-minute law.” It purports that waking up suddenly from sleep and standing to go to the bathroom can result in dizziness or possible stroke and death.
The message continues with a suggestion to lie awake for 30 seconds after waking; then sit up for 30 seconds; next, lower your legs and sit for another 30 seconds. Only then should you get up to use the bathroom. This, according to the message, can be especially important for older folks.
We fact checked the story and discovered there’s apparently no scientific evidence supporting the claim that rising quickly from bed can cause a stroke or sudden death. However, according to Mayo Clinic, orthostatic hypotension – also called postural hypotension – is a form of low blood pressure that happens when you stand up from sitting or lying down. The condition can make you feel dizzy or lightheaded, and maybe even faint.
We shared this information with friends who told us the information was helpful. One friend wrote back with the following:
It seems like good advice whether you’re elderly or not, for three reasons:
- Gives your eyes time to adjust
- Gives your mind time to clear
- Gives the dog time to get the heck out of the way
Aspirin Against Migraines and Cancer
 For an inexpensive drug that’s been around for more than 120 years, it’s amazing that there continues to be new discoveries about aspirin. The latest has to do with its use in the prevention of migraine headaches and helping to reduce the risk of certain types of cancers.
For an inexpensive drug that’s been around for more than 120 years, it’s amazing that there continues to be new discoveries about aspirin. The latest has to do with its use in the prevention of migraine headaches and helping to reduce the risk of certain types of cancers.
Migraines
Dr. Charles Hennekens, one of the world’s top scientists and contributor to three textbooks and more than 750 medical publications, and his colleagues reviewed data on aspirin over the past several decades. They concluded, “The totality of evidence, which includes data from randomized trials, suggests that high-dose aspirin, in doses from 900 to 1,300 mg, given at the onset of symptoms, is an effective and safe treatment option for acute migraine headaches. In addition, the totality of evidence, including, some but not all, randomized trials, suggests the possibility that daily aspirin in doses from 81 to 325 mg, may be an effective and safe treatment option for the prevention of recurrent migraine headaches.”
Of course, no one should take high doses of aspirin without first consulting a doctor. The same holds true for long-term use. Aspirin can cause digestive problems, gastrointestinal bleeding, and allergic reaction.
Cancer
Aspirin continues to generate excitement with its anti-cancer properties. Scientists have reported that patients taking low-dose aspirin have better survival statistics against head and neck cancer, as well as non-small-cell lung cancer. Evidence also suggests regular aspirin use reduces the risk of colorectal and other digestive tract cancers. Aspirin may also provide some protection against breast and prostate cancer.
Again, you should always consult with your physician before taking a new drug. And a health professional should monitor treatment and help weigh the benefits and risks of taking aspirin.

.jpg)
Is It Safe to Go Out to Eat?
Hungry for interaction after months of isolation, many are heading to restaurants now that many have reopened. But is it safe? Should you eat outside or is it safe inside? Here’s something you may have wondered: Can coronavirus be spread through food?
First – there’s no evidence that handling food or consuming food is associated with COVID-19. Coronavirus germs travel through respiratory droplets, so steer clear of anyone coughing or sneezing. You should also keep your distance – the standard six feet – from anyone who’s not living with you. If an infected individual is talking or laughing too close to you, you could be infected.
So, just how safe is it to eat at a restaurant? If you don’t want to take any risk at all, stick to home cooked meals. The fact is – there’s no such thing as “zero risk.” If you have an intense desire to have someone cook for you in an environment other than your home, go to a restaurant. The question becomes – how do you mitigate risk of exposure to COVID-19 when going out to eat? Following are a few suggestions.
Assess Your Risk
- Older people are at higher risk for severe illness from COVID-19.
- Those with underlying conditions – lung disease, diabetes, heart disease, obesity, or a compromised immune system – are particularly vulnerable.
- Consider how widespread the virus is in your community.
Do Your Homework/Be Prepared
- Call ahead to ask if servers and staff wear face coverings while on duty; ask if seating follows social distancing requirements; and find out what other adjustments the restaurant has made to their hours and safety practices.
- Self-park your car instead of using a valet.
- Bring a bottle of hand sanitizer, a packet of disinfecting wipes, and wear a face covering.
Opt for Outside
- Choose a restaurant that offers outside seating. There’s ample data that show the risk for transmission outdoors is lower than indoors.
- Consider a restaurant that has a large, open, outdoor seating area rather than a small patio surrounded by walls or fences. If you find the outdoor seating is cramped, consider taking your business elsewhere.
Read more tips for eating out.
Recap: 2020 Virtual Proton Conference
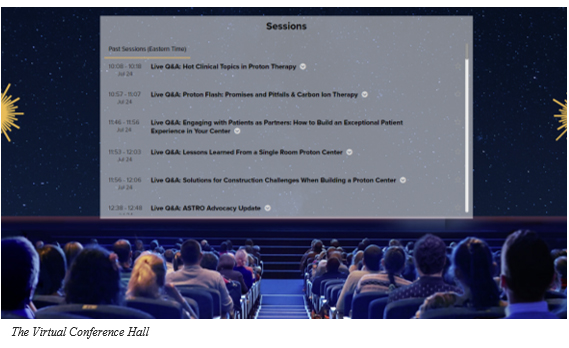
The eighth annual National Proton Conference, which was scheduled for April 26-29, 2020 in Nashville, TN, was canceled due to the coronavirus outbreak. After evaluating options, the team at the National Association for Proton Therapy (NAPT) decided to provide a one-day virtual conference on Friday, July 24, 2020, to ensure attendees didn’t miss out on access to the premier educational event for the proton therapy community. The robust agenda and interactive capability made the conference a valuable opportunity to access the latest information and resources in the proton world. Deb Hickey attended from her home in Medfield, MA. Her recap follows.
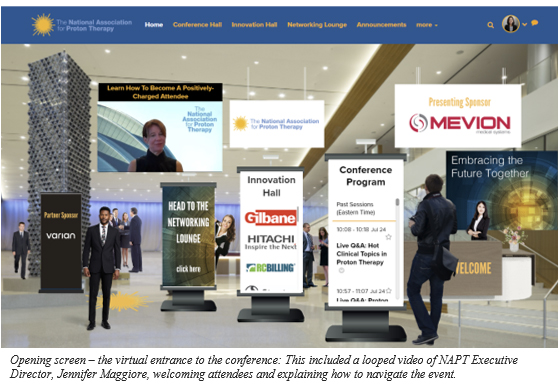
NAPT Executive Director, Jennifer Maggiore, Vice President of Marketing for Provision CARES Proton Therapy Centers and NAPT’s 2020 Conference Chair, Nancy Howard, and the rest of the conference planning committee did a superb job pulling a comprehensive, virtual conference together with less than three months to prepare. Although Deb missed shaking hands with her friends in the proton community, she was truly impressed and even excited as she logged in. She even made the “oooooh” sound out loud as she “entered the networking lounge” for the first time. The effects, the graphics, the music – it was professionally done, and Deb felt for a few minutes like she was actually in the room.
This year, there were 450 attendees at the live event, representing more than 50 cancer centers from 30 states, seven countries and eight time zones. Although we’re sure everyone missed meeting in person, the virtual space allowed the opportunity for a record number of attendees across the globe to engage with the proton therapy community in a truly unique way.
As usual, the following isn’t intended to be a comprehensive review of every presentation – to do that, we’d have to write a book. The following includes highlights from the conference that we think would be of interest and value to our members.
Opening Remarks
 Jennifer Maggiore began the day by welcoming attendees and reiterating NAPT’s mission to work collaboratively to educate and raise awareness of the clinical benefits of proton therapy, ensure patient choice and access to proton therapy, and encourage cooperative research and innovation, and then spoke about the challenges we’ve faced. An excerpt from her speech follows.
Jennifer Maggiore began the day by welcoming attendees and reiterating NAPT’s mission to work collaboratively to educate and raise awareness of the clinical benefits of proton therapy, ensure patient choice and access to proton therapy, and encourage cooperative research and innovation, and then spoke about the challenges we’ve faced. An excerpt from her speech follows.
NAPT was created from adversity and the proton community has always persevered in challenging times while making unprecedented progress in improving access to proton therapy for cancer patients. In the past few months, we’ve become more united than ever – we’ve faced reimbursement challenges, questions over the clinical benefits of proton therapy, and a global health crisis never seen before in our lifetime. And we’ve responded – collaborated, provided support, and become stronger through our efforts. The interest in proton therapy is strong and as the research increasingly supports the short- and long-term benefits of this treatment, more providers seek this technology and more patients seek this treatment. The voice of the proton community echoes the voice of cancer patients across the world who want precise treatment and the best quality of life.
Nancy Howard also provided opening remarks. She thanked Jennifer for her leadership and contributions and went on to thank participants and attendees. She explained how the virtual event was designed and what to expect throughout the day. She then introduced the keynote speaker, retired American figure skater and Olympic gold medalist, Scott Hamilton.
 Most are familiar with Scott – his sense of humor, the energetic way he entertained the crowd during his skating performances, and his signature move – the back flip. He also coined the phrase, “turning cancer upside down” and started the Scott Hamilton Cares Foundation, dedicated to changing the future of cancer by funding advanced, innovative research that treats the cancer while sparing the patient.
Most are familiar with Scott – his sense of humor, the energetic way he entertained the crowd during his skating performances, and his signature move – the back flip. He also coined the phrase, “turning cancer upside down” and started the Scott Hamilton Cares Foundation, dedicated to changing the future of cancer by funding advanced, innovative research that treats the cancer while sparing the patient.
Scott joyfully welcomed attendees to the conference and talked about his support for the proton therapy community. An excerpt from his presentation follows.
I was supposed to meet you all in Nashville, but things got turned upside down because of coronavirus. But that’s how it is for cancer patients when they learn they have cancer – their lives get turned upside down. I know – I’m a cancer and three-time pituitary brain tumor survivor. I’m also a husband and father of four. So, I need not only to survive, but thrive. I’m an advocate of proton therapy and I believe it’s a real solution for many cancer patients with tremendous benefits for quality of life … I support all of you who fight every day to deliver proton therapy to patients … I admire your passion and drive for cancer patients to have a choice and to have access to proton therapy and other treatment solutions that can kill the cancer and spare the patient harm. We can’t stop fighting.
Hot Clinical Topics in Proton Therapy
Proton Therapy and the Immune System
Ralph Vainer, MD, Ph.D., radiation oncologist at Cincinnati Children’s Hospital, explained how radiation can modify the immune response to tumors and enhance the activity of immunotherapy. He talked about the potential benefits of proton therapy on the immune response to tumors and the dangers of exposing circulating blood to radiation with conventional radiation.
Proton Therapy for Post-operative and High-risk Prostate Cancer
Curtiland Deville, MD, Associate Proton Director at the Johns Hopkins Proton Therapy Center, talked about proton therapy for post-operative and high-risk prostate cancer patients and the differences between proton therapy and IMRT for treating patients with recurrent prostate cancer after failed surgery. He revealed that post-prostatectomy proton beam therapy minimized low‐range bladder and rectal doses relative to IMRT.
Proton Therapy for Palliative Treatment and SBRT
Bree Eaton, MD, radiation oncologist at the Emory Proton Therapy Center reviewed the potential benefits of using proton therapy for palliative treatment and SBRT (Stereotactic Body Radiation Therapy). As radiation treatments can generally be divided into two categories – definitive/curative (standard, longer treatment courses designed to provide long-term tumor control with curative intent) and palliative (shorter treatments focused on improving or preventing tumor-associated symptoms in incurable situations) – proton therapy is used in less than two percent of all radiation treatments, and primarily as definitive treatment. According to Eaton, palliative treatment compromises 30-50 percent of radiation treatments, creating an opportunity for increased use of proton therapy to improve symptom burden for patients in the end of life. To improve tumor-associated symptoms such as pain, dyspnea, and bleeding, lower radiation doses and/or shorter treatment courses are needed. She went on to discuss the types of palliative radiotherapy – conventional and SBRT – and how proton could benefit both.
Proton Therapy Combined with Chemotherapy
James Metz, MD, Chair, Radiation Oncology at Penn Medicine explained the rational for combined modality therapy and the opportunity for proton therapy to reduce toxicity and hospitalizations when combined with chemotherapy. He reviewed the Bragg Peak, the similar biologic tumor-killing properties in protons and photons, and the markedly decreased dose to normal tissues and therefore potential to decrease side effects and complications using proton therapy. He explained how physicians can combine proton and other therapies safely, which often can’t be done with conventional radiation. He discussed a patient receiving radiation for rectal cancer detailing the difference between proton (left) and IMRT (right). In the image below, you can see significantly less dosage to normal tissues with proton therapy.
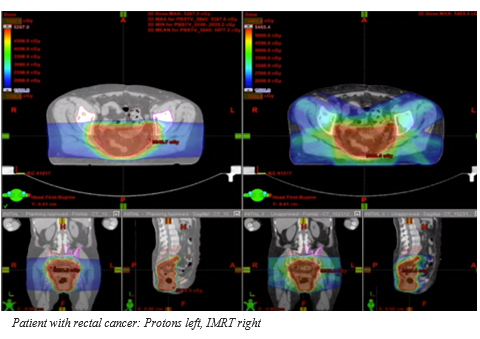
“More and more, definitive cancer treatment is moving to multimodality treatments,” said Metz. He explained that single-modality therapy has a high likelihood of success only in the earliest cancers and for specific cancers like prostate cancer. Most cancers, he said, need multimodality treatment to optimize patient outcomes.
Metz explained that combined modality therapy is done to treat the original tumor as well as distant, micro-metastasis. Radiotherapy primarily targets the local tumor while chemotherapy deals with both local and distant, micro-metastasis. Studies have shown that chemotherapy with radiation, while improving organ-preservation rates and survival, is almost always at the expense of increased toxicity when using conventional radiation.
Metz hypothesized that reducing the integral radiation dose will lead to reduced toxicity when protons are combined with chemotherapy compared to photons. He also hypothesized that a combination with radio-sensitizing chemotherapy would be easier with proton therapy with reduced normal tissue exposure and lead to improved performance status after treatment.
Impact of Medicare Payment Reform on Proton Therapy Practices
Last year, we informed our newsletter readers that the Center for Medicare and Medicaid Innovation (CMMI) had proposed a new payment model for radiation oncology services. The goal of the proposed alternative payment model is to increase the quality and value of radiation therapy received by Medicare beneficiaries; increase transparency in billing and payments; and hold down the overall growth in Medicare expenditures for radiation oncology. Basically, their goal is to decrease spending.
The Problem
The problem is this mandatory model for those on Medicare would result in beneficiaries receiving reimbursement for proton therapy at the same national base rate as all other radiation modalities (including IMRT and brachytherapy). To be clear, Medicare is proposing a huge change to their coverage for proton therapy—and it’s not good. If this new proposed rule is approved, Medicare will no longer cover proton therapy as it has in the past. Rather, it will cover the same amount for proton as it does for any other radiation treatment, reducing coverage levels by roughly 50 percent.
Mark Waddle, MD, assistant professor in the department or radiation oncology at Mayo Clinic, discussed the proposed model and its potential impact on clinical practice, focusing specifically on proton therapy practices. He noted that in a report to Congress, the Centers for Medicare and Medicaid Services (CMS) had claimed proton therapy was “low value care” meaning it provided little benefit to patients and incurred unnecessary cost. In the report, proton therapy reimbursement was shown to have doubled in the past few years, with about 46 percent of treatment volume for prostate cancer. CMS cited an ICER report from 2014 that noted proton therapy was comparable with alternative radiation treatments for prostate, lung, and liver cancer, citing a low quality of evidence.
Dr. Waddle explained that radiation oncology witnessed a rapid increase in innovation and technology, which resulted in improved care for patients, but this also increased Medicare spending. As a result, those in the radiation oncology field are the focus of increased scrutiny. Expectations exist that any new technology should be cost neutral or demonstrate a clear, clinical result that justifies increased cost.
So How Will the Proposed Model Impact the Use of Protons?
According to Waddle, the financial impact may be significant. Because there’s a reduction in reimbursement of photon radiation by 5-25 percent, proton will likely be affected to a greater degree due to higher capital expenses. This has the potential to create financial strain for practices and may ultimately limit access to proton therapy.
Advocacy Efforts
Waddle noted the significant advocacy efforts over the past few months to modify reimbursements, make participation elective, and to remove proton therapy. Late last year, we asked you – our members – to contact congressional leaders through email, letters and phone calls asking them to reconsider the new model and the response was overwhelming. Waddle mentioned the efforts were well received by CMS and he’s hopeful positive changes will be made for the final model. Note the release date for the model was Jan. 1, 2020, but due to unforeseen circumstances, that date has come and gone. It’s still unclear when the final model will be released and what it will look like.
Using ERISA in Proton Therapy Insurance Appeals
Tim Rozelle, an associate attorney at Kantor and Kantor, LLP, provided a comprehensive presentation on ERISA (Employee Retirement Income Security Act) health benefit denial issues. He explained that ERISA governs all types of employee benefits – including health benefits. To explain how ERISA doesn’t work, Tim described a jury trial where there are 12 jurors in a box deciding the final decision after hearing multiple arguments. Under ERISA, if a patient files litigation, his juror is the judge, and typically, a case is decided based on what’s inside an administrative record.
The Importance of the Administrative Record
An administrative record contains all the paperwork, denial letters, the appeals developed by the patient or the healthcare provider or both. It contains supportive, scientific journal articles and other up-to-date materials. It includes all the rationales for why the treatment should be approved. It’s the package the judge will use to make his decision and therefore, it’s extremely important.
Note that under ERISA, the judge determines whether he thinks the denial decision is reasonable. Keeping this in mind, when compiling your administrative record, consider how you can present that the insurance company’s denial is unreasonable.
Tim then described, in detail, how to build the key components of the administrative record. Specifically, he discussed his experiences in developing appeal letters – what he learned and how they’ve changed. He talked about the different types of denials including an increasingly more common reason that “proton is equally as effective as IMRT, but not cost-effective because IMRT is a less-costly alternative.”
The Third-party Review Process
Tim also talked about the external third-party review process. He shared his opinion that an external third-party review isn’t always the best option because they typically end up being negative and the result is if you go to litigation, an insurance company attorney will “highlight, promote, and hone in on the fact that a third-party reviewer supported the denial.” So, you may not want to give the insurance company the opportunity to say that an external, third-party reviewer agreed with their decision.
Peer-to-peer Calls
Finally, Tim discussed peer to peer calls. These calls – which are outside the scope of an appeal letter – are typically between the healthcare provider and the insurance company medical reviewer. He suggested the healthcare provider participate in these calls and document everything – the time, place, manner of communication, what was said, what wasn’t said, how long the call lasted, confirmation that the medical reviewer had the full record and information in front of her for the call, and whether there were any missed calls or emails from the medical reviewer.
Interestingly, Tim mentioned that many times, the medical reviewers on these calls aren’t qualified to be rendering denial decisions. In some instances, the calls end up becoming “a sham” because they’re not substantively discussing the issues and they’re not individually reviewing an individual patient’s record. Instead, the medical reviewer is making a blanket determination and applying blanket guidelines. Tim recommends healthcare providers place their notes from these calls in the patient’s appeal letter and in the administrative record.
What is a Class Action?
After a patient has exhausted all levels of appeal, he has the option to bring legal action. One way to do this is with a class action lawsuit. Stephanie Casey, a litigation lawyer with Colson Hicks Eidson, provided a presentation on this topic. She began by explaining the difference between an individual lawsuit and a class action lawsuit. In an individual lawsuit, one plaintiff files a case against a defendant. In a class action lawsuit, there’s a class of plaintiffs (policyholders) who sue a defendant (health insurance company). Typically, with a class action, there’s a class representative – one plaintiff that represents a group of unnamed individuals with similar issues/complaints.
Benefits of a Healthcare Class Action
- Provides restitution to plaintiffs who’d otherwise receive nothing because of attorney costs
- Reduces the cost of litigation
- Motivates defendants to settle since there are many plaintiffs
- Potential to achieve change in healthcare policy that affects many others
Proton Therapy Class Actions Pending
Stephanie mentioned seven proton therapy class actions pending across the country, all governed by ERISA except one. They challenge the uniform application of medical policies that were designed to allow the insurance company to deny proton therapy claims. They’re seeking retraction of categorical denials of coverage of proton; they ask that the insurance company reevaluate all prior claims; and they ask for reimbursement to patients that paid out of pocket.
Non-ERISA Litigation
There are several other types of litigation including FEHBA, the Federal Employees Health Benefits Act, Medicare, and litigation under state law. Rich Collins, a trial attorney at Callahan and Blaine, described each of these in detail.
Proton FLASH Therapy
Dr. Ricky Sharma, MD, PhD at Varian Medical Systems, talked about FLASH therapy – ultra-high dose rate radiotherapy that uses electrons to minimize healthy tissue damage while targeting tumors. He expressed his excitement over the technology and the reason it’s one of the hottest topics in radiation oncology – it’s able to increase normal tissue sparing compared to conventional dose rate and the tumor control is equivalent or better than conventional dose rate. However, he noted, electron FLASH is limited in depth to a maximum of about three centimeters which limits its use in treating cancer. So, Varian developed a way to deliver ultra-high dose rate FLASH therapy with protons that can reach much deeper within the body.
The team at Varian recently completed their first preclinical mice trial with proton FLASH. Results showed improved survival and reduced skin toxicity. This was the first indication that the published results with electron FLASH could be reproduced with proton FLASH. The technology will continue to be developed.
Summary
The take-away from this year’s conference is that the proton therapy community has faced extreme challenges over the past year, but we’ve persevered and made extraordinary progress in advancing proton technology and improving access to proton therapy for cancer patients. We will continue to fight for proton therapy, and hope to meet face to face with others in the proton community at NPC 2021.

Where Your Money Goes
Where does your money go when you make a contribution via the Robert Marckini Chair for Proton Research at Loma Linda University Health? Many think it goes directly to help others who’ve been diagnosed with prostate cancer and they’re right. What you may not know is that your contributions are also used to further proton therapy research in general, helping patients suffering from other types of conditions including breast cancer, lung cancer, acoustic neuroma, chondromas and chondrosarcomas, meningiomas, arteriovernous malformations, isolated brain metastases, pituitary ademas, uveal melanomas, nasopharynx, oropharynx, sarcoma of the paranasal sinuses, parameningeal rhabdomyosarcomas, and other pediatric conditions.
Loma Linda researchers have six active clinical trials including trials for esophageal cancer, liver metastases, soft-tissue sarcomas, early stage breast cancer and newly diagnosed glioblastoma. As you know, Loma Linda, along with more than 40 other treatment facilities across the country, are also recruiting prostate cancer patients for the COMPPARE trial, comparing the quality of life, side effects, and cure rates for prostate cancer patients treated with proton therapy or photon therapy.
Every dollar you give helps someone in need – even just $25 a month. Please help Loma Linda University Health obtain the funds they need to continue their life-saving research. When you donate, you join a century-long legacy of faith and innovation in healthcare, education, research, and wellness.
Give to Proton Therapy Research
- Donate online.
- Write a check to LLUCC Proton (Put “Marckini Chair” on the memo line) and mail to LLUH, Office of Philanthropy P.O. Box 2000, Loma Linda, CA 92354.
- Call Regina Joseph at 909-558-5010.

Why is 98.6° Fahrenheit Considered Normal Body Temperature?
WebMD reports that 98.6° F is considered a normal body temperature and any temperature above 100.4° is considered a fever. In fact, for a typical adult, “normal” body temperature can be anywhere from 97 to 99° F. Babies and children have a slightly higher range for normal: 97.8 – 100.4° F. Any temperature above 100.4° F is considered a fever for adults and children. But why? The answer can be found in the June 28, 2020 issue of Parade Magazine in the Marilyn vos Savant column.
As it turns out, most of the world uses the Celsius system for temperature measurement. Only a few countries use Fahrenheit as their official scale: the U.S., Belize, Palau, the Bahamas, and the Cayman Islands.
And, for most of the rest of the world, normal body temperature is 37° C, while a fever is any temperature over 38°C. Fahrenheit, 37° C is 98.6, and 38° C is 100.4.

.jpg)
Useless Facts
- Snails can sleep up to three years.
- Most lipstick contains fish scales.
- Hudson Bay area in Canada had less gravity than the rest of the world and scientists don’t know why.
- Only one to two percent of the world population are natural redheads.
- Diamonds don’t show up on X-ray.
- Scorpions can hold their breath underwater for up to six days.
- Your cellphone carries up to 10 times more bacteria than a toilet seat.
- Humans and bananas share about 50 percent of the same DNA.
- A human has fewer chromosomes than a potato.
- Hot water can turn to ice faster than cool water.
- Statistically, you’re more likely to die on the way to buy a lottery ticket than you are to win the lottery.

Last Month’s Brain Teaser
Three men are walking across a green and luscious field. Only two of them are wearing rubber boots and yet the feet of the third man remain dry. Why? (Think hard.)
Answer: The field was dry.
Winner: BOB member Jim Pennington of Towanda, KS is last month’s brain teaser winner. Jim was pleasantly surprised to learn he’d won the contest. In an email to Deb, he wrote, “There’s no way either you or your father could know how many lives you’ve affected – the two of you are very much appreciated.” Jim went on to say Bob’s book was the “major reason” he chose proton therapy nine years ago and he’s never once regretted his decision.
 Jim sent us a photo of him and his wife Glenis, and reminded us they’re likely the only couple to simultaneously undergo proton therapy at Loma Linda University Cancer Center – he was treated for prostate cancer while she was treated for breast cancer. “Neither of us has experienced another sign of cancer,” he assured us.
Jim sent us a photo of him and his wife Glenis, and reminded us they’re likely the only couple to simultaneously undergo proton therapy at Loma Linda University Cancer Center – he was treated for prostate cancer while she was treated for breast cancer. “Neither of us has experienced another sign of cancer,” he assured us.
The COVID-19 pandemic has put a halt to most of Jim and Glenis’ normal activities. And their home is “in the woods,” so they’re isolated from friends and family. “Although we miss seeing our grandkids and square dancing with friends, it’s beautiful and quiet here,” said Jim. “We bucket garden a little and feed the birds, rabbits, deer, and turkeys just enough that they come by regularly.”
Congratulations, Jim! Your signed copy of Bob Marckini’s new book is in the mail.

.jpg)
New Brain Teaser/Riddle
You see a boat filled with people. It hasn’t sunk, but when you look again you don’t see a single person on the boat. Why?
Send your answer to [email protected] for a chance to win a signed copy of Bob Marckini’s NEW second edition book, You Can Beat Prostate Cancer.

.jpg)
Signs
A sign in a shoe repair store reads: “We will heel you. We will save your sole. We will even dye for you.”
A sign on a blinds and curtain truck: “Blind man driving”
On a septic tank truck: “Yesterday’s Meals on Wheels”
At an optometrist’s office : “If you don’t see what you’re looking for, you’ve come to the right place.”
On a plumber's truck: “We repair what your husband fixed.”
At a tire shop: “Invite us to your next blowout.”
On a maternity room door: “Push. Push. Push.”
In a veterinarian’s waiting room: “Be back in 5 minutes. Sit! Stay!”
In the front yard of a funeral home: “Drive carefully. We’ll wait.”

Quote of the Month: "Age is merely the number of years the world has been enjoying you." —Unkown


Great Quotes from the “Peanuts” Comic Strip
On Oct. 3, 1950 the cartoon, “Peanuts,” first appeared in seven newspapers. The cartoon ran for nearly 50 years and was published in 2,600 newspapers in 75 countries and 21 languages. Following are some Charlie Brown, Snoopy, Linus, Schroeder, Lucy, Woodstock, Pig Pen, Rerun, and Sally Brown quotes from the creative genius, Charles Schulz.
“Worrying won’t stop the bad stuff from happening. It just stops you from enjoying the good.”
“A good laugh and a long sleep are the two best cures for anything.”
“I don’t have time to worry about who doesn’t like me – I’m too busy loving the people who love me.”
“Perhaps they are not stars in the sky, but rather openings where our loved ones shine down to let us know they are happy.”
“The less you respond to rude, critical, argumentative people, the more peaceful your life will become.”
“Definition of a friend: Someone who says nice things about you when you aren’t around.”
“When my arms can’t reach people who are close to my heart, I always hug them with my prayers.”
“There are moments in life when you miss someone so much that you just want to pick them from your dreams and hug them for real.
“All you need is love. But a little chocolate now and then doesn’t hurt.”
Bob Marckini and Deb Hickey
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
NO MEDICAL ADVICE: Material appearing here represents opinions offered by non-medically-trained laypersons. Comments shown here should NEVER be interpreted as specific medical advice and must be used only as background information when consulting with a qualified medical professional.