Dear Members (a note from Deb Hickey):
This month’s issue is a very special one.
We’re honored to share a personal message written exclusively for our members by Dr. Richard Hart, president of Loma Linda University Health (LLUH). In it, he announces something extraordinary: Loma Linda University Cancer Center is pioneering four revolutionary cancer treatments at its Loma Linda, California, campus. To our knowledge, it is the only medical center in the world advancing all four of these leading-edge cancer therapies:
- CAR-T cell therapy
- Theranostics
- Boron Neutron Capture Therapy (BNCT)
- Proton FLASH Therapy
These treatments aren’t just incremental improvements—they represent a new era of cancer care. From delivering a complete radiation therapy treatment in a single dose in just a few nanoseconds (that’s billionths of a second), to harnessing a patient’s own immune cells to attack once-incurable cancers, to pairing imaging with targeted treatment at the molecular level, to destroying tumors from within while sparing healthy tissue—these innovations are already transforming what’s possible for patients facing the toughest diagnoses. They’re also at the heart of LLUH’s Stronger Together campaign—a bold effort to expand access to these groundbreaking therapies and ensure more patients benefit from them today and in the years to come.
This is also deeply personal for me.
In 2014, my husband, Mark, was diagnosed with metastatic pancreatic neuroendocrine cancer. We were told it was incurable and terminal—he was given three to six months to live. The only option offered at the time was an outdated chemotherapy protocol, which, if successful, might give him a few more weeks or months.
By God’s grace and for reasons his doctors still can’t explain, Mark was declared “disease-free” a few months later.
What gives me chills these days—and in the best way—is knowing that if his cancer were ever to return, theranostics—coincidentally, a therapy first tested in neuroendocrine cancers—would now be available to him. That reality allows me to fully breathe again, knowing the world has changed so much since that absolutely earth-shattering time in our lives. It’s this kind of progress—and the hope and peace it brings—that Dr. Hart highlights in his letter.
As we near the end of the year, Dr. Hart’s message is a timely reminder of one of the greatest reasons our community exists: to support innovation that truly changes lives. Our members were privileged to receive proton therapy—something not within reach for everyone due to cost, geography, or lack of awareness. It’s important to remember that LLUH pioneered proton therapy in the hospital setting—without that bold leadership, the other 45 proton centers in the U.S. may not exist today, and our members might not have had access to this life-changing treatment.
Many of you choose this time of year to consider annual gifts, and Dr. Hart’s message underscores how such generosity supports both LLUH’s groundbreaking history and its ongoing efforts—helping bring tomorrow’s cancer treatments to more patients today. Personally, I can’t think of a more meaningful reason to give.
I encourage you to read Dr. Hart’s letter carefully. His words describe not just scientific progress, but a true turning point in how cancer will be treated going forward. These advancements are awesome—in every sense of the word.
Now, in honor of my husband’s incredible survival and what it continues to mean to our family, I’m proud to share a photo of him with his recently completed oil painting—an impressive 5-by-6-foot depiction of the iconic musician Jimi Hendrix. Created in a mosaic-style technique (known as “pixel painting”) using 1-by-1-inch squares (4,320 of them!), the painting may appear blurry at first glance, but once you step back, the image comes into striking focus. To give you a better sense of how it works, you can watch a short video that zooms in on the squares and then steps back to reveal the full painting.
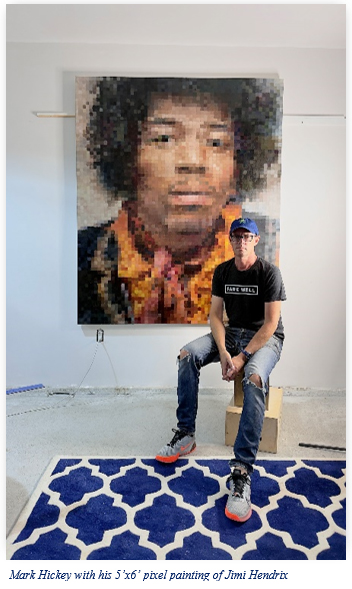
Mark began this project last July—exactly 11 years after his oncologist silently turned the computer monitor toward us. I stared at the scan, confused, and finally said, “I don’t see the cancer. Where is it?” Without a word, he raised his hands in a gesture that said it all.
In addition to the special information from Dr. Hart, this month’s BOB Tales includes a mix of research updates, inspiring stories, and practical health tips. In our News Report section, we cover Artificial Intelligence and machine learning breakthroughs that improve early detection, new insights on statins for men with advanced disease, ongoing debates about PSA screening, and promising complementary therapies like acupuncture for urinary symptoms.
Our Flashback Article revisits a 2020 Stanford study showing that proton therapy dramatically reduces the risk of second cancers, highlighting its long-term benefits.
Our Health section offers practical tips for proactive living, from heart health and the coronary artery calcium scan to sunlight for cellular energy, and a simple, nutrient-packed snack that can power your workouts and boost overall vitality. And much, much more.
As always, we welcome your feedback! Just write to [email protected].
Deb Hickey
📄 Prefer to print and read?
👉 Download the PDF here.

Special Segment:
News Report:
- AI Detects Early Prostate Cancer in More Than 80% of Missed Samples
- MicroRNA + Machine Learning Improves Prostate Cancer Detection
- Statins Show Promise for Men with Advanced Prostate Cancer
- Caught Early or Overtreated? The PSA Debate
- Acupuncture May Reduce Nocturia for Prostate Cancer Survivors
Flashback:
Health:
- A Simple Test That Could Save Your Heart—And Your Life
- The Hidden Power of Sunlight: Improve Vision and Vitality
- The Perfect Pre-workout Snack

From the President: Shaping the Future of Cancer Care
We're honored to share a personal message written exclusively for our members by Dr. Richard Hart, president of Loma Linda University Health. In it, Dr. Hart announces something extraordinary: Loma Linda University Cancer Center is likely the only cancer center in the world to unite four of the most advanced cancer therapies under one roof. These include proton therapy (featuring next-generation FLASH technology), CAR-T cell therapy, theranostics, and boron neutron capture therapy (BNCT).
The Future of Cancer Care at Loma Linda University Health
Written by Richard H. Hart, MD, DrPH
Today we stand at a new threshold. Just as many years ago we stepped out in faith with the opening of the world’s first hospital-based proton treatment center, we now envision the next era of cancer care—one that brings together the four most advanced treatment modalities in the world and that will be available together only in one place—here at Loma Linda University Health.
At Loma Linda University Health, we approach cancer care through a collaborative, multidisciplinary team of experts that works together to ensure each patient receives the most advanced and personalized treatment possible. Our teams of physicians, researchers, nurses, and support staff unite their expertise to treat not just the disease, but the whole person.
Guided by both leading-edge science and unwavering faith, we will build upon our history of innovation that has transformed cancer care while continuing to look toward the future with hope and determination.

Proton Therapy
In 1990, Loma Linda University Health made history by opening the world’s first hospital-based proton treatment center. That bold step, rooted in faith and scientific vision, forever changed the way cancer could be treated. Since then, thousands from around the globe have come to Loma Linda, seeking not only advanced medicine but also compassionate, whole-person care.
Proton therapy has already transformed cancer care by delivering radiation with remarkable precision. Now, FLASH proton therapy takes that one step farther by delivering the dose in a fraction of a second. While most proton centers do not yet have the capability to deliver FLASH due to the highly specialized technology required, Loma Linda University Health has the unique capability to investigate its potential use across many cancers. Early studies have shown promise, and we are excited to once again be involved at the leading edge of proton therapy research. We are expecting to be offering this to patients in 2028.
“Our leadership in proton therapy has been an important part of our legacy of cancer treatments since we opened the first proton accelerator used in a medical environment in 1990,” said Dr. Jerry D. Slater, chairman of the department of radiation medicine, Loma Linda University Health. “Thousands of cancer patients have undergone successful proton therapy in the decades that followed. FLASH proton technology will be an important advancement in our cancer proton treatment options, one that has the potential to offer reduced side effects, enhanced tumor control, and shorter treatment durations.”

CAR T Cell Therapy
CAR T cell therapy marks a groundbreaking advance in personalized cancer treatment—reprogramming a patient’s own immune cells to recognize and destroy cancer. In April 2024, Loma Linda University Cancer Center introduced this cutting-edge therapy, becoming one of the first with a single program to offer it for both children and adults—a development that brings revolutionary hope to those who seek our care.
CAR T cell therapy is only one of the many exciting cell therapies to treat cancer that are being researched, developed, and introduced at LLUH. Others include T Cell Receptor (TCR) Therapy, Tumor Infiltrating Lymphocyte (TIL) Therapy, Natural Killer (NK) Therapy, and gene therapy. These cell therapies are particularly exciting because they hold the promise to expand the precision and power of cell therapy beyond hematologic cancers to solid cancers. We are building a cell-manufacturing lab that will allow us to move these exciting therapies directly from the laboratory to patient care.
“The availability of immune cellular therapy at Loma Linda University Cancer Center will vastly improve care for many people who are battling cancers,” said Dr. Mark Reeves, Director of the Cancer Center.
Dr. Hisham Abdel-Azim, Division Head of Transplant and Cell Therapy, emphasized the treatment’s transformative potential: “CAR T therapy represents a remarkable and truly revolutionary advancement in cancer treatment. By modifying a patient’s immune cells to target cancer, we see high rates of success in curing patients who had limited treatment options. The good news is that CAR T cell therapy is often a one-time treatment, providing hope for patients with relapsed or refractory cancers.”
By combining cutting-edge science with compassionate, comprehensive care, our center is giving families hope, transforming outcomes, and redefining what is possible in the fight against cancer.
Theranostics
Theranostics combines therapy and diagnostics into a single approach that changes how we see and treat cancer at the cellular level. Using radioactive tracers, physicians can locate cancer cells with imaging, and then target those same cells with therapeutic doses delivered directly to the tumor cells. This precision reduces exposure to healthy tissues while increasing effectiveness. Already showing success in prostate and neuroendocrine cancers, theranostics is rapidly expanding into new applications.
Importantly, theranostics can also provide a second line of defense in treating micro-metastases, making it especially valuable when prostate cancer and other types of cancer have already spread. At Loma Linda University Cancer Center, this technology is now available and will give patients access to personalized treatments designed around the molecular biology of their disease. In addition, we are building a radiopharmacy that will allow us to move these exciting therapies directly from the laboratory to patient care.
“Theranostics represents a remarkable step forward in how we diagnose and treat cancer,” said Dr. Eric Peters, Chief of Nuclear Medicine at LLUH, “by pairing imaging with targeted therapy, we can see and treat cancer at the molecular level, offering our patients treatments that are more precise, more effective, and more personal than ever before. This approach is transforming cancer care today and opening the door to breakthroughs we once only imagined.”
Boron Neutron Capture Therapy (BNCT)
BNCT is one of the most promising therapies under development for hard-to-treat cancers. Patients receive a boron-based drug that accumulates in tumor cells. When exposed to a beam of neutrons, the boron atoms react and release energy that destroys the cancer from within—while sparing healthy tissue.
BNCT holds great promise for recurrent head and neck cancers, glioblastomas, and melanomas, which often resist conventional therapies. Few centers in the world are exploring this frontier, and Loma Linda University Cancer Center is uniquely positioned to be one of the first to bring BNCT to patients in the United States. We anticipate this therapy being available within the next 3-to-5 years.

Carrying the Legacy Forward
The story of cancer care at Loma Linda University Health has always been one of courage, vision, and faith. In 1990, we launched a bold initiative of opening the proton treatment center that has since treated thousands of patients. With the support of the Brotherhood of the Balloon throughout the years, what began at Loma Linda University Health grew into a global movement in cancer treatment.
Now, 35 years later, we’re preparing to unite FLASH proton therapy, CAR T cell therapy, theranostics, and BNCT under one roof, creating a cancer program unlike any other.
Once again, Loma Linda University Health is uniquely poised to lead the world in transforming how cancer is treated—not only through the most advanced science, but also through our enduring commitment to treating the whole person, guided by faith and compassion, fulfilling our mission to bring hope and healing to every patient.
“We are focusing on cancer therapies that are incredibly precise and are giving early signals of truly being game-changers. By developing these therapies at LLUH, together with our prior experience in introducing ground-breaking cancer therapies, we think there will be even more profound synergies between these therapies that will truly change our ability to destroy cancer while allowing people to live well,” said Dr. Reeves.
We invite you to be part of this vision. Your gift can accelerate the development of these groundbreaking treatments and expand access for patients in need. Together, we can honor the legacy of the past and transform the future of cancer care.

Support Stronger Together
- Online: Donate here. From the pull-down menu, choose “Cancer Center Vision/Stronger Together Campaign.
- By Check: Make your check out to “LLUCC.” Write “Stronger Together” on the memo line.
Mail to: LLUH, Office of Philanthropy P.O. Box 2000, Loma Linda, CA 92354. - By Phone: Call Regina Joseph at 909-558-5010.

AI Detects Early Prostate Cancer in More Than 80% of Missed Samples
A groundbreaking study from Uppsala University in Sweden reveals that artificial intelligence (AI) can identify early prostate cancer in tissue samples previously deemed healthy by pathologists. The research demonstrates that AI detected subtle tissue changes indicative of cancer in more than 80% of samples from men who later developed aggressive prostate cancer.
The study involved 232 men whose biopsies were initially assessed as negative. Over time, half of these men developed aggressive prostate cancer, while the other half remained cancer-free. AI analysis of their tissue samples revealed patterns that human pathologists had overlooked, highlighting the potential of AI to uncover early signs of cancer before they become visible to the human eye.
“The study has been nicknamed the ‘missed study,’ as the goal of finding the cancer was ‘missed’ by the pathologists. We have now shown that with the help of AI, it is possible to find signs of prostate cancer that were not observed by pathologists in more than 80% of samples from men who later developed cancer,” said Dr. Carolina Wählby, Professor of Quantitative Microscopy.
This development underscores the growing role of AI in enhancing diagnostic accuracy and improving patient outcomes in prostate cancer care.

MicroRNA + Machine Learning Improves Prostate Cancer Detection
Researchers in India are also using AI in prostate cancer detection—specifically, a machine learning approach combined with a new blood test that profiles microRNAs (miRNAs). MiRNAs are tiny molecules in the blood that act like messengers controlling gene activity, and their patterns can reveal whether cancer is present.
Machine Learning vs AI: Machine learning (ML) is a type of artificial intelligence (AI) that learns patterns from data to make predictions. In this study, ML was trained on blood biomarkers (miRNAs) to distinguish prostate cancer from benign conditions. Unlike “AI” in the movies, it doesn’t think—it analyzes data and finds patterns humans might miss.
The study, conducted at the Institute of Medical Sciences, Banaras Hindu University, identified three key miRNAs—miR-21-5p, miR-141-3p, and miR-221-3p—that were most useful in distinguishing prostate cancer from non-cancerous prostate conditions. By feeding these miRNA levels into a machine learning model, researchers were able to correctly predict cancer in about three-quarters of cases—significantly outperforming standard PSA tests.
Certain ratios between the miRNAs were particularly predictive, reflecting real biological pathways linked to cancer.
This approach could eventually lead to a non-invasive, blood-based test that reduces unnecessary biopsies while improving early detection, though larger studies and standardization are needed before it can be widely adopted in clinics.

Statins Show Promise for Men with Advanced Prostate Cancer
A new study sheds fresh light on how common medications—statins for cholesterol and cardiovascular disease and metformin for Type 2 diabetes—may influence outcomes in men with prostate cancer.
Using data from a massive French national database, researchers from the University of California, San Francisco, analyzed records from more than half a million men, making this one of the most comprehensive real-world studies to date. What makes it particularly noteworthy is that the study breaks down results by treatment type, highlighting a connection between statin use and survival in men receiving androgen deprivation therapy (ADT) for advanced disease.
Breaking Down the Findings
Metformin alone did not improve survival, indicating that men with diabetes remain at higher risk of worse outcomes, even when treated with standard therapy. Statin use, on the other hand, was linked to better survival for men on ADT, with the strongest benefit observed in men taking both statins and metformin. By contrast, among men treated with radical prostatectomy, neither statins nor metformin showed a survival advantage.
The connection with ADT makes this particularly compelling. Previous studies had hinted at a potential protective effect of statins against prostate cancer, likely due to cholesterol-lowering, anti-inflammatory properties, or synergy with hormone therapies. This new research confirms that statins’ benefit is most pronounced when paired with ADT, a first-line treatment for advanced prostate cancer. For many clinicians and patients, this is unexpected, since statins are typically thought of solely as heart medications.
What This Means for Patients and Doctors
This large-scale, real-world study strengthens evidence that statins may support men receiving ADT, while also highlighting that diabetes remains a significant risk factor and metformin alone cannot fully offset its impact. By separating outcomes by treatment type, the research provides actionable insights for personalized care and underscores the importance of considering both cancer and comorbid conditions when developing treatment strategies.

Caught Early or Overtreated? The PSA Debate
Prostate cancer remains the second-leading cause of cancer death in men, yet screening is still a controversial topic. PSA testing can save lives by detecting cancer early, but it’s not perfect—false positives, unnecessary biopsies, and overtreatment are real risks.

Recent research shows that even men whose biopsies reveal no cancer can experience lasting regret, often due to the discomfort, bleeding, or stress of the procedure. In the U.S., only about 38% of men aged 50–64 were screened in 2023, leaving many at risk of advanced disease.
Non-invasive treatments and precision approaches, like proton therapy, are part of ongoing efforts to improve outcomes and reduce treatment-related side effects.
Experts emphasize that informed decision-making and personalized screening strategies are essential. By carefully assessing individual risk factors, physicians aim to detect cancers early while minimizing unnecessary procedures and stress for patients.

Acupuncture May Reduce Nocturia for Prostate Cancer Survivors
A pilot study conducted at Memorial Sloan Kettering Cancer Center in New York explored whether acupuncture could help reduce nocturia—a common and frustrating side effect in men treated for prostate cancer that causes frequent nighttime urination. The study enrolled 60 men who reported waking at least twice each night to use the bathroom.
Half of the participants received 10 weekly acupuncture treatments, while the other half continued with their usual routines and symptom management strategies.
Those in the acupuncture group experienced a noticeable reduction in nighttime bathroom trips—both immediately after treatment and again one month later. They also reported improved overall urinary function.
This research adds to the growing body of evidence supporting acupuncture as a complementary therapy for prostate cancer survivors dealing with urinary symptoms. However, larger studies are needed to confirm these promising findings.
We’ve been publishing BOB Tales for nearly 25 years, sharing thousands of articles—many of which our newer members haven’t seen, and longtime members may have forgotten or would appreciate revisiting. That’s why we regularly reprint articles from past issues that we believe are still relevant and carry an important message. The following is an abstract from an article we first shared in our September 2020 issue.
Proton Therapy Dramatically Cuts Risk of Second Cancers, Stanford Study Finds
A recent study published by the American Cancer Society investigates whether the type of radiotherapy used in primary cancer treatment affects patients’ risk of developing a second, distinct cancer later on. The researchers looked at three common forms of treatment:
- 3D Conformal Radiotherapy (3DCRT)
- Intensity-Modulated Radiotherapy (IMRT)
- Proton Beam Radiotherapy (PBRT)
Both the 3DCRT and the IMRT utilize Photon (X-Ray) radiation, while PBRT utilizes Proton radiation, which is what our members have received.
Study Scope and Patient Pool
The study drew on data from the National Cancer Database, focusing on patients—including both children and adults—who were first diagnosed with cancer between 2004 and 2015. In total, the analysis included 450,373 patients, who were treated using one of the three radiotherapy methods. These patients spanned nine types of cancer, including head and neck, gastrointestinal, gynecologic, lymphoma, lung, prostate, breast, bone/soft tissue, and brain/CNS cancers.
The researchers tracked outcomes over a median of 5.1 years after radiotherapy completion.
Key Findings
-
IMRT vs. 3DCRT:
There was essentially no difference in the risk of developing a second cancer between patients treated with both forms of X-Ray radiation: IMRT and 3DCRT
-
PBRT (Proton Therapy) vs. IMRT:
Patients receiving proton therapy had a significantly lower risk of a second cancer compared to those treated with IMRT. At 5.1 years median time interval, the risk with protons was 70% lower.
Results held consistent across the whole range of cancer types, including prostate cancer.
Why This Matters
This large-scale analysis provides strong evidence that proton beam radiotherapy can significantly reduce the long-term risk of developing a second primary cancer, compared to conventional X-Ray (photon-based) approaches like IMRT or 3DCRT.
But here’s the kicker: According to the American Cancer Society, while secondary blood cancers can appear two to 10 years after primary radiation treatment, solid tumor secondary cancers can appear 10 to 40 years later. If proton therapy shows a 70 percent benefit after only five years, one would expect the secondary cancer protection of proton therapy to be even more beneficial over a longer time period.
BOB Comment: In our Flashback section, we typically don’t revisit articles from fewer than 15 years ago, but we feel this 2020 Stanford study is a landmark in showing one of proton therapy’s most important benefits—dramatically reducing the risk of second cancers. The findings are particularly striking because they come from a massive, real-world dataset of over 450,000 patients across all ages, tumor types, and genders. Even compared with modern photon techniques like IMRT, the reduction in second malignancies with proton therapy was remarkable—less than a third the rate. For patients weighing treatment options, this study underscores why proton therapy is not just a highly precise form of radiation, but one that can have lasting, life-protecting implications.

A Simple Test That Could Save Your Heart—And Your Life
Heart disease is the leading cause of death for men in the U.S., and age is a major risk factor. Men over 40, especially those with a history of chronic conditions or prior serious illnesses, should be proactive about their heart health.

A quick, painless test—the Coronary Artery Calcium (C.A.C.) Scan—measures calcium deposits in your coronary arteries and produces a personalized score that reflects your heart disease risk:
- 0: No plaque; risk may be lower than expected
- 1–100: Some plaque; discuss preventive steps with your doctor
- 100–300+: Higher risk; treatment may be recommended
Your Heart, Your Call
Many men hesitate to start cholesterol-lowering medications like statins. Some worry about side effects, others feel healthy enough without medication, and some hope lifestyle changes alone will be enough. A C.A.C. scan can take the guesswork out of the decision. Seeing actual plaque in your arteries can motivate treatment—or reassure you if your score is zero. Statins are effective, widely available, and generally safe, but many avoid them due to exaggerated fears.
So why isn’t the C.A.C. test more common? Despite its benefits, it’s underused due to cost (usually $100–$300, rarely covered by insurance), lack of awareness, and absence of large-scale clinical trials—though recent studies show promising results.
Is the Test Right for You?
The C.A.C. scan is most helpful for people without a history of heart disease—those who haven’t had a heart attack or stroke, don’t currently have symptoms, and aren’t already at very high or very low risk. For these individuals, the scan can provide valuable insight into their heart health and help doctors decide how aggressively to manage risk factors. Even if your doctor is uncertain about the best treatment plan, a C.A.C. scan can offer clear guidance.
If You Think You Qualify…
If you might benefit from a C.A.C. scan, start by scheduling an appointment with your primary care doctor or a preventive cardiologist. A referral is usually required, so be ready to discuss your personal and family medical history, risk factors, and—even optionally—your 10-year cardiovascular risk using the American College of Cardiology’s calculator.
C.A.C. scans are available at hospitals, private imaging centers, and healthcare systems. Your doctor can provide a referral, or you can locate a facility online using tools like LabFinder. Out-of-pocket costs typically range from $100 to $400, though some centers offer promotions as low as $49–$99. Most private insurance plans, including Medicare, generally do not cover the scan.

The Hidden Power of Sunlight: Improve Vision and Vitality
A striking new study found that near-infrared light—a wavelength of natural sunlight just beyond what our eyes can see—can penetrate deeply into the body, even through clothing. This exposure helps cells produce energy, leading to measurable benefits for vision.
What the Research Shows
Just 15 minutes of full-body exposure to this long-wavelength sunlight—even with the eyes shielded—significantly improved color contrast sensitivity. Participants were better able to distinguish blues, yellows, reds, and greens when tested 24 hours later. These benefits occurred without light directly reaching the eyes, showing a truly systemic effect in which sunlight stimulates energy production in mitochondria throughout the body. The boost comes from increased ATP (cellular energy) production and reduced oxidative stress, two key factors in aging and many common chronic diseases.
Sunlight, Inside and Out

As we age, mitochondrial function naturally declines, which can affect vision, mobility, immunity, and overall energy. This research suggests that simply spending a few minutes outside in the sun can activate these energy pathways deep within the body. By contrast, LED-based indoor lighting often lacks these beneficial long wavelengths, potentially depriving us of natural cellular support.
Aim to spend around 15 minutes outside each day, ideally at midday when the sun’s infrared output is highest. Keep your eyes protected—there’s no need to look at the sun, which can be harmful. Just let sunlight hit your body; that’s enough to boost cellular energy, support vision, and promote healthier aging.

The Perfect Pre-workout Snack
According to a recent USA Today report, Bananas aren’t just a convenient, portable fruit—they’re packed with nutrients that make them an excellent choice for overall health and fitness. Registered dietitian Jamie Nadeau, RD, explains why they’re often called the “perfect pre-workout snack.”

Bananas contain potassium, vitamin B6, vitamin C, fiber, and magnesium. These nutrients support cardiovascular and digestive health, according to the Harvard T.H. Chan School of Public Health. A medium banana provides about 450 mg of potassium—roughly 13% to 20% of an adult’s daily needs—and around three grams of fiber, which is essential for gut health. They’re also naturally low in calories (about 110) and fat-free, making them a smart everyday choice.
One of their biggest advantages? They’re a fast, natural source of fuel. “Bananas are a quick and easy option, making them a perfect pre-workout snack for an energy boost,” Nadeau says. Their natural sugars and starches provide readily available energy without the need for processed snacks. Unripe bananas also contain resistant starch, which acts more like fiber and supports gut-friendly bacteria—further boosting digestive health.
While generally safe for most people, bananas can pose issues for certain health conditions. Those with high potassium levels or diabetes may need to monitor intake, as bananas can raise potassium or blood sugar. Choosing smaller or under ripe bananas may help manage this. Additionally, individuals with latex allergies could experience cross-reactivity with bananas.
Bottom line: For most people, bananas are an affordable, nutrient-dense, and convenient option—whether on their own or in smoothies, oatmeal, or paired with peanut butter.

You Can Beat Prostate Cancer: And You Don't Need Surgery to Do It - Second Edition
As of this writing, Bob’s second edition is still holding the No. 2 spot on Amazon—out of more than 7,000 books—on a search for “prostate cancer.” The book has 321 reviews and an average rating of five stars.
Beyond the Amazon stats, what truly matters is the feedback we hear from readers. Every day, men share how Bob’s book gave them the confidence to make one of life’s most important decisions. Some call it a “lifesaver,” others say it was the one resource that made proton therapy the clear choice. Hearing their stories reminds us why Bob wrote it in the first place.
Real Words from Real Readers—Even Doctors!
![]()
Great Information: Well written and this MD learned a lot.

Did Bob’s book help you? Your review matters.
When diagnosed with cancer, 89% turn to the internet for answers—40% on the very same day. Many end up on Amazon, where reviews carry serious weight. If Bob’s book helped you, please take a moment to write a review. As you can see above, they don’t have to be lengthy! Your words could help someone else find clarity and hope. Thank you.

Last Month’s Brain Teaser
The person who makes it has no need for it. The person who buys it doesn’t use it. The person who uses it doesn’t know it.
Answer: A coffin.
Winner: Congratulations to Doug Wilson of Knoxville, TN—winner of our September 2025 Brain Teaser!
Doug was treated for prostate cancer in 2019 at Provision CARES Proton Therapy Center—now the Thompson Proton Center—in Knoxville, TN. He completed 42 proton therapy sessions along with ADT therapy. “With the balloon, of course!” Doug shared, and he’s happy to report that he’s doing great and is a strong advocate for proton treatment.
A Navy veteran with more than 21 years of active duty and reserve service, Doug also spent more than 44 years working in the IT field. Today, he enjoys golfing, bowling, and driving Corvettes. He and his “wonderful wife Louise” are about to celebrate their 57th anniversary this October. Together, they have three daughters and eight grandchildren.


New Brain Teaser
What is the weight of a fish if it weighs 10 pounds, plus half its weight?
This one should be easy for anyone who knows simple algebra.
Send your answer to [email protected] for a chance to win a signed copy of Bob Marckini’s second edition book, You Can Beat Prostate Cancer.

The Cranky Shoplifter
A very cranky old woman was arrested for shoplifting at a grocery store. She gave everyone a hard time; from the store manager to the security guard to the arresting officer who took her away; she complained and criticized throughout the entire process.
When the woman later appeared before the judge, he asked what she had stolen from the store. The lady defiantly replied, “Just a stupid can of peaches.”
The judge then asked why she had done it. She replied, “I was hungry and forgot to bring cash to the store.”
The judge asked how many peaches were in the can. She replied, “Nine, but what do you care about that?”
The judge patiently said, “Well, ma’am, because I’m going to give you nine days in jail―one day for each peach.” As the judge was about to drop the gavel, the lady’s long suffering husband raised his hand and asked if he might speak.
The judge said, “Yes, sir, what do you have to add?”
The husband said, “Your Honor, she also stole a can of peas.”
Where Are You From?
A couple is waiting at the airport in Phoenix, bundled head-to-toe in heavy boots, parkas, scarves, and mittens—clearly heading back to the Canadian winter.
An older American couple nearby notices them. The wife says, “Look at those two—where do you think they’re from?”
Her husband shrugs, “How would I know?”
“You could go ask them,” she suggests.
“I don’t care. If you want to know, go ask,” he replies.
So, she does. She walks over and asks the bundled couple, “Excuse me, I couldn’t help but notice your heavy clothes—where are you from?”
The man answers, “Saskatoon, Saskatchewan.”
She returns to her husband. “Well?” he asks.
“I don’t know,” she says. “They don’t speak English.”
The Most Expensive Home in the U.S. Hits the Market
The most expensive home in the U.S. just hit the market—listed at an astonishing $300 million. Known as Little Lake Lodge, this Aspen, Colorado estate spans 74.1 acres, including a private six-acre lake. Billionaire couple Stewart and Lynda Resnick, co-owners of The Wonderful Company—the same people behind FIJI Water and POM Wonderful—purchased the land in the early 1990s. Lynda Resnick envisioned the main residence and collaborated closely with architect Peter Dominick to design and build the home, drawing inspiration from rustic National Park architecture.
The house itself measures 27,000 square feet and features 18 bedrooms, 20 full bathrooms, and four half baths. There’s ample parking, accommodating up to 45 vehicles. The estate borders public land while remaining just one mile from downtown Aspen, offering both privacy and convenience.
Adventure enthusiasts will appreciate the property’s trail system, designed for hiking, biking, and cross-country skiing. To put its value in context, the next most expensive home on the market is in New York, listed at $125 million, while Aspen’s current record sale of $108 million in 2024 will be far surpassed once this lodge sells.
Adding a fun twist, Pitkin County—the local government for Aspen—capped new home sizes at 9,250 square feet in 2023, making mega-estates like Little Lake Lodge nearly impossible to build in the future.
With its sweeping acreage, private lake, and luxurious design, Little Lake Lodge stands as one of the most remarkable estates in the country.
The High-Tech Hoax Preying on Seniors
A growing wave of fraud is targeting older Americans, and it’s leaving many devastated both emotionally and financially. Scammers pose as tech experts or security agents, using fear to convince seniors that their computers or bank accounts have been hacked. They trigger panic with alarming pop-ups, threatening emails, or urgent phone calls that warn personal information is at risk.
Once they have a victim’s attention, the fraudsters escalate the pressure, demanding remote access to computers or insisting on immediate payment to fix the supposed problem. Victims are urged to pay through gift cards, wire transfers, or by handing over sensitive information—things legitimate companies would never request.
Seniors are especially vulnerable because they may not be as comfortable with technology, and scammers exploit this uncertainty. Fear of making a mistake often leads victims to trust the caller, and social isolation can make it harder to double-check whether the warning is real.
The best defense is to pause before reacting. If a frightening message or suspicious caller claims your computer or accounts are at risk, don’t act immediately. Reach out to a trusted friend, relative, or your bank directly. Real companies don’t use scare tactics or demand instant payment. Awareness and caution are the strongest shields against this high-tech hoax.

Today is All We Have
Bobby Leach was a daredevil by trade. A former circus performer with Barnum & Bailey, he spent his life chasing danger. On July 25, 1911, he climbed into a steel barrel and hurled himself over Niagara Falls. He survived the plunge—though he emerged with two broken knees, a fractured jaw, and months of recovery—and his feat earned him worldwide fame.
Fifteen years later, he slipped on an orange peel, broke his leg, the injury turned septic, and he died. The sequence sounds almost trivial in the telling—an orange peel—yet it was the painful cascade of real consequences that mattered: an ordinary moment that changed everything.
There’s a clear lesson in Leach’s life: even the boldest achievements can’t guarantee the future. Yesterday is gone and tomorrow may never come. What matters most is the moment we have right now. So, make the most of today—laugh, love, forgive, and live fully—because everything can change in an instant.
Low PSAs to all,
Bob Marckini and Deb Hickey
Want a printable version of this issue?
👉 Download the PDF here.
NO MEDICAL ADVICE: Material appearing here represents opinions offered by non-medically trained laypersons. Comments shown here should NEVER be interpreted as specific medical advice and must be used only as background information when consulting with a qualified medical professional.