Dear Members (a note from Bob Marckini):
I have a dilemma. I’m overwhelmed with gratitude for the hundreds and hundreds of birthday cards and letters so many of you sent me – when prompted by my daughter, Deb – for my 80th birthday back in early April. I’m astounded with the quality and variety of the cards and especially with the notes and letters written with heartfelt thoughts and clearly significant time and effort (some hand-wrote long missives; some typed three-four pages; others included drawings, photos, poems…).
My dilemma is that, ordinarily, I’d respond to each message individually. But, alas, it would take me the rest of my life to do so.
I’ve disciplined myself to read 10 to 20 cards every morning, and I must admit, it’s my favorite part of the day. It’s “the gift that keeps on giving.”
And, by the way, cards are still coming in!
“I think we’re going to need a bigger binder.”
When I completed proton treatment almost 23 years ago, I brought home with me dozens of photographs and assorted memorabilia from my eight-week odyssey at Loma Linda. During the ensuing years, I saved many newspaper articles, magazine articles, and letters from some very special people including sports professionals (like Ken Venturi), members of the clergy (including several pastors and a bishop), three ambassadors, several corporate executives, numerous members of the medical profession, and lots of everyday people I counseled from all walks of life. I stored all these things in a cardboard box.
About 10 years ago, Deb “borrowed” the box with the articles, letters, memorabilia, and photographs, and compiled them into a huge, three-ringed binder. She gave this to me as a birthday present, and I’ve treasured it ever since.
Then I began adding to the binder with new articles and mementos, including letters from patients I’ve counseled and literally hundreds of letters I received from people at Loma Linda notifying me of gifts made to LLUH in my honor by members of our group and others. The giant binder started bursting at the seams. Long before I received the two huge boxes of cards and letters for my recent birthday, I said to Deb, to paraphrase a line from one of my favorite movies, Jaws, “I think we’re going to need a bigger binder.”
Gratitude
Every day when I open and read more of the cards and letters, I’m overcome with gratitude for the time and effort so many of you have put into these precious gifts which have touched my heart. Many of you expressed your appreciation for my help and guidance at a very low point in your lives. Several of you wrote about your fears, the pressure from your urologists to have surgery, and the fabulous results from your proton therapy. The themes were common, but each story was different. And they didn’t all come from Loma Linda patients. To date, I have cards and letters from members who were treated at 14 proton centers, including one in Europe. And there are lots more yet to open.
In the body of this month’s BOB Tales, we’ve included several excerpts from the hundreds of cards and letters I’ve already opened and read. Deb and I plan to share more of these in future newsletters.
Once again, I can’t adequately articulate how grateful I am for the overwhelming love, support, and kindness that you’ve shown me for my 80th birthday. Your cards and letters brought tears to my eyes; they will forever be cherished.
It’s been my passion to bring peace, comfort, and hope to those who’ve been diagnosed with prostate cancer and are searching for answers. Your messages have reaffirmed the importance of this work. You’ve shown me that my efforts have made a difference in your lives. I’m honored to have such amazing people in my life, and I look forward to continuing our journey together.
------------------
This month’s BOB Tales is a two-month issue, considerably longer than our standard newsletter, as we have so much to share with you, including Deb’s comprehensive review of the annual NAPT conference she attended in Salt Lake City, UT last month.
Other topics covered in this issue include the increasing role artificial intelligence is playing in medicine in general and prostate cancer treatment in particular. New approaches to treating advanced prostate cancer; an intriguing new anesthesia; the role of mental wellness in dealing with cancer; some surprising health tips; and – who would have guessed – an unsolved brain teaser also highlight this month’s newsletter.
Oh, and one more thing – you may have noticed we have a new website! Things have been pretty busy over here.
------------------
As always, we appreciate feedback and welcome any suggestions you have on how to improve the value of the BOB Tales to our members. Just send an email to [email protected].
Bob Marckini
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
- AI Tools Could Revolutionize the Way Prostate Cancer is Treated
- Prostate Biopsies – A Laughing Matter?
- Mental Wellness in Prostate Cancer Patients
- Special Segment: National Proton Conference 2023
- Faking it with Sugar Substitutes
- 5 Surprising Benefits of Walking
- hMPV: The ‘Most Important Virus You’ve Never Heard Of'

AI Tools Could Revolutionize the Way Prostate Cancer is Treated
Should a prostate cancer patient be treated at all (active surveillance)? And if treated, should androgen deprivation (hormonal) therapy be used in addition to radiation therapy to improve the patient’s chances of a cure? These questions and more are being answered with the assistance of artificial intelligence (AI) according to Dr. Dan Spratt, chairman of the department of radiation oncology at University Hospitals Cleveland Medical Center. The use of AI, along with the first-of-its-kind “predictive biomarkers” is “wildly different and very advanced from what we do today,” said Dr. Spratt.
Spratt explained that, “The ArteraAI test takes the tissue from a man’s biopsy and digitizes it, then runs a highly sophisticated algorithm using artificial intelligence to tell you how best to personalize therapy.”
ArteraAI is a Jacksonville, FL-based company that’s leading the charge on this technology. Artera says they have developed the first ever, predictive test that can help identify the best treatment for localized prostate cancer.
Interpreting Prostate Biopsies
Dr. Jennifer Bepple, a Maryland-based, board-certified urologist, confirms that AI should help remove subjectivity in analyzing and interpreting biopsy slides. This issue, in particular, excites us. We’ve reported here and in Bob’s book that the reading/interpretation of biopsy slides is extremely subjective and it’s not uncommon for two pathologists to report different Gleason scores on the same slides. This is a significant problem because the customized treatment for any patient is based, to a great extent, on Gleason score. Improperly interpreted slides could result in a patient being over- or under-treated for prostate cancer. Over-treated patients could experience significant life-altering side effects, and under-treated patients could see a recurrence of their cancers resulting in the need for salvage treatment.
Despite rising concerns about all the unknowns and risks associated with the rapidly growing use of artificial intelligence, its potential – particularly in the medical field – appears to be significant. We’ll be hearing much more about the benefits of AI in medicine in the coming months and years.
Prostate Biopsies ─ A Laughing Matter?

Can you imagine laughing through a prostate biopsy? That day may be coming, according to a recent Medscape article. The author says that, “an old dog – nitrous oxide – can learn new tricks – managing pain in men undergoing transrectal biopsies.” This was reported at the 2023 annual meeting of the American Urological Association.
Nitrous oxide is often used as an anesthetic during dental procedures, childbirth, after trauma, and even in end-of-life care.
According to researcher Heidi Rayala, MD, PhD, assistant professor of surgery at Harvard Medical School, “At concentrations of less than 50 percent, nitrous oxide is classified as a minimal sedative, making it a promising option for many urologic outpatient procedures such as prostate biopsies.”
The study involved 128 men who were given either nitrous oxide or a placebo during their biopsy procedures. While researchers didn’t find a significant difference in the levels of anxiety between the two groups, the men who received nitrous oxide tolerated the pain and discomfort “better than expected,” according to the study.
Mental Wellness in Prostate Cancer Patients

Learning you have cancer affects more than your physical health. The fear, stress, and anxiety that accompany such a life-changing diagnosis can take a huge toll on your mental health. From processing the news of a cancer diagnosis to navigating the many treatment options available to undergoing treatment – it’s important to focus on the body and the mind.
Yes, even guys have to pay attention to mental wellness. In addition to the shock of hearing you have the “Big C,” those with prostate cancer have the added concern about potential side effects from treatment such as erectile dysfunction, incontinence, and other related problems. Then there’s the worry about cancer recurrence. Further, hormonal therapy, which is typically recommended for Gleason scores 4+3 and higher, can cause psychological side effects including mood changes and irritability which, compounded with existing anxiety, could impact mental health.
Do Men ‘Hide Things’?
A 2014 study by UK researchers found that among nearly 4,500 prostate cancer patients across the treatment spectrum, 17 percent reported depression and 27 percent reported anxiety before they were treated. The figure for anxiety is about twice that in the general population of men in the U.S., said John Oliffe, PhD, founder, and lead investigator of the University of British Columbia’s Men’s Health Research program. “Untreated anxiety can lead to other mental health problems, including depression and suicidal thoughts and behavior,” said Oliffe.
Scott Tagawa, MD, medical director of the Genitourinary Oncology Research Program at Weill Cornell Health in New York City, thinks the total number of men in mental distress may be understated. “Men tend to be less communicative and verbal,” said Tagawa. “They hide things.”
Emphasis on the Whole Patient
Jim C. Hu, MD, a professor of urology at Weill Cornell, said mental health issues are more prevalent because of “a greater emphasis on the whole patient. This goes with patient-centered care. There’s a focus on mental health issues in terms of patient care, particularly as it comes to cancer patients.”
That’s in line with LLUCC’s “Make Man Whole” mission, which aims to treat the “whole” patient – body, mind and spirit – by showing care and compassion for every patient as soon as they walk in the door; providing free membership to their onsite fitness center, incorporating nutritional and wellness education and healthful, vegetarian meals on campus; holding weekly patient support group meetings, scheduling lunch and dinner outings and weekend visits to local attractions; as well as spiritual guidance and support.
Penn Medicine has a “patient engagement team” that has built a vibrant and engaging community for its patients. They offer virtual reality experiences for “distraction therapy” and a “listening lab” where patients can listen to other patients’ pre-recorded stories of treatment and life after treatment. Many other proton centers have developed programs to support the whole patient as well.
Caring for the whole patient helps patients and their families manage the psychological aspects of the disease and the overall adjustment to life with cancer. It helps improve the patients’ quality of life thereby minimizing disease symptoms and improving recovery and overall health.
One Doctor’s Approach
Dr. Andrew J. Roth, a psychiatrist at Memorial Sloan Kettering Cancer Center in New York City, has devoted his entire career to mental health issues in prostate cancer patients. Twenty-five years ago, he helped develop the “distress thermometer” to detect cancer-related distress in men with prostate cancer. He’s still working as a liaison to the genitourinary medical oncology program.
“Screening for distress tries to identify signals that someone is having difficulty dealing with cancer that might interfere with making treatment decisions, managing treatment, improving quality of life, or that a particular patient doesn’t have enough social support,” Roth says. “Then there’s the opportunity to get them the help they need. If we don’t ask, we may not find out, and won’t be able to help these men cope better with their prostate cancer and their lives in a timely manner.”
Psychiatric or Not Psychiatric?
In an interview with Prostate Cancer Foundation CEO Charles J. Ryan, MD, Dr. Roth reiterated the effects of hormonal treatment on patients’ mental wellness. “These medications can have a lot of effects on the whole body,” said Roth. “They can cause weakness. They can cause fatigue. They can cause men to start crying at the drop of a hat even if they’re watching a baby diaper commercial.”
“Not everything that looks psychiatric in the world of prostate cancer is psychiatric,” said Roth. “Very often, if a patient is having irritability, mood changes, or anxiety because of his treatment – for example, chemotherapy is sometimes accompanied by a steroid that can cause some emotional changes – the family thinks he’s depressed or he’s got an anxiety disorder.” That’s where Roth’s expertise comes in handy – he can distinguish between the effects of medication versus a psychiatric episode.
Distress – the Sixth Vital Sign in Cancer Care?
Along with the traditional clinical measurements or vital signs in cancer care – body temperature, pulse/heart rate, respiratory rate, blood pressure, and pain – Dr. Ryan recommends making “distress” a vital sign. “It was a substantial moment in oncology when we realized we were underassessing and undertreating pain in cancer patients, so we made it a vital sign,” said Ryan. “‘Are you in pain today?’ It’s an important question. And I would think, ‘Are you in distress today?’ is a potential vital sign that we should be thinking about as well.”
How to Manage the Feelings
The most important thing to do is to reach out for help. Talk with your doctor. Talk to your partner. Join a support group – in person or online. Having social support can be hugely helpful in combating anxiety or depression. Additionally, channeling your feelings into enjoyable activities may also help reduce anxiety and depression. Try exercising, journaling, prayer, or meditation.
Oftentimes, medications can help manage feelings. Though antidepressants and antianxiety medications have been shown to ease emotional symptoms during cancer treatment, some are hesitant to take them. It’s important to speak with a psychiatrist that understands your diagnosis and then together you can make the decision as to whether medication is right for you.

National Proton Conference 2023

The 11th annual National Association for Proton Therapy Conference was held at the Hyatt Regency in Salt Lake City, UT May 6 through 9. This year’s event was titled, Elevating Access, Research and Innovation in the Field of Particle Therapy.
Every year, the National Association for Proton Therapy (NAPT) gathers together leaders in the field of particle therapy with a robust agenda focused on emerging clinical research, operational efficiencies, barriers to patient access such as the insurance prior authorization processes, and a new addition, a special session presented by the Particle Therapy Co-Operative Group (PTCOG), a non-profit worldwide organization of scientists and professionals interested in proton, light ion, and heavy charged particle radiotherapy.
Deb Hickey, along with nearly 300 others in the proton therapy world, attended the four-day event which featured speakers from more than 40 cancer centers and proton therapy facilities. Presentations and panel discussions covered topics such as FLASH therapy, policy initiatives, patient engagement, and advancements in oncology. An exhibition hall featured 25 industry partners and technology providers.
 |
Following is a letter written by Jennifer Maggiore, Executive Director at the National Association for Proton Therapy, that includes insights from the 2023 NAPT Annual Member Survey written exclusively for the BOB Tales newsletter. |
Proton Therapy Trends: Insights from the NAPT Annual Survey
We are delighted to share the latest updates from the National Association for Proton Therapy annual survey, a crucial tool in monitoring and reporting on proton therapy trends in the United States. As the nation's sole organization dedicated to this innovative treatment modality, NAPT plays a vital role in educating and raising awareness about the clinical benefits of proton therapy.
At the recent conference held in Salt Lake City, NAPT revealed the insightful findings from their 2022 survey which encompassed data reported by 35 proton centers across the country. The results not only underline the increasing adoption of proton therapy also shed light on the diversification of cancers treated and the ongoing challenges faced by patients seeking access to this life-saving, life-changing treatment.
Over the past year, the number of patients treated with proton therapy continued its upward trajectory, reaching a significant milestone of over 16,000 individuals. Among them, 4,277 men received proton therapy for prostate cancer—a meaningful increase from the approximately 2,000 patients reported when the NAPT first initiated its survey in 2013. This substantial increase underscores the growing recognition of proton therapy as a preferred option for prostate cancer treatment.
Furthermore, the survey data indicated an encouraging expansion in the utilization of proton therapy for other cancer types. Notably, there has been an upsurge in the percentage of patients with head and neck cancer and breast cancer who benefited from proton therapy. This shift signifies the evolving landscape of research, as evidence continues to emerge showcasing the value and efficacy of proton therapy across various cancer types.
To further advance the field, researchers are actively exploring the applications of proton therapy in breast, lung, esophageal, and FLASH therapy through numerous ongoing clinical trials. These studies hold tremendous promise and have the potential to revolutionize the delivery of proton therapy, opening new avenues for precision treatment and improved patient outcomes.
While the survey brings to light many positive developments, it also highlights persistent challenges in patient access to proton therapy. Commercial insurance denials remain a significant obstacle, with initial denials affecting over 30 percent of proton therapy authorizations. Additionally, more than 60 percent of patients faced delays in starting treatment due to the lengthy prior authorization process.
However, it is encouraging to note that the numbers have improved slightly compared to the previous year, indicating the dedication and advocacy efforts of NAPT and our member centers. Proton centers continue to invest additional resources to address the burden of prior authorization, recognizing the importance of timely access to treatment for patients in need.
Physicians are bearing the brunt of these challenges, spending increasing amounts of time on writing appeal letters and participating in peer-to-peer reviews. Despite these obstacles, NAPT member centers remain committed to streamlining operations and advocating for patients, ensuring equitable access to this life-changing therapy.
NAPT and its member centers are steadfast in our mission to educate and raise awareness about proton therapy, ensuring patient choice and access, and fostering research and innovation for optimal and cost-effective utilization of this groundbreaking treatment. As we move forward, we must continue to support and amplify these efforts, working collaboratively to overcome barriers and ensure that proton therapy remains accessible to all who can benefit from it.
Together, we can drive progress, advance proton therapy, and provide hope for a brighter future in cancer treatment.
2023 Conference Highlights
Following are highlights from a select few sessions at last month’s conference. It includes information we think would be of interest and value to our members.
Best Practices for Managing Proton Therapy Appeal LettersLegion Heathcare Partners is a group of healthcare executives, clinical advisers, and domain experts that provides solutions to healthcare providers – including consulting, technology, education, and training – to eliminate barriers to proton therapy development and ownership. Legion’s President and COO, Matt Palmer, led this very informative session on navigating the insurance appeals process.
Receiving an insurance denial after a cancer diagnosis creates additional an emotional burden for the patient and his/her family. But it’s important to understand, you’re not alone, and in fact, you shouldn’t handle this alone. The first step should be to speak with a financial counselor or someone on the insurance billing team at your treatment facility so they can explain the process and offer support.
Though navigating the appeals process can be daunting and frustrating, keep in mind that winning takes patience, persistence and a solid understanding of why proton therapy is a viable treatment option. The treatment facility most likely has an insurance appeals team that has done this many times, and they can walk you through the process which includes:
- Understanding the reason coverage was denied
- Outlining specific steps required to file an appeal
- Discussing your specific health insurance plan (HMO, PPO, Tricare Military, Medicare or Medicare Supplement, Etc.)
- Finding out deadlines and information required by health insurer
- Explaining the levels of appeals your health insurer allows
- Finding out if your plan is funded by an employer and if the health insurer is the administrator of the plan
- Documenting every interaction with your insurer, including phone calls made and received
Matt explained that insurance companies want to know why proton therapy is beneficial for the patient. Why is it better than another treatment option? What are the toxicity benefits? Written input from your physician – in the form of a letter of “medical necessity” which includes medical documentation detailing the reasons why proton therapy is the best treatment option for your specific condition – can be extremely valuable.
Also, include any recent medical literature such as peer reviewed studies from professional journals documenting the medical effectiveness of proton therapy. If you’re enrolled in a clinical trial, be sure to include this information. You may also want to write your own personal letter to include in the appeal.
Sometimes patients seek legal counsel during this process. There are attorneys that specialize in handling insurance coverage denial appeals and they also know specific state laws concerning health insurance denial appeals and can ensure health insurers follow their own rules as well as the state’s laws. Also, health insurers may take the denial appeal more seriously if an attorney has been hired.
Matt also mentioned getting support from the National Comprehensive Cancer Network (NCCN) or the American Society for Radiation Oncology (ASTRO). For example, NCCN offers patient-friendly adaptations of their NCCN Guidelines. Patients can search for their specific cancer type, view webinars and animations, and order free print copies of specific documents. There’s even a “Patient Guide for Cancer” mobile app. The ASTRO Model Policies is also a helpful resource. It was developed as a means to efficiently communicate what the organization believes to be correct coverage policies for radiation oncology services, and it addresses coverage for proton therapy in a comprehensive and detailed overview.
Suveena Mathew, senior manager for oncology financial services at Legion, spoke about the importance of writing descriptions of the patient’s medical records in a clear and concise manner. Even if the reviewer is a medical doctor, it doesn’t mean he/she’s familiar with oncology and the clinical language associated with that branch of medicine. It’s also extremely important to include specific information about the patient, including his/her personal story. This makes the patient real and unique.
If you refer to a publication in your appeal, print that publication and attach it to the back of the appeal letter. Medical reviewers typically have a stack of cases he/she’s reviewing, so time may be limited. Give him/her everything all wrapped up with a bow.
Suveena also spoke about highlighting key pieces of clinical information so the reviewer will immediately see it if they’re scanning through documents quickly. Make sure key pieces of information are included in the body of the appeal letter. Bold or underscore where you need to.
Revolutionizing Patient Education: Exploring the Synergy of AI and VR ApplicationFern Nibauer-Cohen of Penn Medicine and Dr. Arpit Chhabra of the New York Proton Center spoke to attendees about the role of artificial intelligence (AI) and virtual reality (VR) in the field of proton therapy.
A typical patient consultation involves a comprehensive evaluation with a review of the patient’s medical history, pathological and genomic data, a diagnostic study, a physical examination, and a discussion of pre-existing health conditions and risk of radiation therapy side effects. The evaluation typically results in a recommended treatment plan.
We learned that using AI, doctors can automatically extract key clinically actionable features that enable personalization of a patient radiotherapy plan because the AI platform can predict the radiation sensitivity of a tumor and the optimal dose prescription that’s achievable with a specfic treatment plan.
AI for Contouring
Contouring a tumor is a critical process in treatment planning because it involves outlining a tumor as well as nearby organs at risk to guide radiation treatment plans that optimize tumor control and reduce side effects. Manual contouring of a tumor and associated lymph nodes is a time-consuming, but crucial task. The accuracy of tumor segmentation can directly affect treatment outcome. If mistakes are made, it can lead to underdosing or overdosing. AI has the potential to dramatically increase the efficiency, reproducibility, and accuracy of the this process.
Treatment planning for patients is a time-sensitive, iterative process whereby the dosimetrist designs the dose distribution, making necessary changes on a trial-and-error basis to carry out the goals outlined in the patient’s dose prescription. AI tools for treatment planning can automatically predict the optimal dose distribution and idenfity the treatment machine parameters required to achieve that distribution. AI algoritthms also have the potential to provide more detailed information on tumor responses throughout the course of treatment.
ChatGPT
During this session, attendees also learned about ChatGPT – a natural language processing tool driven by AI technology. It allows users to have a “human-like” conversation and according to Deb, “It’s scary.” ChatGPT has a massive knowledge base and can mimic human-like responses.
The good news is – ChatGPT is already helpful in the healthcare world because it can automatically book patient appointments and manage their health information. It can also assist with clinical decision support by providing real-time, evidence-based recommendations such as flagging potential drug interactions. It can also suggest treatment options for specific conditions and provide relevant clinical guidelines.
If you’d like to try it yourself, visit chat.openai.com and sign up for an account using your email address or a Google or Microsoft account.
Virtual Reality
VR is a computer-generated, fully immersive experience that simulates your physical presence in an artificial, but seemingly real environment. Instead of just viewing a screen in front of you, you put on a VR headset, and immediately feel like you’re walking through a forest, floating through space, on the battlefield, playing a game
of tennis … The VR experience can effectively mimic the real world or put you in a fantasy world. It posesses qualities like gravity, shadows, and depth and can be completely convincing for the brain.
According to experts at Penn Medicine, VR has opened some really interesting doors for neurologists, psychologists, and other researchers. While some headsets are often associated with gaming, VR has applications outside of entertainment as well – science and medicine.
One way Penn uses VR technology is by using it as “distraction therapy” for its patients. The voice-guided meditation program runs fewer than 10 minutes and gives patients the chance to leave their thoughts of cancer behind for a short while and focus on something more relaxing as they wait for their treatment. Caregivers, family, and friends who are visiting can also use the equipment.
Penn also uses VR for patient education. The device allows patients to tour the facility, go through treatment, and ring the final “graduation” bell all in one sitting. It gives patients and caregivers a detailed idea of what the patient will experience.
VR simulations are also used for global staff education, treatment research, and staff burnout. Nibauer-Cohen is involved with the International VR Healthcare Association; she’s attended a few meetings and is considering more ways to use VR at the medical center.

A Race Against Time: Examining Disparities in Authorization
Health disparities and inequities have been documented in the use of radiation therapy for cancer screening, diagnosing, staging, and treatment delays, as well as clinical outcomes, clinical trial participation, follow-up, and even survivorship. In regard to proton therapy specifically, studies have shown that while the use of the treatment has increased significantly over the years, black people have a lower likelihood of receiving the therapy compared to their white counterparts. One reason is geographical access to proton therapy. Even though the number of U.S. proton centers continues to grow, there’s a wide open space in the rocky mountains and the far western part of the Midwest. As a result, people living in that part of the country can’t easily access treatment.
Ample literature has stated that Hispanics and asian patients also have significantly lower odds of receiving proton therapy than white people. So, unfortunately, though prostate cancer is a common disease, it’s complex and comes with risks and outcomes influenced greatly by factors in addition to access – such as socioeconomics, genetics, and biology.
Though there are many contributors to health disparities, the speakers in this session, Dr. Curtiland Deville from Johns Hopkins, and Allison Randolph, a soon-to-be MBA graduate from Meharry Medical College in Nashville, TN, focused on health insurance status and type and how those may influence disparities – especially the prior authorization (PA) process.
PA is a cost-control process used by some health insurance companies to determine if they’ll cover a prescribed procedure, treatment, or medication. “Prior” means the authorization must be obtained before the service is delivered to the patient.
A 2022 study, Racial and Ethnic Health Disparities in Delay to Initiation of Intensity-Modulated Radiotherapy, researchers tried to better understand the role of different insurance policies and their effect on racial disparities. They found that black patients with private insurance took longer to start treatment than those on Medicare. Randolph explained to attendees that physicians complete about 45 prior authorizations every week and of those, 35 percent have to hire additional staff just to get through them. Sometimes, they have to outsource prior authorizations to other companies. The process is extremely burdensome.
Johns Hopkins Analysis
Researchers at Johns Hopkins wanted to better understand the prior authorization experience, so they performed a retrospective analysis of a prospective cohort of their patients. They categorized the data by insurance provider and focused on 10 disease sites – lymphoma, sarcoma, gastrointestinal, breast, head and neck, thoracic, genitourinary, pediatric, gynecological, and central nervous system.
They performed the bulk of their analysis on the cases that were denied insurance coverage, and learned there was no difference in approval timing when comparing private to public health insurance, however the public insurance approved at much higher rates (i.e. Medicare doesn’t require prior authorizations).
In the case of genitourinary cancers (including prostate cancer), Blue Cross Blue Shield came out as the clear winner in regard to approval rate, while Cigna came in last. Although it’s important to note – there were only six patients in the study with Cigna insurance at the time of treatment.
So, What Can Be Done?
Although the PA process can be lengthy, the process is there to ensure that treatments and medications are medically necessary, clinically appropriate, and align with evidence-based guidelines. They may also improve patient outcomes by ensuring appropriate use of medications thereby minimizing harmful drug interactions and adverse events.
Solutions to streamlining the PA process include leveraging technology; increasing transparency and communication between payers and providers; shortening turnaround times for approvals, selective waiving of some PA requirements, creating an electronic trail (not a paper one which can be susceptible to security issues and are challenging to track and monitor), and advocacy of practicing physicians.
Johns Hopkins researchers intend to continue their own research to examine whether disparities are further exacerbated by sociodemographic characteristics such as race, ethnicity, age, socioeconomic status, and other social determinants of health.
Beyond the Legal Battle: Navigating Litigation Options and Strategies to Enhance Patient Access to Proton Therapy
This session was presented by attorney Doug Terry of Doug Terry Law in Oklahoma, and Dr. Andrew Chang from California Protons. They spoke about a couple of recent healthcare lawsuits they’d been involved with and the lessons they learned from each. Deb felt her blood boiling while listening to the the following stories:
Cunningham vs. Aetna
Terry and two of his law partners tried the case of Ron and Orrana Cunningham vs. Aetna, along with the help of Dr. Chang back in 2018. Ron’s wife, Orrana, was diagnosed with stage IV nasopharyngeal cancer in November 2014, when she was just 53 years old. Ron and Orrana had just finished building a house – almost entirely with their own two hands – on a farm near eastern Oklahoma county.
When Orrana was diagnosed, she sought local medical advice. She was told that due to the complexity of her disease, she should visit MD Anderson in Houston, TX.
Doctors at MDA evaluated Orrana and determined she needed proton therapy because her tumor was at the base of her skull, adjacent to multiple “critical structures” including her brain, optic nerves, and brain stem. Although traditional radiation could potentially kill the tumor just as well, proton therapy would increase the chances that Orrana could be cured without devastating side effects because the nearby critical structures would be spared direct radiation. Potential side effects included blindness, loss of memory, loss of taste, and potentially, death.
MDA submitted a request for coverage to Orrana’s health insurer, Aetna. The request was denied. An appeal – including a 150-plus page package of information supporting Orrana’s case – was also denied, and the case eventually went to trial.
Evidence at the trial revealed Aetna recommended the claim be denied because “proton therapy is experimental or investigational.”
Other evidence showed one of the Aetna medical directors who reviewed the claim held a “peer-to-peer” phone call with an MDA radiation oncologist to discuss the case. Apparently, this Aetna doctor was an internal medicine/family practitioner before going in-house 25 years prior, and hadn’t treated a single patient since.
More evidence revealed that two Aetna doctors who reviewed the claim were not familiar with the duty of “good faith.” They also spent just 30-45 minutes reviewing the claim (including a 150-plus page appeal package).
Meanwhile, after all of her requests for coverage were denied, time was running out and Orrana still needed proton therapy. So, Ron and Orrana mortgaged their dream home to pay for it.
Orrana underwent proton therapy and it appeared to work. However, after she returned home, she developed herpetic encephalitis. Her brain swelled severely, causing her brain stem to herniate, and she passed away. Ron filed a lawsuit shortly thereafter. The evidence was the financial stress of the whole situation, in addition to the fact she was battling cancer, weighed heavily on Orrana.
After 12 days, the jury found:
- Aetna breached its insurance contract with the Cunninghams and therefore the Cunninghams were awarded the $92,082.19 they paid out of pocket for proton therapy.
- Aetna acted in reckless disregard of the duty of good faith and fair dealing it owed the Cunninghams in connection with the way it investigated and evaluated the request for coverage for proton therapy. Terry and his team offered evidence and argument in court that the Aetna claim handling system is designed to use unqualified, untrained, overworked and biased personnel to consider claims like this. The jury agreed.
The jury awarded compensatory damages for the emotional distress caused by Aetna’s repeated denials. They awarded Mr. Cunningham $500,000 individually, and Mrs. Cunningham’s estate $15,000,000.
Terry then proceeded to a punitive damage phase of the trial. He and his team argued to the jury that to send Aetna away without punishing them for what the jury had already found was reckless conduct would not be a just result. The jury agreed and awarded another $10,000,000 in punitive damages.
This brought the total verdict to $25,592,089.
An Important Lesson – Speaking to the Jury
Dr. Chang explained that ensuring a jury fully understands an insurance injustice is imperative. To do this in a trial like Cunningham vs. Aetna, they first need to understand the basics physics of radiation oncology. Then they must understand the difference between conventional radiation and proton beam radiation therapy, including the advantages of proton therapy in regard to side effects. Then it’s important to clearly explain the thought process behind the doctor’s recommendation, including the patient’s unique diagnosis and circumstances.
Jury members typically don’t want to be there, so it’s not easy for them to sit through and pay attention to an educatonal session on radiotherapy. Therefore, speak to them like first-time medical students and keep them engaged through staying in motion, using examples, and speaking clearly.
Eskew vs. United Healthcare
A couple of years after the Cunningham trial, Terry and his partners tried the case of Sandy and Bill Eskew vs. Sierra Health and Life, a UnitedHealthcare Company. Again, they called in Dr. Chang for assistance.
In 2015, Bill was diagnosed with stage IV metastatic lung cancer when he was just 63 years old. Sandy’s research led them to MD Anderson. Bill’s world-renowned thoracic radiation oncologist, as well as a team of other doctors and scientists, conducted several tests to determine the best treatment for Bill. Their decision was that proton therapy would give him the best chance of a cure while sparing nearby critical structures. Bill’s tumor was in the middle of his chest, right next to his esophagus, trachea, heart, and healthy lung tissue.
MDA submitted a request to Sierra Health for prior authorization of proton therapy, including a detailed letter explaining the rationale for need for this particular type of treatment, along with Bill’s medical records supporting the request.
The request was denied by Sierra. Instead, they approved an alternative photon-based form of radiation – Intensity-modulated Radiation Therapy (IMRT – about half the cost of proton therapy). But MDA had already compared proton therapy and IMRT for Bill’s unique diagnosis, and concluded that proton therapy was superior and safer.
After the denial, Bill and Sandy were faced with a difficult choice. Bill could either go untreated, or he could ungero IMRT, which could not be delivered as precisely as proton therapy. Bill decided to be treated because he wanted the best chance to live as long as he could to enjoy life with Sandy and his children and grandchildren.
During the treatment, Bill began to suffer symptoms of esophagitis related to the radiation. After the treatment was completed, the esophagitis got worse. Ultimately, it caused Bill’s health to deteriorate. Cancer patients need good nutrition and hydration so their bodies can fight the cancer. When Bill attempted to eat, it was painful for him to swallow. He had dry heaves or vomited every time he attempted to drink or eat. In addition to the physical suffering, he also suffered a loss of his quality of life. Bill became reserved, withdrawn, depressed, and angry. This dramatically affected his life and the life of those who loved him. Bill soon passed away – about a year after his treatment.
The claim was made that the doctor that Sierra chose to assess Bill’s request for proton therapy coverage was unqualified to understand and evaluate his medical condition and the reasons why proton therapy was determined to be the best treatment option for him. It was also charged at the trial that the Sierra doctor lacked even a basic understanding of the medical issues involved with Bill’s claim. It was also learned that the doctor Sierra chose was an independent contractor and was handling claims part-time in addition to running a full-time oncology practice. He testified that he was handling 20-25 claims a week for Sierra, and that he’d spent 30-60 minutes reviewing Bill’s claim before he denied it. However, the doctor’s billing records showed he handled nearly 80 claims for Sierra the week he denied Bill’s claim. He billed Sierra 16.5 hours for that work. This indicated that he spent an average of 12 minutes per claim.
Evidence also showed the Sierra doctor didn’t even look at the terms of the policy Sierra sold to Bill before denying his claim. The doctor also didn’t write, nor did he ever see, the denial letter sent to Bill. Instead, the letter was “cut and pasted” by one of Sierra’s clerical employees from a spreadsheet containing stock language.
The lawsuit argued that IMRT, a less precise method of radiation treatment, caused Bill to suffer physical injury, physical pain, mental suffering, emotional distress and anxiety. The lawsuit also cited the distress and anxiety related to the initial denial for proton therapy that Bill received.
Terry and his team claimed Sierra breached its contract with Eskew when they denied treatment. They also alleged the company acted in bad faith and breached the Nevada Unfair Claims Settlement Practices Act.
Eskew’s family was awarded $40,000,000. An additional $160,000,000 was awarded as punitive damages against Sierra Health. The total verdict was $200,000,000.
An Important Lesson – Patients’ Best Interest Not Always in Mind
Often, the medical directors representing the health insurance companies to review claims are family medicine practitioners or internists – even when the insured is seeking review of a claim for coverage for a specialized procedure such as proton therapy for a cancer diagnosis. These medical directors often have zero experience with a particular diagnosis, or might have zero knowledge of the treatment for which they are reviewing coverage. It’s also sad to remember that these medical directors are employees or sub-contractors of the insurance companies and are often not working for the best interest of the patient.
NAPT is Coming to Boston!
We’re excited to announce that the next National Proton Conference will be held in Bob and Deb’s neck of the woods! NAPT is coming to Boston, MA, April 6 – 9, 2024. Stay tuned for more info …

We’ve been producing BOB Tales newsletters for more than 20 years. During this time there have been articles that many new members haven’t seen, and some longer-term members may have forgotten. So, we periodically re-run articles from past newsletters. The following is from June 2007.
Faking It with Sugar Substitutes
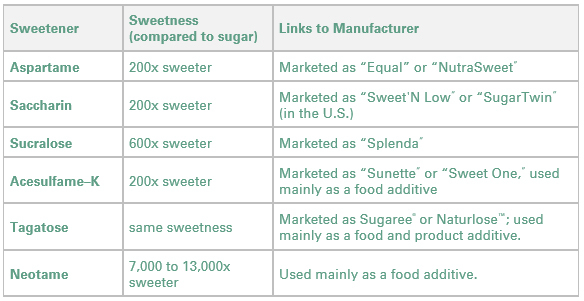
Artificial sweeteners may be safe, but are they healthful? When you’re on a diet, the “no-sugar” label on many packaged foods can be tempting. Sometimes no sugar means “not sweetened.” And sometimes it means the food has been sweetened artificially.
As many as 75 percent of people in the U.S. consume artificial sweeteners. Sugar substitutes may be safe, but are they really healthful? Not if they’re causing you to: 1) overeat; 2) consume too many empty calories; or 3) neglect nutrients. And that’s not considering the fact that we don’t know the long-term effects of consuming artificial sweeteners. How can these sweet substances possibly cause unhealthful habits?
Here’s something to consider when deciding the best way to incorporate sugar substitutes into your diet: You’ll have to guard against overeating. Substituting artificial sweeteners for sugar is an easy way to cut back on calories and thus lose weight, right? Not really. Although sugar substitutes may help you maintain your weight after shedding pounds, they generally won’t help you lose weight.
They may cause you to eat more servings than you would if the food or drinks were sweetened with real sugar. Animal studies suggest sugar substitutes may interfere with the body’s natural ability to count calories based on a food’s sweetness. When this calorie-counting ability is skewed, you may consume excess calories. It’s still too early to say there’s a definite link between artificial sweeteners and skewed appetite control. However, there’s no question that regardless of the sweetener you choose, you need to be conscious of the total number of calories you consume whenever you eat or drink sweet things.
Bob's Birthday Messages
As promised in the opening memo, following are excerpts from a small sampling of the birthday cards and letters Bob’s opened to date:
It’s the perfect time to tell you how much I’ve appreciated your analytical clarity, empathy, and dedication. My prostate cancer diagnosis was the most devastating moment of my life, and you pulled me back from the edge of the cliff. Your book and generous counsel put me on the path to successful proton treatment at Loma Linda, where I also learned the principles of a healthier lifestyle. The BOB newsletter and our periodic telephone conversations have kept me informed and on track.
--------------
Friends insisted I read your book. That’s all I needed. Thanks to you, I travel the world making a difference. I give away copies of your book
--------------
From a physician: You changed my life. Thank you for saving thousands of guys just like me.
--------------
I can’t thank you enough for your research and your wonderful books. I would not have known about proton and LLUH without you, my friend. You have enriched my life – perhaps saved it! Savor this day, Bob, thinking about the many lives you’ve touched, and the love and appreciation of us all.
--------------
You’ll never know how much your personal counsel and your book helped me.
--------------
You’ve made the world a better place. Thank you for all you have done for our family
--------------
When I was diagnosed, a friend suggested that I read your book before making a treatment decision. Once my wife and I read your book, the decision was obvious.. (was treated at CA Protons). I will be forever grateful for your efforts to educate patients about their options for treatment.
--------------
I was scared and confused by all the options when I learned two tumors were bulging against the prostate capsule in June 2016. I got several opinions (most recommending surgery). Your book was instrumental in leading me to proton therapy at UF Proton in Jacksonville, FL. I’m grateful and thankful for your efforts that have helped so many people like me. My latest PSA is 0.1 and I don’t even think about it much anymore.
--------------
I was booked for surgery and came across your book. I contacted you and you answered all my emails. You put me in touch with former proton patients in Australia. I chose proton at Loma Linda. I loved the experience along with touring CA and western US.
--------------
From a police chief in the Midwest: Please know how important you have been to countless prostate cancer patients. I believe you and CK saved my life. Your quiet confidence inspired me to choose proton treatment. Thank you and may God bless Bob Marckini. I'll always keep good thoughts of you.
--------------
Without being armed with factual, rational knowledge and insights from your book, I am sure I would have been persuaded to do other than proton therapy. Because of you, I am 100 percent convinced I took the right path. I completed treatment in the spring of 2012 at the Hampton University Proton Therapy institute and have been going great guns ever since. You spoke the truth and I am so happy I followed your advice. Happy BD and thank you for bringing so many more Happy Birthdays to all of us in the BOB. You have my respect, my admiration, and my eternal gratitude.
--------------
I read your book when diagnosed and was considering proton therapy at ProCure in NJ. Your practical guide was invaluable to me. I have tried to always be available as an advocate for others diagnosed with prostate cancer. And I always recommend your book.
And one of our favorites:
Without you I would not be living a full life like I do. Thanks to your book I found out about proton therapy. Since then, I’ve completed two full Ironman triathlons, three Boston marathons, got my instructor’s qualification to teach high-speed driving with the Porsche Club of America, and I’m enjoying a full life with my wife of 47 years. I think you should be nominated for sainthood, and maybe your daughter, too.
Why Loma Linda?
If you’re like most of our members, you had an excellent experience of treatment; your PSA is dropping or has leveled off; and your quality of life is as good as, or maybe even better than, before treatment.
How would you like to show your appreciation to Dr. James Slater, Dr. Jerry Slater, and Loma Linda University Cancer Center for the pioneering work they did to make your treatment possible?
In 1986, the Loma Linda University and Loma Linda University Medical Center Boards of Trustees approved Dr. James Slater’s request to work with Fermi National Accelerator Laboratory (Fermilab) to begin planning the Loma Linda Proton Treatment Center, which would result in the construction of the most expensive piece of medical equipment that had ever been built. The issue was one of the most disputed items the LLUH board would ever deliberate.
In 1989, the year the first particle accelerator (synchrotron) components were shipped to the Loma Linda University Health campus from FermiLab, controversy about the new treatment raged, becoming the focus of a March 17 Wall Street Journal article, Off the Beam? Proton Device to Fight Cancer Is a Boondoggle — or a Breakthrough. The story, while acknowledging that the FDA had approved proton therapy as a cancer treatment, referred to the Loma Linda synchrotron as a “contraption.”
When the Loma Linda University Medical Center Proton Treatment Center opened in 1990, it was the only place in the world to offer proton therapy for patient treatment and research in a hospital setting. It would remain the only hospital-based treatment center of its kind in the United States until 2003.
The realization of Slater’s resolve to ease cancer patients’ suffering was captured in Beam of Hope: The Story of Proton Therapy at Loma Linda University Medical Center, by Richard A. Schaefer. The Wall Street Journal in February 2005, nearly 16 years after a previous article had harshly questioned proton therapy, published an article, Proton-Beam Therapy for Cancer, which listed quality-of-life issues among proton therapy’s most important benefits. Patients in Massachusetts and Indiana were receiving proton therapy at facilities in their states and additional facilities were under construction in Texas and Florida.
Today there are 43 proton therapy centers in the U.S., with several other centers under construction or in development. Two hundred thousand patients have been treated with proton therapy worldwide.
Without the pioneering work of Dr. James Slater, where would we all be today?
So if you’d like to say “thank you” to the late Dr. James Slater and LLUCC for the gift of proton therapy whether or not you were treated at LLUCC, please see below.
Once again, as Winston Churchill said, “We make a living by what we get; we make a life by what we give.”

Giving Options
- Online: Donate here. From the pull-down menu, choose where you’d like to direct your gift —1) Proton Research through the James M. Slater Chair, 2) Proton Research through the Robert J. Marckini Chair, or 3) choose “Other” and specify where you’d like your gift directed in the space provided.
- By Check: Make your check out to “LLUCC.” Specify where you’d like to direct your gift in the memo line — 1) Slater Chair, 2) Marckini Chair, 3) Theranostics, or 4) write “unrestricted” so LLUH can use it where it’s needed most. Mail your check to: LLUH, Office of Philanthropy P.O. Box 2000, Loma Linda, CA 92354.
- By Phone: Call Regina Joseph at 909-558-5010.

5 Surprising Benefits of Walking

One of the most powerful ways to maintain a healthy weight, keep your joints strong, and perhaps even extend your life is also one of the simplest. Walking comes with a host of benefits that can greatly improve your physical and mental health. Following are five that may surprise you.
- Daily walking helps improve your mood. Research has shown that taking a walk every day helps your body release endorphins. Endorphins stimulate relaxation and improve your mood. Walking also increases blood circulation and has a positive influence on your hypothalamic-pituitary-adrenal (HPA) axis. This is a good thing because the HPA is responsible for the body’s stress response.
- A short walk curbs chocolate cravings. A study from the University of Exeter found that a 15-minute walk can cut your chocolate cravings in half and even reduce the amount of chocolate you eat in stressful situations.
- Walking reduces joint pain. Several studies have found that walking reduces arthritis-related pain. Walking just five to six miles a week can even prevent the disease from forming in the first place. Walking protects the joints (especially your knees and hips!) which are most susceptible to osteoarthritis.
- Brisk walking makes you smarter. Research suggests that walking promotes positive changes in white matter – found in the deeper tissues of the brain – in older adults. Regular exercise is also associated with improved sleep and decreased stress, which could also have a positive impact on the brain.
- Walking at a moderate pace boosts immune function. A study of more than 1,000 men and women found that those who walked at least 20 minutes a day, at least five days a week, had 43 percent fewer sick days than those who exercised once a week or fewer. And if they did get sick, it was for a shorter duration and symptoms were milder. One study suggests that the best place to walk is in the woods because being surrounded by nature helps to reduce stress. Research in Japan even showed that walking in the woods may help fight cancer!
hMPV: The 'Most Important Virus You've Never Heard Of'
While cases of COVID-19 and RSV are decreasing, infections linked to another lesser-known respiratory virus are increasing. Human metapneumovirus (hMPV) is in the same family of viruses as RSV, according to the CDC. It causes symptoms similar to the common cold: cough, fever, congestion, runny nose, a sore throat, and shortness of breath. But younger children, older adults, and immunocompromised people are at higher risk of severe disease that could send them to the hospital.
Although we’re entering the summer months and surveillance data show that hMPV tends to be more active in the late winter and spring, it’s surged this year, so it’s important to be vigilant about hand washing.
hMPV spreads just like other respiratory viruses – through droplets from coughing and sneezing, personal contact such as shaking hands, or touching surfaces infected with the virus and then touching the eyes, nose, or mouth.
There are no antiviral medications to treat hMPV, so use over-the-counter pain relievers or decongestants. There are also no vaccines.

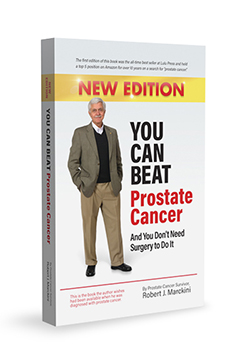
You Can Beat Prostate Cancer: And You Don't Need Surgery to Do It – Second Edition
215 Amazon Reviews
|
As of this writing, there are 215 reviews on Amazon, almost all five-star, and the book is in the No. 2 position on a general search for “prostate cancer” in the books category.
|
 |

Hope for Survival from Prostate Cancer
I listened to Robert Marckini share his amazing experience and research on prostate cancer.
Robert shares his considerable research on the effectiveness of many prostate cancer treatments and discusses them in understandable detail. His research also includes discussions with many men who’ve received proton therapy as well as scientific research comparing proton therapy to other treatments.
I highly recommend this book to every man concerned about prostate cancer…

Was Bob's Book Helpful to You?
If Bob’s book was helpful to you and you’d like to help others find it on Amazon, please write a review. Book reviews help boost the book’s visibility within Amazon’s search results for users looking for information on prostate cancer treatments and/or proton therapy.
Proceeds from book sales are used to help fund our efforts and to support proton therapy research.

Last Month's Brain Teaser
A man puts his bare hand into a pan of boiling water but doesn’t get burned. Why?
Answer: He’s a mountain climber and is on a very high mountain. Water boils at much lower temperatures at high altitude because of the lower air pressure, so he wasn’t burned.
Winner: Here’s a first: Not one member submitted the answer we were looking for! Either the last brain teaser was too complex, or everyone was focused solely on Bob’s birthday. We’ll assume the latter since it took Deb a month to respond to the birthday emails after the May newsletter was issued.
Interestingly, one member who submitted his brain teaser answer directed us to this video of an Indian street chef who’s been dubbed “super hands.” Ram Babu can dip his hands into boiling water without getting burned (or feeling pain)! So, we guess his brain teaser answer, “he must have heat-resistant hands,” is correct!

New Brain Teaser: A Matchstick Puzzle
| Move just two matchsticks to make the dog face to the right instead of to the left. The dog’s tail must stay up. | 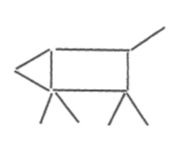 |
Be creative! Think outside the box.
Send your brain teaser answer to [email protected] for a chance to win a signed copy of Bob Marckini’s NEW second edition book, You Can Beat Prostate Cancer.

Getting Old
A distraught senior citizen phoned her doctor’s office. “Is it true” She wanted to know, “That the medication you prescribed has to be taken for the rest of my life?”
“Yes, I’m afraid so,” said the doctor.
There was a moment of silence before the senior lady replied, “I’m wondering, then –just how serious is my condition? Because this prescription is marked ‘No Refills.’”

In Court
“Mr. Clark, I’ve reviewed this case very carefully,” the divorce court judge said. “And I’ve decided to give your wife $1,500 a week.”
“That’s very fair, your honor,” said the husband. “And every now and then, I’ll try to send her a few bucks myself.”

Wrong Email Address
Here’s a lesson to be learned from typing the wrong email address …
A Minneapolis couple decided to go to Florida to thaw out during a particularly icy winter. They planned to stay at the same hotel where they spent their honeymoon 20 years earlier. Because of hectic schedules, it was difficult to coordinate their travel schedules. So, the husband flew out on Thursday, while his wife left the following day.
The husband checked into the hotel. There was a computer in his room, so he decided to send an email to his wife. However, he accidentally left out one letter in her address. Without realizing the error, he sent the email to the wrong person.
Meanwhile, somewhere in Houston, a widow had just returned home from her husband’s funeral. He was a minister who was called home to glory following a heart attack.
The widow decided to check her email, expecting messages from relatives and friends. After reading the first message, she screamed and fainted.
The widow’s son rushed into the room and found his mother on the floor. He then saw the computer screen which read:
To: My Loving Wife
Subject: I’ve Arrived
I know you’re surprised to hear from me. They have computers here now and you’re allowed to send emails to your loved ones. I’ve just arrived and have been checked in. I see that everything has been prepared for your arrival tomorrow. Looking forward to seeing you then! Hope your journey is as uneventful as mine was.
P.S. Sure is hot down here!

Some Trivia
Q: Half of all Americans live within 50 miles of what?
A: Their birthplace
Q: Most boat owners name their boats. What’s the most popular boat name requested?
A: Obsession
Q: If you were to spell out numbers, how far would you have to go until you’d find the letter “A”?
A: One thousand
Q: What do bulletproof vests, fire escapes, windshield wipers, and laser printers all have in common?
A: All were invented by women.
Q: What’s the only food that doesn’t spoil?
A: Honey
Q: Which day are there more collect calls than any other day of the year?
A: Father’s Day

No. 1 Hit Song?
What was the No. 1 song on the day you were born? For Bob, it was, I’ve Heard That Song Before, by Harry James and His Orchestra. The date was April 6, 1943. And the No. 1 movie? There were two – Hello, Frisco, Hello and You’ll Never Know.
For Deb, the No. 1 song on October 16, 1972, was Ben, by Michael Jackson. Watch a very young Michael Jackson sing this song! Interestingly, the song was about his pet rat. The No. 1 movie on Deb’s birthday was Lady Sings the Blues.
Find your No. 1 song here. Find your No. 1 movie here.

Just 100 People on Earth?
What would the world look like if condensed to just 100 people? The current population on earth is around 7.8 billion. For most people, it’s a large figure, that’s all. However, someone has condensed the 7.8 billion into 100 people, and then into various percentage statistics. The resulting analysis is relatively much easier to comprehend.
Out of 100 People:
• 11 are in Europe
• 5 are in North America
• 9 are in South America
• 15 are in Africa
• 60 are in Asia
• 49 live in the countryside
• 51 live in cities
• 12 speak Chinese
• 5 speak Spanish
• 5 speak English
• 3 speak Arabic
• 3 speak Hindi
• 3 speak Bengali
• 87 have clean drinking water
• 13 either lack clean drinking water or have access to only a water source that is polluted
• 75 have cell phones
• 25 don’t have cell phones
• 30 have internet access
• 70 don’t have access to the internet
• 7 received a college education
• 93 didn’t attend college
• 83 can read
• 3 speak Portuguese
• 2 speak Russian
• 2 speak Japanese
• 62 speak their own language
• 77 have their own houses
• 23 have no place to live
• 21 are over-nourished
• 63 can eat full meals
• 15 are under-nourished
• 1 ate the last meal but did not make it to the next meal.
• The daily cost of living for 48 of them is less than $2 (U.S.)
• 17 are illiterate
• 33 are Christians
• 22 are Muslims
• 14 are Hindus
• 7 are Buddhists
• 12 are other religions
• 12 have no religious beliefs
• 26 live fewer than 14 years
• 66 died between 15 – 64 years of age
• 8 are over 65 years old
If you have your own home, eat full meals, drink clean water, have a cell phone, can surf the internet, and have gone to college, you are in the miniscule, privileged lot (in the less than 7 percent category).
Among 100 people in the world, only eight can live to or exceed the age of 65. If you’re over 65 years old, be content and grateful. Cherish life and grasp the moment. You didn’t leave this world before the age of 64 years like the 92 people who’ve gone before you. You’re already the blessed among mankind.
Take good care of your health because nobody cares more for you than yourself! Cherish every remaining moment.
Low PSAs to all,
Bob Marckini and Deb Hickey
Click here for the printable PDF version of this newsletter.
NO MEDICAL ADVICE: Material appearing here represents opin1ions offered by non-medically trained laypersons. Comments shown here should NEVER be interpreted as specific medical advice and must be used only as background information when consulting with a qualified medical professional.