Dear Members (a note from Deb Hickey):
We’re living in challenging times. Back in February, we were all glued to our TV screens as we learned Russia had invaded Ukraine. Three months later, we watched news reports of a mass shooting at an elementary school in Uvalde, TX. We’ve all felt the impact of the continued supply chain disruptions through inflation, smaller quantities of available goods, and longer wait times for purchases. And just when we thought things couldn’t get worse, parts of Florida and the Carolinas, along with several areas in the Caribbean, were decimated by Hurricane Ian.
As with all tragic events, natural and man-made, there are many stories of heroic acts by people in harm’s way, by first responders and others who’ve stepped in to help those affected. Our prayers and heartfelt condolences go out to the victims of these tragedies as well as their family members.
November is the month of Thanksgiving. Despite some of the dreadful things going on in this world, most of us have much to be thankful for—family, friends, faith, a roof over our heads, food on the table, and good health. Thanksgiving is the perfect time to acknowledge all we have. And for me, it’s the time of year I give back to the organizations and charities that mean the most to me. At the top of that list is Loma Linda University Cancer Center.
More than 30 years ago, Dr. James M. Slater pioneered the field of proton therapy at LLUCC. It was a huge risk and a substantial financial commitment for the medical center. To reach that point, Dr. James Slater and his team of physicians, physicists, and engineers had to literally invent ways to image a tumor, deliver, rotate, and focus the beam, and create other new technologies supporting this leading-edge treatment.
Prior to the Loma Linda facility, all proton treatment in the U.S. was being done in physics laboratories using a fixed beam. Today, many of the novel approaches designed by LLUCC are still being built into the newest proton centers around the world.
My life would be drastically different if a visionary physician/physicist and a then little-known Seventh-day Adventist institution in Southern California had not made a very bold decision. Dr. Slater and LLUCC made my father’s treatment possible, and I’m thankful for that every day.
--------------------
Our top news story this month is one of the most exciting I’ve ever read. Richard had advanced prostate cancer – with more than 100 metastatic sites – and was ready to die. Then he underwent a revolutionary treatment that turned his life around.
Also in this issue, find out if syndicated columnist Dr. Keith Roach thinks HIFU is a viable option for treating prostate cancer. Read about two interesting studies – one that found a link between coffee consumption and longer survival rates in prostate cancer patients and another that suggests combining pre-biopsy MRI with PSA testing could provide a big benefit to patients.
Since November 17 is National Testosterone Awareness Day, our Flashback article this month focuses on the frequently asked question – “Is it safe to take testosterone supplements after I’ve had prostate cancer treatment?” In our Member Spotlight section, we include feedback from one member who’s in favor of the potential movement to downgrade Gleason 6 prostate cancer to “pre-cancer” or “non-malignancy” followed by our thoughts. And of course, there’s much more.
As always, we love to get feedback on the newsletter, and welcome any suggestions you have on how to improve the value of the BOB Tales to our members. Just send an email to [email protected].
Deb Hickey
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file. .jpg)
.jpg)
In This Issue:
- Extraordinary Story of Healing ─ Advanced Prostate Cancer
- Is HIFU Ready for Prime Time?
- Coffee Associated with Longer Survival Rates in Prostate Cancer
- Study Shows Benefit of Pre-biopsy MRI in Diagnosing Prostate Cancer
- To ‘T’ or Not to ‘T’ ─ That is the Question
- Member Feedback: Gleason Score 6 ─ Not Cancer?
- Three Ways to Maintain Healthy Weight and Reduce Risk of Prostate Cancer
Extraordinary Story of Healing — Advanced Prostate Cancer
“I’m not much of a people person,” says Richard Humphreys, an educated professional who’s worked all over the world, “That’s just the way I’ve always been.”
Richard was diagnosed with advanced, metastatic prostate cancer that was untreatable by surgery or radiation. His doctors concluded that his only option was androgen deprivation therapy (ADT) – also called hormonal therapy – to slow the progression of the disease and to buy him time.
Some tolerate ADT reasonably well. Others experience moderate effects, which can include a combination of hot flashes and night sweats, weight gain, loss of bone density, body hair loss, loss of muscle mass, breast enlargement, and loss of libido. And some men suffer significant, debilitating, life-altering, intolerable side effects. Richard was in the latter category.
After trying ADT for one year, Richard made the decision to stop, though he knew it would likely end his life. By this time, he was experiencing severe pain throughout his body.
Along Comes Theranostics
Richard’s neighbor is related to a friend of Bob Marckini. The friend, Lori, called Bob late last year and asked if he knew of anything that might benefit Richard.
Coincidentally, Bob had recently learned from Dr. Richard Hart, President of Loma Linda University Health, of LLUH’s major commitment to an incredible technology called “theranostics” for treating advanced cancers, including prostate. We wrote about this revolutionary technology in our May and December 2021 BOB Tales newsletters.
Bob spoke with Richard and told him about this new and emerging technology at Loma Linda that might benefit him. He was excited about the prospect of trying theranostics, so Bob introduced him to Dr. Frankis Almaguel, director of the theranostics program at LLUCC. “When I first spoke with Dr. Almaguel,” Richard tells us, “my PSA was in the thousands!”
Dr. Almaguel arranged for a Ga-68 PSMA PET/CT scan for Richard and determined that he’d be an excellent candidate for theranostics and would likely require three or four treatments.
“My skeletal system lit up on the PET scan like a Christmas tree,” Richard says. “I had well over 100 metastatic sites throughout my body.”
Three Treatments with Extraordinary Results
In January of this year, Richard had his first treatment. During the first infusion doctors injected a radionuclide designed to identify the precise locations of all the lesions in his body.
Then came a second infusion – this one with a different, and much more powerful, radionuclide designed to travel to each of these locations and destroy the lesions without damaging adjacent healthy organs and tissues.
Before Richard knew it, the uneventful and painless treatment was over, though certain procedures were followed after treatment to flush the materials out of his body.
A follow up PET/CT scan showed that more than 80 percent of the lesions were gone. A couple days later, Richard reported that all of his pain was gone. He was elated.
Richard’s second treatment was in early March, and it was much like the first. A follow up PET/CT scan showed more than 90 percent of the lesions were destroyed. Once again, Richard was thrilled. A couple months later, he had his third treatment.
Cancer Free?!
After completing his third treatment, Richard is convinced he’s cancer free. “I feel wonderful,” he reports, and I have a whole new lease on life. Another scan is planned, but he’s not concerned. “I know I’m cancer free,” he says.
Richard reports that he experienced extreme dry mouth and a loss of taste and smell during treatment, but it was temporary. Today he feels “terrific” and has no lingering side effects.
Getting on with Living
Richard lives with his wife, Margot, in Sequim, WA. His home is next to an airport runway which is quite convenient for Richard, a private pilot. He has recently resumed work on one of his pet projects – restoring a 1929 Waco taper wing biplane. He’s rebuilding the engine and hopes to have the plane in the air soon.

Richard met with one of his doctors recently who told him, that if he hadn’t had theranostics treatment after stopping ADT, he probably wouldn’t be alive. No one really knows if this is true. What is true, however, is that Richard really does have a new lease on life and he wants to give back in any way he can. “If that means becoming a spokesman for the miraculous benefits of theranostics treatment, then I’m your man,” he says.
In addition to rebuilding his old plane, Richard spends much of his time volunteering at a hospice center, ministering to the ill and the elderly, and helping terminally ill patients. “I find it very rewarding to bring these people comfort,” Richard says.
That’s not bad for someone who says he’s not much of a people person.
Not for Everyone
One might ask, “If two or three infusions of theranostic compounds can be used to search out and destroy metastatic prostate cancer so quickly, then why not treat early and mid-stage prostate cancer the same way?” And for that matter, why not treat all cancers with this exciting, new technology?
The fact is, our explanation of theranostics treatment above fails to put into proper perspective the intricacies and complexity of this extraordinary technology. Treatment is limited – for the most part – to advanced cancers where the patient has no other options.
What’s Next?
Considerable research and development is necessary to custom design/develop radionuclides that can deal with a wide range of cancers, and this is precisely the objective of those involved in the design, construction, and staffing of the new, state-of-the-art, theranostics research and treatment center at LLUH. It’s also the reason we’re encouraging our members to help support this effort by making contributions to LLUH so that more people like Richard Humphreys can have a new lease on life.
It’s our hope and expectation that theranostics will be used someday to treat a broad range of cancers at all stages. We have no doubt that the new theranostics research and treatment center at LLUH will be at the forefront of these developments.
We’ll provide an update on theranostics in future BOB Tales newsletters.
Is HIFU Ready for Prime Time?
HIFU (pronounced HIGH-foo) is a technology that destroys cancer by heating it with sound waves. It’s promoted as a minimally invasive treatment for prostate, liver, and lung cancer. The procedure can take up to four hours and is typically done on an out-patient basis. When treating prostate cancer, HIFU requires the insertion of a Foley catheter which the patient must wear for up to four weeks.
Bob Marckini wrote about HIFU in the new edition of his book (Chapter 6: Investigating Treatment Options). He interviewed several patients who had undergone HIFU for prostate cancer and found that results were mixed. Some had excellent results and were happy with their treatment decisions, while others reported urethral strictures, urinary complications, recurrences, and loss of or reduction in sexual function.
Bob concluded that although HIFU shows promise; it’s highly practitioner dependent; and seems to carry an inordinate risk of life-altering side effects.
Dr. Roach’s Opinion
Syndicated columnist Dr. Keith Roach weighed in on HIFU last month. A patient reported that he’d recently been diagnosed with prostate cancer with a PSA in the 40s, and that his urologist had recommended HIFU. According to the patient, the urologist told him that HIFU does an excellent job killing prostate cancer and it “wouldn’t have any of the side effects from the ‘standard,’ surgery.”
Dr. Roach responded by explaining how HIFU works and said, “This may eventually become a standard treatment for localized prostate cancer, but as of yet, there isn’t strong evidence to support its use.” He also said that his urologist exaggerated if he suggested there would be no risk of side effects because, “44 percent of men (who choose HIFU) have sexual troubles; 17 percent have obstructions, 12 percent develop a stricture in the urethra, and 8 percent develop urinary incontinence after HIFU.”
Roach further stated that although the FDA has approved HIFU for the destruction of prostate tissue, it hasn’t approved the procedure explicitly for treating prostate cancer.
Finally, he noted that while HIFU is reasonable as an option for salvage therapy, he wouldn’t recommend it for treatment in this case.
► BOB Comment: Dr. Roach must have read the new edition of Bob’s book! We agree with his conclusions.
Coffee Associated with Longer Survival Rates in Prostate Cancer Patients
A new study found an association between a specific genotype and longer survival rates in prostate cancer patients. The genotype, which is associated with fast caffeine metabolism, is called CYP1A2 AA.
Coffee contains active compounds that lower inflammation and according to some research, drinking several cups of coffee every day may be linked to a lower risk of developing prostate cancer. However, few studies have looked at whether coffee consumption or the impact of caffeine metabolism genes can affect the risk of cancer progression among men who’ve been diagnosed with prostate cancer.
Researchers at the University of Texas MD Anderson Cancer Center sought to examine the association between coffee consumption, caffeine metabolism genotype, and survival among thousands of men with prostate cancer.
The study included data for 5,727 prostate cancer cases across seven studies. Patients (median age, 63 years) included those on active surveillance, those who underwent treatment, and some who had metastatic prostate cancer. They were all asked about their food and drink consumption.
The researchers compared levels of coffee consumption. Those who drank two or more cups of coffee per day were considered “high intake,” while those who drank three or more cups per week were considered “low intake.”
Results showed high intake coffee consumption was associated with longer prostate cancer-specific survival among patients who had the CYP1A2 AA genotype.
Dr. William Dahut, chief scientific officer for the American Cancer Society, said what he took away from the study was that if a coffee drinker is diagnosed with prostate cancer, there’s no reason to stop drinking coffee and there may be some benefit. He continued, “There’s at least a theoretical reason why it’s helpful, but there’s not enough information out there for us to say, ‘If you have prostate cancer, you need to start drinking coffee’ either.”
The study’s findings suggest that coffee intake is likely associated with longer prostate cancer-specific survival in certain groups, but more research is needed to fully understand which patients may benefit.
Study Shows Benefit of Pre-biopsy MRI in Diagnosing Prostate Cancer
Results from a new study suggest that combining pre-biopsy MRI with PSA testing could prevent biopsy in more than 88 percent of patients without prostate cancer.
The PSA test has been widely used to evaluate the possibility of prostate cancer. However, PSA alone isn’t an effective tool for detecting prostate cancer as PSA increases not only in prostate cancer, but also in the presence of benign prostatic hyperplasia (BPH) or prostatitis.
Researchers sought to assess the diagnostic performance of PSA testing with adjunctive MRI to better predict prostate cancer in patients with PSA levels lower than 20 ng/mL.
For the study, 881 patients had a pre-biopsy MRI and PSA test due to suspicion of prostate cancer. Of those, 220 were diagnosed with prostate cancer and 162 had clinically significant disease. For clinically significant cancer, researchers found the combination of pre-biopsy MRI and PSA testing had a significantly higher positive predictive value than a PSA level greater than or equal to 4 ng/mL alone. They also found that adding MRI to PSA testing resulted in more than triple the specificity rate for detecting clinically significant prostate cancer.
We’ve been producing BOB Tales newsletters for more than 20 years. During this time there have been articles that many new members haven’t seen, and some older members may have forgotten. So, we periodically re-run articles from past newsletters. The following is from February 2017.
To 'T' or Not to 'T' — That is the Question
As mentioned in our opening memo, November 17 is “National Testosterone Awareness Day.” How do they come up with these things?
Over the years, many members have asked if they should take testosterone supplements after their prostate cancer treatment. And if so, is it safe?
In addressing this question, we must remind you that we aren’t physicians and can’t give medical advice. We can tell you only what we’ve heard or read on this subject.
There seems to be differing opinions among physicians on this. Some say testosterone can promote prostate cancer growth and should never be taken after prostate cancer treatment. Others say, five to 10 years after treatment, men may begin taking testosterone supplements, but they should continue to monitor their PSA closely. One oncologist we spoke with supports this practice, but also suggests that men maintain testosterone levels in the lower half of the normal range.
One of our members wrote to us recently on this subject. He said he was treated 12 years ago and his PSA reached a nadir of 0.6 and stayed there for several years. Last year, as a result of a physical, he learned he had some bone loss. His urologist recommended a testosterone supplement. Two months later his PSA rose to 0.9 ng/mL. And at four months it was 1.2 (double his nadir). He stopped the testosterone and his PSA came back down.
We spoke with an oncologist about this, and he wasn’t surprised with the result. This doctor is opposed to taking testosterone after prostate cancer treatment.
Bottom line: The jury is out on whether or not it’s safe to take testosterone supplements after prostate cancer treatment. It might make sense, however, to fail on the safe side and avoid testosterone supplements.
We encourage you to talk with both your urologist and your oncologist if you’re considering taking testosterone supplements.
'My Cup Runneth Over'
BOB member Bud Ralston was diagnosed with prostate cancer in August 2010. “The call put me in a daze,” said Bud. “When you hear the word ‘cancer,’ it gets your attention.”
Bud’s urologist recommended surgery. “I was naïve and uninformed,” Bud said. “All I knew was that I had cancer. I wanted it out. And since he was ‘the expert,’ I trusted his advice.”
Since there’s always a risk of bleeding with any surgery, in preparation for his prostatectomy, Bud had to withdraw from his blood thinner, Warfarin, which he was taking for an artificial heart valve. As a result, he suffered a TIA, also known as a “mini-stroke,” and his treatment had to be canceled.
The Path to Protons
“Then the real hunt began,” said Bud. He read everything he could find about prostate cancer and treatment options. He also called every friend he knew who’d been diagnosed with the disease.
Bud spent many weeks reviewing the pros and cons of every treatment option he found, but wasn’t confident in any of them. “I didn’t find anything about proton therapy at the time, so it wasn’t even on my radar,” said Bud.
“It was a confluence of circumstances that brought me to proton therapy and Loma Linda University Cancer Center,” Bud said. “I think I had a guardian angel looking out for me.”
While attending a funeral in California – Bud lived in Hawaii at the time – he ran into a friend who told him his brother had just started “something called proton therapy” for his prostate cancer at LLUCC. “Apparently his brother was singing proton’s praises and that had me intrigued,” said Bud. “And then he told me to check out the Brotherhood of the Balloon for more information.”
After reviewing the BOB website and reading Bob Marckini’s book, You Can Beat Prostate Cancer, Bud made the decision to fly to Loma Linda.
During his visit, Bud attended a patient orientation meeting; connected with his medical insurance provider about treatment coverage; found a two-bedroom condo that catered to patients at LLUCC; arranged for a rental car from a company that also catered to patients; got measured for his immobilization pod; and received a treatment start date for the last week in December 2010.
“I was so impressed with the Loma Linda proton facility, the staff, and the ‘Make Man Whole’ program they offered,” said Bud. “And my treatment was a breeze.”
While in treatment, Bud played golf three to four times a week and participated “fully” in the many support activities offered at LLUCC. “I also formed lasting friendships with a wonderful group of men that were all in the same boat as I,” Bud said.
Feeling Lucky
Today, Bud appreciates how “lucky” he is and says he leads a wonderful life. He moved to Gig Harbor, WA in 2019 where he and his high school sweetheart Kathy share a beautiful home overlooking the harbor entrance. Together they watch the tides and seasons change, the mariners sail their boats in and out, and the many birds and animals that are native there.
Bud golfs two-three times a week and spends the rest of his time fulfilling his photography passion. “I have a constant desire to see and record the wonders around me,” Bud said. He travels all over the world taking photos. He’s been to Canada, England, Norway, Denmark, Estonia, Germany, Scandinavia, Russia, Finland, Kenya, Hungary, Austria, Slovakia, and Sweden. Closer to home, he’s taken photographs at Yellowstone, Grand Tetons, Yosemite, and Lake Clark National Park.
Bud’s traveling to Fairbanks, AK this winter for the aurora borealis, Iceland next summer for its waterfalls and volcanoes, and Costa Rica soon after that for its mangrove-lined waterways, mountain jungles, and hundreds of species of rare and beautiful birds.
“I’m genuinely grateful for the proton beam treatment that gave me these ‘bonus years’ to truly enjoy life – my love, my friends, and the many wonders of nature,” said Bud. “For those who get a diagnosis of prostate cancer, I hope they know it’s not a death sentence! I recommend they hold their heads high, read Bob Marckini’s book, and go to Loma Linda for a golf vacation.”
“My cup runneth over!”
What’s His Urologist Think?
“When I returned to my urologist for a follow-up exam six months after my proton treatment ended, he was amazed at my numbers and the smoothness and shrinkage in my prostate,” said Bud. “When I told him I had proton therapy, he’d never heard of it!”
Bud says he has strong feelings about urologists who recommend surgery without advising their patients to weigh all the options before making a decision. He has a good friend who went to his same urologist for a prostatectomy the week before Bud’s surgery was originally scheduled. His friend is still wearing diapers.
► BOB Comment: You can see samples of Bud’s photography here. You won’t be disappointed!
Member Feedback: Gleason Score 6 — Not Cancer?
In our September BOB Tales, we told you about a potential movement to downgrade Gleason 6 (Grade Group 1) prostate cancer to a “pre-cancer” or “non-malignancy” stage. Dr. Scott Eggener, an associate professor of surgery and urologic oncology at the University of Chicago Medicine, proposed this prospect be considered in an article, “Low-grade Prostate Cancer: Time to Stop Calling it Cancer,” published in the Journal of Clinical Oncology April 18, 2022.
Last month, we received lots of feedback from members who don’t support declassifying Gleason 6 prostate cancer as “cancer.” Most were concerned it could do a disservice to men whose disease could progress from Gleason 6 to a more aggressive variant without close monitoring or treatment.
This month, a member wrote in support of the movement. An excerpt from his message is below.
A cancer diagnosis scares the heck out of those who are uninformed. This fear has driven upwards of a million men to have their prostates removed … when a major portion of them was unnecessary.
This happens because they don’t understand there’s a huge range of prostate cancers that need to be addressed individually rather than an aggressive “one size fits all slash-and-burn” approach.
To help consumers identify the lowest grade, indolent, non-metastatic disease, there’s a crying need for a better descriptor. The devil is in the details. To defuse the argument that doing so will lull the consumer into complacency, the name should clearly identify an irregularity without the heart pounding generic prostate cancer diagnosis. For me, those words caused many sleepless nights.
I think the term “pre-cancer” is on the right track, but we should explore other possibilities that will reduce the likelihood of patients overreacting while motivating them to pay attention to a condition that needs to be watched.
─BOB Member, Cordova, TN
► BOB Comment: We have some very smart members, don’t we? This member makes some good points. Nevertheless, we still disagree. We feel we could be doing more harm than good by “sugar-coating” the term we use for Gleason 6 prostate cancer. Calling it “pre-cancer” or a non-malignancy as has been proposed. Gleason 6 prostate cancer isn’t necessarily “indolent,” and it could someday develop into something more serious. Also, many urologists are still using the old “blind biopsy” technology, which often misses more aggressive cancers. Even the significantly improved MRI-guided fusion biopsy can miss aggressive cancers. So, until our imaging, biopsy, and diagnostic technologies can clearly identify those cancers that are truly indolent, we should continue calling Gleason 6 tumors “prostate cancer.”

Thanksgiving
It’s nearing the end of the year, a time when many of us make gifts to our favorite charities. There are so many worthwhile causes, it’s often hard to choose which ones to support, but for Bob and Deb, one choice is easy. Loma Linda University Health (LLUH) saved Bob’s life and preserved the quality of his life. We couldn’t be more thankful.
LLUH pioneered proton therapy 30 years ago at great financial risk, and at a time when protons were being generated and used only in physics laboratories. Today, thanks to their efforts, proton therapy is a proven technology and is growing exponentially with 43 proton centers in the U.S., 50 more around the world and many more in the works.
Further justification for our financial support is the fact that Loma Linda University Health is an extraordinary institution treating thousands of patients annually with leading edge medical technology in just about every medical specialty. And that includes theranostics, an incredibly powerful cancer-fighting therapy.
Over the next five years, LLUCC will make a significant investment to exponentially expand access to this extraordinary field. As you plan your year-end giving, please consider making a gift to the theranostics program.

Giving Options
Online
From the pull-down menu, choose where you'd like to direct your gift — 1) Proton Research through the James M. Slater Chair, 2) Proton Research through the Robert J. Marckini Chair, or 3) choose "Other" and specify where you'd like your gift directed in the space provided.
By Check
- Make your check out to "LLUCC."
- Specify where you'd like to direct your gift in the memo line — 1) Slater Chair, 2) Marckini Chair, 3) Theranostics, or 4) write "Unrestricted" so LLUH can use it where it's needed most.
- Mail your check to: LLUH, Office of Philanthropy P.O. Box 2000, Loma Linda, CA 92354.
By Phone
- Call Regina Joseph at 909-558-5010.
Three Ways to Maintain Healthy Weight and Reduce Risk of Prostate Cancer
Maintaining a healthy weight is critical to men’s overall well-being and longevity. It’s also important in the prevention of prostate cancer as studies have linked obesity and excess abdominal fat to a greater risk of the disease.
“Excess weight parallels the risk of prostate cancer during the aging process,” says Andrew Woodward, MS, RD, CSO, an oncology nutritionist at Loma Linda University Cancer Center. “Many people think weight gain is inevitable as they age, but that’s not the case. Instead, it requires becoming more intentional about physical activity and slowly reducing caloric intake to compensate for aging and sluggish metabolism.”
One way excess body fat raises the risk for prostate cancer is through its production of cortisol, the body’s main stress hormone that increases inflammation in the body. Over time, inflammation can cause DNA damage and lead to cancer.
Insulin also helps explain the link between excess abdominal fat and prostate cancer as it increases cell production and reduces cell death. This creates more of an opportunity for something to go wrong and cancer to develop.
Below, Woodward outlines three key ways to maintain healthy weight and decrease the risk of prostate cancer.
1. Replace Starches with Vegetables
Replacing one serving of a starchy food with a serving of vegetables can significantly reduce the number of calories consumed. One way to do this is to try vegetables prepared to mimic starches, like cauliflower rice or noodles made from zucchini.
2. Keep a Food Journal
Growing an awareness about eating habits is one of the first steps toward identifying areas for improvement. For example, logging types, amounts, and timing of food consumption can reveal a “mood-food connection,” Woodward says. Stress eating is real! In times of emotional turmoil, you may crave the calming effects of carbohydrates. Through a set of biochemical processes, amino acids from carbohydrates eventually convert into serotonin which regulates your mood.
3. Eat Plant-based Foods
We’ve written dozens of articles about the benefits of eating plant-based foods, so you probably already know that we (and Woodward) recommend sticking to a primarily plant-based diet. Many fruits and vegetables are rich in phytochemicals, compounds that help fight cancer.
You should also limit your intake of processed foods, sugar, and fatty foods. Studies have shown that a high consumption of these foods lead to higher risks of prostate cancer compared to a diet rich in fruits and vegetables.
Woodward recommends speaking with your doctor – or finding a trained nutritionist – if you plan to significantly change your diet.

Time to Get a Flu Shot
Long-term fever, muscle aches, sore throat, runny or stuffy nose, cough, headache, and fatigue. These are just a few of the symptoms people can experience with the seasonal flu. But there’s something we can do about it.
Each year the World Health Organization studies flu virus samples from around the world and makes a recommendation on a specific vaccine to protect against the virus they predict will circulate during the upcoming year. The CDC reports that the flu vaccine reduces the risk of flu illness by up to 60 percent. It can also reduce the severity of illness for those who do get sick after having been vaccinated.
Doctors recommend the flu vaccine for everyone ages 6 months and older. The vaccine is especially important if you’re at high risk for flu-related complications. People in this category are typically adults over 65 and others with certain chronic medical conditions such as asthma, diabetes, or heart disease.
Check with your doctor to see if the flu vaccine is right for you.

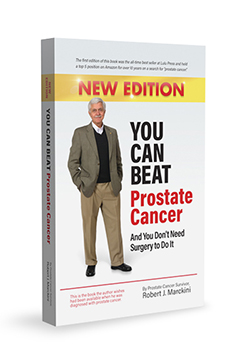 You Can Beat Prostate Cancer: And You Don’t Need Surgery to Do It – Second Edition
You Can Beat Prostate Cancer: And You Don’t Need Surgery to Do It – Second Edition
180 Amazon Reviews
As of this writing, there are 180 reviews on Amazon, almost all five-star, and the book is in the No. 2 position on a general search for “prostate cancer” as well as a search in the “books” category.
Following is a recent review:

Study Your Options: After I was diagnosed with prostate cancer, I researched all of my options for treatment. While doing my research, my sister asked if I had looked at proton therapy. After reading You Can Beat Prostate Cancer, I made the choice to have proton therapy. My choice was to go to Loma Linda for treatment. By the time insurance approved treatment, Seattle had a center for treatment. Because of the book, I feel I made the best choice. Thank you, Bob, for helping me with my research.

The Personal Side
We received a lot of positive feedback on the series we ran over the past year on Chapter 18 of Bob’s book, “The Ten Steps for Taking Control of the Detection and Treatment of Your Prostate Cancer.” But what about the personal and emotional side of treatment?
The Personal Side of the Treatment Experience
Much of Bob’s book is dedicated to explaining his research and due diligence efforts, including understanding the technology surrounding each of the treatment options. He also gave readers some insight into the personal and emotional side of dealing with prostate cancer, including events leading up to the first treatment. Some readers have told us the personal stories played a large part in putting their minds at ease, especially some of the humorous events described in the book. The following excerpt is from Chapter 9, “My Treatment Begins.”
A Warm California Reception?
My wife and I flew to California on Tuesday, Oct. 24, 2000, to get settled in our new temporary apartment. We landed in Los Angeles, picked up our rental car, and drove east toward Loma Linda. Traffic was horrific, and the 70-mile trip lasted almost three hours. We arrived at Redlands about 9 p.m., parked the car, and carried our gear up to our second-floor apartment. Somehow, I managed to sprain my back in the process. It was hot – about 85°F – and the air conditioning in our new apartment was broken. Not a great start.
The next morning there was a nasty note on the windshield of my rental car reminding me that I parked in the reserved space of another tenant. How was I to know the spaces were reserved?
We’d been there less than 24 hours; we experienced a horrible traffic jam; I sprained my back; our air conditioning didn’t work; and I managed to “tick-off” one of my new neighbors. A bad omen?
Treatment Number 1
My first of 38 treatments was on Wednesday, Oct. 25, 2000, at 1:30 p.m. Pauline was invited to observe. This both surprised and delighted me. Despite all my research, I really didn’t know what to expect that first day, and neither did my wife.
My instructions were to consume 16 ounces of water about 20 minutes before the procedure in order to fill my bladder. This helps to stretch the bladder and lift it off the prostate and out of the range of the proton beam. I dutifully complied and drank the water.
Tip: Drink the water. The bladder and prostate are somewhat like a hot air balloon sitting on top of a passenger gondola. When the hot air balloon is full of warm air, it lifts and rises off the gondola.
We were escorted to a changing room where I was told to disrobe and put on a hospital johnny. I could leave my socks on. Somehow that comforted me – but I don’t know why. Pauline joined me in the changing room, to provide company and encouragement. A few minutes later, the door to the changing room opened and the previously treated patient, dressed in his johnny, entered – a slightly awkward moment with Pauline there. It was time for my first treatment.
Pauline and I walked down the corridor and entered Gantry 3. We were greeted by three radiation therapists – Tim, Nick, and Barbara, all beaming with welcoming smiles. I remember thinking, “Sure – it’s easy for them to smile – I’m the one having 250 million electron volts shot into my private parts.”
I was asked to climb into my pod, which had already been installed on the gantry treatment table. “How do you know this is my pod?” I asked. They told me my name was written on it and it was bar coded. The bar code was scanned into the computer in the gantry control room.
Pinching the back of my johnny to hold it closed, lest I show three strangers my best angle, I gingerly climbed into the pod. The smile on the lead therapist’s face told me that perhaps everybody is modest at first. Later, I would find myself bounding into the pod with an untied johnny flapping in the breeze and my “better side” fully exposed for all to see.
The pod fit perfectly, almost like it was made for me – but then, it was.
I was asked to roll over on my left side and was presented with my first “official” balloon – not so bad, but a little embarrassing in front of my wife, especially when they filled it with water from two syringes.
As instructed, I rolled onto my back again and they made an initial adjustment to my position in the pod by tugging on the sheet under me. I was conscious of the water-filled balloon in its “resting place.” It felt a little unnatural at first, but not uncomfortable.
Next, the pod and platform assembly was slid to the center of the treatment apparatus, and the entire 94-ton gantry began to rotate in order to position the low-energy X-ray equipment above me. At first, I had the sensation that my pod was rotating, and the room was stationary. I found myself hanging on so I wouldn’t fall out. I quickly adapted to that phenomenon.
So, there I was 3,000 miles from home, at a hospital in Southern California, lying in a pod, a water balloon in my butt, a sheet covering me, cantilevered into the center of a three-story high, white, cylindrical 94-ton gantry, with two radiation devices pointed at my pelvic region, about to have billions of protons shot into my prostate. I remember thinking, “What the hell am I doing here?”
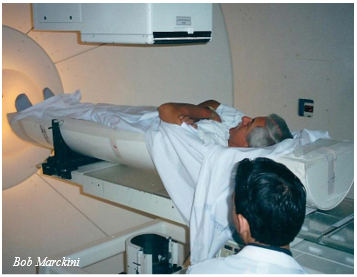
At this point Pauline broke down and cried. It seemed to hit her all at once: My diagnosis with prostate cancer; all the research, the phone calls, a two-month move to California; my lying helplessly in this “coffin-like” device, surrounded by hospital technicians dressed in white; and this giant “Star Wars” machinery rotating around me. She was suddenly struck with thoughts of the mortality of her partner and best friend of 35 years. Death was something we never discussed, or even thought about, because we considered ourselves young, healthy, and physically fit.
To be continued next month …

Did Bob's book help you?
If Bob’s book was helpful to you and you’d like to help others find it on Amazon, please write a review.
We’re happy to discount books in quantity to anyone who is interested in spreading the word on proton therapy. Just send an email to [email protected].
Proceeds from book sales are used to help fund our efforts and to support proton therapy research.
National Proton Conference
Elevating Access, Research, and Innovation in the Field of Particle Therapy
The 2023 National Association for Proton Therapy (NAPT) conference will be held in Salt Lake City, UT, May 6-9. The annual conference brings together leaders in the field of particle therapy with a robust agenda focused on emerging clinical research, operational efficiencies, insurance authorizations, and a special session presented by PTCOG-NA.


Last Month’s Brain Teaser
Place the numbers: 1, 2, 3, 4, 5, 6, 7, 8, 9, one in each box so that all rows, columns and diagonals add up to different totals.

Answer:
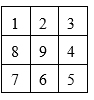
Winner:
BOB member Mike Savage is the October BOB Tales brain teaser winner.
Mike, who lives in Wheaton, IL, was diagnosed with prostate cancer in 2013. Lucky for him, his urologist was well educated and told him he’d be a good candidate for proton therapy. “That sounded very appealing to me,” said Mike. “It sounded much better than surgery, so I jumped at the chance.”
While waiting for his treatment to begin, read Bob Marckini’s book, You Can Beat Prostate Cancer. “It gave me comfort in my treatment choice,” said Mike. “In fact, I was so impressed with the book, I bought additional copies and sent them to my adult son and three younger brothers.”
Mike was treated at the Northwestern Medicine Proton Center in Warrenville, IL in early spring 2014. “As an extra bonus, I was told I was eligible to get into a treatment regime consisting of about half the number of treatments as the standard protocol,” said Mike. “In a little over a month, my 28 treatments were complete.”
The highlight of Mike’s experience at the proton center was getting to know the exceptional doctors, nurses, and other staff members. “To say they were professional, caring, considerate, and personable would be an enormous understatement,” said Mike. “I’m sure they experience considerable strain and perhaps some sadness working with cancer patients day in and day out, but they never let it show.”
“Now on to the happy news,” Mike said. “The results of my proton therapy are spectacular. My PSA dropped immediately and has remained near zero ever since. The other good news is that I had little, if any, side effects. I’m happy to report my ‘tattoo dots’ are the only tangible reminders of my treatment.”
At 75, Mike is retired and enjoying life with his wife Martha, two grown children, and seven grandchildren. He also spends time with friends and his church community.
Prior to Mike’s retirement, he spent almost 25 years as an Air Force officer, serving as a B-52 crewmember, Air Force Academy instructor, R&D project manager, Pentagon action officer, and as an R&D liaison between the UK MOD and offices under the Secretary of the Air Force. He then worked in Knights of Columbus financial programs and finished as a high school chemistry teacher.

“I’m looking forward to many more years of high times and low PSAs,” said Mike. “Best wishes for the same to all!”

New Brain Teaser
It takes a clock two seconds to strike 2 o’clock. How long will it take to strike 4 o’clock?
Hint: It may not be as obvious as it first appears.
Send your brain teaser answer to [email protected] for a chance to win a signed copy of Bob Marckini’s NEW second edition book, You Can Beat Prostate Cancer.

Locked Out?
Three guys walk out of a restaurant to their car and realize they locked the keys inside.
One of them says, “Get me a wire coat hanger; I’ll straighten it out, snake it in and unlock the door.”
The second one says: “Hold on. If we do that, someone will think we’re stealing the car.”
The third guy says: “Look, we’d better do something quick, it’s starting to rain, and we left the top down.”

Reflections for Old Folks
You drop something when you were younger, you just pick it up. When you’re older and you drop something, you stare at it for a bit contemplating if you actually need it anymore.
One thing no one ever talks about when it comes to being an adult, is how much time we debate keeping a cardboard box because it’s, you know … a really nice box.
I’m in a Walmart parking lot watching a woman who can’t remember where she parked. Every time she holds her key fob in the air, I honk my horn.
At my age, rolling out of bed in the morning is the easy part. Getting off the floor is a whole other story.
I may not have lost all my marbles yet, but there’s a small hole in the bag somewhere.
If a cookie falls on the floor and you pick it up, that’s a squat, right?
I can’t believe I forgot to go to the gym today. That’s seven years in a row!
I’ve been watching my weight. It’s still there.
It’s fine to eat a “test grape” in the produce section, but take just one bite of a rotisserie chicken, and it’s, “Sir, you’ll need to leave.”


Consumer Alert: Water on Candles
Americans spend $3.2 billion on candles every year and during the holiday season, scented candles are one of the most popular decorations. But before you hit up the local Yankee Candle, make sure you know how to safely extinguish candle flames and fires.
Simply put, water and hot burning wax don’t mix. If you try to put out a candle flame or fire with water, the reaction creates a massive fireball. Even just a small amount of wax
and water can create a dangerous wax fire.
The best way to put out a candle is to blow it out or put a lid on it.
There are several videos on YouTube that show what happens when water is thrown on burning wax. The flames can shoot out and up, some reaching more than six feet in the air.
Watch what happened to a CBS anchorwoman from Texas who poured a cup of water into a candle jar in her kitchen.
The National Candle Association also suggests the following …
- Don’t leave a burning candle unattended.
- Don’t burn a candle all the way down.
- Don’t move a candle while it’s burning.
- Don’t move a container with hot melted wax.
Stay safe this holiday season, everyone!

Be Cyber Aware
Last month was Cybersecurity Awareness Month – a great time to review good tech habits with your family and friends. The following information was sent to us by BOB member Bernie Picchi, who’s managing director for Private Wealth Management at Palisade Capital Management.
According to the FBI, “Internet-enabled crimes and cyber intrusions are becoming increasingly sophisticated, and preventing them requires each user of a connected device to be aware and on guard.” While it may seem more likely that older people primarily fall prey to cyber scams, young adults who are just starting out can also be prime targets.
Don’t get scammed.
Scammers are more sophisticated every day, making it increasingly difficult to distinguish between legitimate communications, phishing, and “smishing.” Do not respond to alerts, emails, texts, or phone calls asking for confidential financial information, gift cards, or money. If you are unsure whether a communication is genuine, contact the sender directly through an official website email, chat function, or known phone number.
Don’t transact in public.
Using publicly available Wi-Fi provides opportunities for thieves to obtain your personal information. This risk goes up significantly when you transmit sensitive financial information, such as your credit card or bank account number, or other personal identifiable information (PII) such as your social security, passport, or driver’s license number over these networks. Always use your phone’s internet hotspot or wait until you are at home on your own protected, secure network to pay bills or make purchases.
Keep your network secure.
Make sure all your devices are up to date with the latest software and operating systems. Install strong, well-reviewed anti-virus software on your computer and timely follow prompts when asked to install applicable updates.
Use strong passwords. 
Always use strong passwords that cannot be easily guessed to help reduce the chance of cyber theft. Consider using randomly generated passwords stored in a reputable password management vault to securely store your passwords. Do not reuse passwords across multiple websites or platforms. Do use multi-factor identification (i.e., a secondary text or app code), when possible, to add an extra layer of protection against unwanted access. Passwords should be periodically updated for optimal security.
Taking proactive steps and using common sense can help significantly reduce the risk of cybercrime.
.gif)

Thank You
Each year in our November issue of BOB Tales, we like to give thanks to the people and organizations that help us with our mission. Without you, this “ministry” wouldn’t exist.
Thank you, our members, for your devotion to “the cause,” for sharing with others your knowledge and passion for proton therapy; for the constant feedback and messages of gratitude; for the news stories and information you think may be of interest to us and to others; for all the questions you ask on behalf of family members and others; for those who have volunteered to help newly diagnosed men and their family members who haven’t found their way; for the You Can Beat Prostate Cancer books you buy in bulk and your offer to pass them along to others; for forwarding the newsletter to those who may find it valuable; and for your ongoing generosity through gifts for proton research.
Thank you, Dr. James M. Slater, Dr. Jerry Slater, and Loma Linda University Cancer Center, for pioneering proton therapy for prostate cancer and other diseases 30-plus years ago so that tens of thousands could have their cancers cured and the quality of their lives preserved. Thank you also for your support of the Brotherhood of the Balloon, your encouragement, and your unwavering faith in our mission.
Thank you, LLUCC senior management, for your support of our efforts in so many ways.
Thank you, all the proton centers, for acknowledging the significant benefits of proton therapy, for making the capital investment to build 40-plus proton centers in the U.S. and for enabling thousands more patients to benefit from this technology.
Thank you, Jennifer Maggiore and the National Association for Proton Therapy, for building awareness and educating others about proton therapy; for your support of our organization; and for being a valuable resource.
Thank you, Dr. Nancy Mendenhall at the University of Florida Health Proton Therapy Institute, for tirelessly leading the effort on the COMPPARE trial comparing proton therapy to IMRT for prostate cancer. Thank you also to the stakeholders, physicians, scientists, statisticians, advisers, and patients, for making this study possible.
Thank you, all the physicians and administrative people connected with proton therapy, for routinely making yourselves available to us when we need answers to technical questions, information for our newsletters, or support for patients in need.
Thank you, Tim Rozelle, and the members of the Proton Therapy Law Coalition,
for helping to coordinate and unify proton therapy providers, patient advocates, and attorneys to fight health insurance denials of proton therapy.
Thank you, Ron Hendricks, for allowing us to reprint your helpful hints on estate planning.
Thank you, Bob Hawley, for your timely, careful, and professional reviews of our monthly newsletter.
Thank you, Ralph Ambrose and the LLUCC Web team, for making sure our website and other systems are running smoothly and for answering our many questions with careful thought and timeliness.
Thank you, Larry Becker, Kelsey Culler, and the rest of the LLUCC team, for the thorough and timely editorial reviews of our monthly newsletter.
Thank you, Janya Mekelburg, for supporting our daily activities in so many ways over the years and for your responsiveness when obstacles surfaced. We were very saddened that you left us this year, but thrilled that your move will bring you closer to family members.
Thank you, Rathyna Gomer, for taking over Janya’s role. We’re so excited to be working with you!
And finally, although he’s retired from LLUH and now pastoring a church in Los Alamitos, CA, we would be remiss if we didn’t extend a special thank you to Dr. J. Lynn Martell, who recognized the extraordinary potential of our group at the very beginning and offered encouragement and support in so many ways over the years. We wouldn’t be here today if it weren’t for Lynn and his support.
-----------------------
With the help of these people, we’re making a difference: Our members are well informed ambassadors for proton therapy; our group is responsible for introducing hundreds of men each year to proton therapy; and we have responded to assaults and misinformation on proton therapy as well as attempts by some insurers to stop reimbursing for proton treatment. Through our members, we have raised close to $14 million, most of which was directed to proton therapy research. We’re so proud of our group and thankful for our members and all who support our efforts.
We wish you all a very happy and healthy Thanksgiving.
Low PSAs to all,
Bob Marckini and Deb Hickey
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
NO MEDICAL ADVICE: Material appearing here represents opinions offered by non-medically-trained laypersons. Comments shown here should NEVER be interpreted as specific medical advice and must be used only as background information when consulting with a qualified medical professional.