Dear Members (a note from Deb Hickey):
The national holiday where we’re called to celebrate fatherhood and paternal bonds is less than a week away. New dads, experienced dads, granddads, dads-in-law, stepdads, like-a-dad big brothers, soccer coach dad figures, dad-like neighbors … there are probably hundreds of paternal types out there, and without a doubt, there are at least that many reasons to honor them on Father’s Day.
You can go to your local CVS or Walgreens, or visit a specialty gift shop, and buy a nice card to celebrate the father figure in your life. Or if you’re like my younger self, take a trip to Wal-mart or The Dollar Store and grab your pappy a glass dolphin paperweight or a plastic back scratcher. One year, I bought my dad a box of golf balls with Bea Arthur’s face on them … but that’s a story for another time.
FYI: Amazon can ship you a Batman Snuggie in four days. They also have toilet putting greens in stock. Did you know you can ship your male mentor a potato with your face on it? The online options are endless. Feel free to pass along these ideas to your kids.
But here’s the thing – I’ve come to a stage in my life where I don’t really like to spend money on stuff just because there’s an upcoming holiday and Target is having a sale. I’ve also realized there are two gifts that Dad would cherish so much more than another necktie, and they don’t cost a dime ─ my words and my time. As such, I’ll be stealing a few sentences from my opening newsletter memo from last year in which I wrote a heartfelt letter to my father, and I’ll be crashing my parents’ 55th anniversary dinner on Friday,
June 18.
Done and done.
So, here’s a short reiteration of last year’s letter. I don’t think I could have said it any better anyway …
Dear Dad,
When I was a child, the simple sound of the garage door opening as you came home from work gave me such comfort. I’ll forever hold dear the memory of your made-up bedtime stories; the lively way you used to play “The Entertainer” on the old organ with the dual keyboard; and riding around on your feet while you called out to no one, “Where’s Deb? Where could she be?”
Sweaty hugs. Those were the best. You’d come home from a jog wearing your gray track suit, soaked with perspiration. “I need a hug!” You’d shout joyfully as you looked around, eventually affixing your eyes on me. A chase pursued. I can’t remember what happened next, but I remember the exhilaration I felt as we ran around the house.
You chose blue Christmas lights every year. As an adult, when I see windows decorated with blue candles or blue fairy lights adorning a tree, I can almost smell the balsam fir and hear an Elvis record playing in the next room.
Boating. With you at the helm and Cuttyhunk in the distance, I remember thinking, life couldn’t possibly get any better.
What a life you’ve given me.
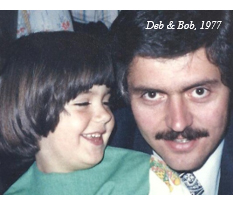 So, this Father’s Day I’d like to (again) publicly thank you for your boundless love and support, the safety and comfort I felt every day throughout my childhood, the brilliant and thoughtful guidance you rendered whenever I was in need, acting like a kid when I was a kid, being a friend when I needed a friend and a parent when I needed a parent, and all the memories in between. I’ll love you for eternity.
So, this Father’s Day I’d like to (again) publicly thank you for your boundless love and support, the safety and comfort I felt every day throughout my childhood, the brilliant and thoughtful guidance you rendered whenever I was in need, acting like a kid when I was a kid, being a friend when I needed a friend and a parent when I needed a parent, and all the memories in between. I’ll love you for eternity.
And while I’m at it, I’d also like to thank the late Dr. James Slater and the Loma Linda University Cancer Center for the gift of the past 21 healthful years (and counting) with my father. I certainly wouldn’t be working with him every day had he not come across proton therapy. What a blessing!
Father’s Day is June 20. Happy Father’s Day to the hundreds of dads and father figures in our group. May your special day be one of joy and love.
This issue of the BOB Tales newsletter is a record breaker at 34 pages. I apologize in advance. Or if you’re on the other side of the fence, you’re welcome – now you can sit in the bathroom for an extra half hour.
This month, we highlight several presentations from the recent 2021 National Association for Proton Therapy annual conference. This isn’t a complete recap of the event, but rather a recap of the topics we feel would be of most interest and value to our members. Also, had we summarized the entire conference, this month’s newsletter would be 115 pages. Though virtual for the second year in a row, this was the most comprehensive conference to date! We have some truly interesting and exciting things to share with you.
We received a surprisingly large member response following last month’s story on transperineal biopsy. Wait until you read about one member’s experience after he had gold fiducial (seeds) implanted through his rectum! We also followed up with Dr. Matthew Allaway, urologist and founder/president of Perineologic. He told us the important reasons he chose to invent the Transperineal PrecisionPoint™ (TP/PP) prostate biopsy technology and some of the challenges he’s faced in the process.
We’re excited about a U.S. FDA program that’s providing hope for some cancer patients who’ve exhausted their treatment options. Also, the COMPPARE trial comparing proton therapy to IMRT for prostate cancer has reached an impressive milestone and we share the latest updates on the study. We also report on a new genetic tool that’s able to predict a man’s lifetime risk of prostate cancer with only a blood or saliva sample. And there’s much more.
We hope you enjoy our June/July BOB Tales. As always, we welcome and encourage your feedback. Please send an email to [email protected].
Deb Hickey
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
In This Issue:
- New/Improved Biopsy Procedure Follow-up
- Hope for Cancer Patients Who’ve Exhausted Their Options
- Study Update: COMPPARE –Proton vs. Photon for Prostate Cancer
- Genetic Tool Predicts Age-specfic Risk for Developing Prostate Cancer
- Screenings and Lifestyle Changes Crucial to Longevity
- Colon Cancer Screening Age Lowered



New/Improved Biopsy Procedure Follow-up
Last month we wrote about serious infections resulting from today’s standard prostate biopsy procedure. The current procedure involves the passing of a needle through the rectum into the prostate in order to collect tissue samples to determine if cancer is present. Typically, an antibiotic is prescribed – commonly Ciprofloxacin (Cipro) – to prevent infection. Unfortunately for some, the antibiotic doesn’t prevent infection. The infection is caused when fecal matter from the rectum is unintentionally “injected” into the prostate. And when that infection is sepsis, the danger to the patient increases dramatically. Hospitalization is common, and death can occur.
This transrectal (TR) biopsy procedure is essentially the same technique used for the past 30 years; very little has changed. Yet, during the past 30 years, the use of antibiotics has been steadily rising, which has increased bacterial resistance, and has resulted in increased infection rates and sometimes death.
Surprisingly Large Member Response
The response from our members on this story has been overwhelming. Many told us of their personal experience with infection or about friends and acquaintances who have experienced serious infections. One of our members who had gold fiducial (seeds) implanted through his rectum told us he became very sick, was hospitalized and placed on intravenous antibiotic treatment followed by two more weeks of antibiotics to deal with his severe sepsis infection – all before beginning his proton therapy.
Another member wrote to us about some of the dangers associated with Cipro and other fluoroquinolone antibiotics. While not common, potentially serious side effects from fluoroquinolones can include increased risk for aortic aneurysm, hypertension, high blood pressure and certain genetic conditions. Other patients have been issued warnings that include decreases in blood sugar levels as well as certain mental health side effects and the (low) risk of retinal detachment. More information on these issues can be found here and here, articles/studies provided by the member who called these issues to our attention.
Follow-up with Dr. Allaway
We wrote last month about our interview with, Dr. Matthew Allaway, a urologist, founder/president of Perineologic and the inventor of a new prostate biopsy technology called Transperineal PrecisionPoint™ (TP/PP), which has significantly changed the prostate diagnostic landscape and has virtually eliminated the probability of sepsis infection.
We spoke with Dr. Allaway again this month just after he returned from traveling to several states training urologists in the TP/PP technique. During our conversation he told us he made the decision eight years ago that he’d never again biopsy a patient through the rectal wall. “The following day,” he said, “I modified a prior method I used to treat prostate cancer in order to biopsy the prostate. I call this ‘The free-hand TP biopsy’ that I published in 2014.” He further told us, “I made this decision because I was deeply concerned about the risks of TR (transrectal) biopsy and the gross limitations in detecting all relevant cancers. I never intended to develop a device or company and travel around the word training urologists. My only goal at the time was to do a better job.”
Dr. Allaway was also motivated by the inability of today’s TR biopsy to access the entire prostate. “I witnessed a slow death of a patient and friend from prostate cancer. He was under-graded as having low-risk disease because the cancer was located in the anterior of prostate and I was unable to sample this region using the TR approach.” This was prior to today’s advanced MRI imaging.
Slow in the U.S. – ‘TRexit’ in the UK – Rapid Acceptance in Norway and Australia
There are still challenges in gaining acceptance of this newer, safer biopsy technique in the U.S., especially from insurance companies, Allaway said. Yet in other countries the path has been much smoother. “In the UK, they started the ‘TREXIT’ movement – transrectal exit.” “In Norway,” he told us, “the TR biopsy has been condemned. And in Australia, they just cut reimbursement for the TR biopsy and some commercial carriers will not pay for a TR biopsy.”
There are peer reviewed manuscripts on the TP/PP approach and the level of evidence showing its superiority is mounting. “But this is not enough,” said Dr. Allaway. “The only way we will move the needle is patient advocacy groups like the Brotherhood of the Balloon. This is surprisingly a much more powerful way to change the way we biopsy men. I wonder if you realize the impact that your work has on the medical community. Men and the families that love them depend on the honest and educational content of your newsletter.”
After drafting this article, Bob was contacted by the wife of a dear friend living in Philadelphia. His friend is in his early 80s; has rapidly rising PSA, and also a very serious comorbidity. A prostate infection in his case could be deadly. With help from Dr. Allaway, Bob learned that both U. Penn and Jefferson Hospital in Philadelphia are qualified to administer the TP/PP prostate biopsy technique. Bob directed his friend to a TP/PP trained physician for his biopsy.
As we mentioned last month, transperineal biopsies have been done in the past, but they are not commonly done because the procedure required general anesthesia, involved multiple punctures of the perineum, and took an excessive amount of time. The new TP/PP technique can be done with local anesthesia in about the same amount of time as as the current TR approach; it involves only two punctures, and antibiotics aren’t needed.
We will continue to follow developments in this important story and will report them in future BOB Tales.
Hope for Cancer Patients Who’ve Exhausted Their Options
Sadly, for many cancer patients, standard treatment options don’t always work. Their doctors often direct them to clinical trials hoping for a cure, or to systemic treatments (ADT, chemotherapy, etc.) in hopes of slowing the progression of disease and delaying
the inevitable.
But for patients who’ve exhausted their treatment options and for whom clinical trials aren’t available, there may be some hope. The U.S. Food and Drug Administration’s Expanded Access (EA) program, sometimes called “compassionate use,” and the 2018 Federal Right to Try program are helping patients gain access to unapproved drugs outside of clinical trials when no comparable alternative therapy options are available.
A recent survey of community oncologists-hematologists in the U.S. evaluated the effectiveness of the two programs. Eighty-nine percent of the physicians who used the EA program reported success in obtaining the investigational drug for their patients and 73 percent were successful in accessing investigational drugs for their patients using the Right to Try pathway.
Study Update: COMPPARE – Proton vs. Photon for Prostate Cancer
 COMPPARE stands for “A Prospective COMparative Study of Outcomes with Proton and Photon RAdiation in PRostate CancEr.” The COMPPARE trial will compare the quality of life, side effects, and cure rates for prostate cancer patients treated with proton therapy or photon therapy (IMRT).
COMPPARE stands for “A Prospective COMparative Study of Outcomes with Proton and Photon RAdiation in PRostate CancEr.” The COMPPARE trial will compare the quality of life, side effects, and cure rates for prostate cancer patients treated with proton therapy or photon therapy (IMRT).
Remind me – why is this study so important?
This study is exciting. It’s the first of it’s kind – a multi-institutional, national trial that will directly compare the potential benefits and harms (cure rates and side effects) of protons versus photons (conventional radiation) in treating men with prostate cancer. It will emphasize patient-centered outcomes and will help future patients make informed treatment decisions. And, as you know, many health insurers refuse to cover proton therapy for prostate cancer due to its higher upfront cost and unanswered questions about its effectiveness compared to photon therapy. The COMPPARE study should answer the question, once and for all, as to whether or not there are discernible differences between proton therapy and IMRT in treating prostate cancer. Results of the study could resolve disagreements that are restricting patients’ access to proton therapy, particularly with regard to private medical insurers’ coverage and reimbursement policies.
Who’s running the show?
The study is being led by Nancy Mendenhall, MD, Professor, Dept. of Radiation Oncology and Medical Director, University of Florida Health Proton Therapy Institute. The COMPPARE Consortium comprises a diverse group of clinicians, researchers, patients, and other stakeholders, all committed to directly comparing the potential benefits and harms of proton versus photon therapy. There are 55 principal investigators, co-investigators, and researchers representing more than 40 medical institutions and healthcare providers. There are more than 20 patient and caregiver stakeholders including Deb Hickey, a patient stakeholder. There are eight on the executive board, including Bob Marckini. The minority engagement group, consisting of 14 advocates, supports the study by educating and recruiting participants in local communities. The Advanced Technology Consortium, led by three representatives from the Washington University School of Medicine in St. Louis, provides an informatics infrastructure and quality assurance process to support the submission, review, and anlaysis of volumetric imaging and treatment planning data for the study. And finally, the team backbone consists of several UFHPTI staff members who run the day-to-day administration, communications, project management, financial management, and clinical coordination.
How big is the study?
The COMPPARE trial will follow 3,000 prostate cancer patients across the U.S. who will be treated with either protons (1,500) or IMRT (1,500).
Who’s eligible?
In general, to be eligible for the COMPPARE study you must be a man diagnosed with non-metastatic prostate cancer; a candidate for radiation therapy; and between the ages of 30-85 with a life expectancy more than eight years. If you’re interested in participating, your doctor can explain the study’s eligibility criteria in more detail. Or, send an email to [email protected].
Wait – there’s more!
COMPPARE participants in the proton arm can also choose to be included in a randomized trial that will evaluate whether quality of life, side effects, and prostate cancer cure rates differ between patients receiving the standard treatment protocol (44 treatments) versus a shorter protocol (20-24 treatments).
As a participant, will my treatment change?
There is no impact on the treatment protocol. All COMPPARE trial participants receive the standard-of-care for whichever treatment they choose – proton therapy (standard or shortened treatment protocol) or IMRT. Participants are asked to answer brief surveys regarding treatment choice, quality of life, and side effects for about three years.
How far along is the study?
As of last month, 50 percent (n=1500) of the project accrual goal has been completed! We’ve also reached another milestone – all partner sites are active, having enrolled at least one patient. The goal is to be finished with accrual by the end of September 2022.
What have been the biggest hurdles?
Researchers from the University of Massachusetts Medical School reported sobering news regarding the impact of COVID-19 on prostate cancer screenings: PSA testing to screen for or diagnose prostate cancer fell from 34.4 men per 1,000 tested per month in 2019 to 17.6 tests in March 2020, 6.1 in April and 11.3 in May. Prostate biopsies were performed at a similar rate over the first five months of 2019 and 2020.
Consistent with a decrease and delay in screening and thus diagnosis of prostate cancer, by October 2020, most COMPPARE partner sites had experienced decreases in referrals and delays in beginning radiation treatment. Many sites had to stop research efforts entirely.
In the Spring 2021 issue of the COMPPARE Connection newsletter, Dr. Mendenhall wrote in her opening memo, “Through our engagement efforts, we continue to remind everyone that men between the ages of 55 and 69 – especially African-American men or those with a strong family history of prostate cancer – should consider scheduling a prostate screening that includes both a PSA blood test and prostate examination. It is imperative that you have these discussions with your brothers, fathers, sons, and friends.”
What do we expect in the coming months?
We hope and expect that as COVID vaccines are rolled out across the country and patients get back to annual prostate screenings, the COMPPARE accrual rate will ramp back up. “I am so appreciative of the dedication displayed by the COMPPARE Administration Team, the research teams at all 51 participating sites, our Patient Stakeholder and Minorit
Engagement Groups, and most of all our COMPPARE enrollees, all working hard to conduct research that will improve the ability of future patients to make informed decisions based on knowledge of the comparative outcomes of conventional radiation and proton therapy in prostate cancer,” wrote Dr. Mendenall in closing.
When will the results be in?
Although we may have an interim analysis around the two-year mark, final data will be reported in 2026.
Genetic Tool Predicts Age-specfic Risk for Developing Prostate Cancer
Researchers at the University of California San Diego School of Medicine have validated a more comprehensive genetic tool for predicting age of onset of aggressive prostate cancer.
“Genetic tools to predict a man’s lifetime risk of prostate cancer might allow us to target cancer screening efforts to the men who are most likely to need it. We are addressing a major public health problem and simultaneously addressing a concern that genomics and genetic tests may exacerbate health disparities because people of non-European ancestry are severely under-represented in most studies,” said principal investigator Tyler Seibert, MD, PhD, assistant professor at UC San Diego School of Medicine and radiation oncologist at Moores Cancer Center at UC San Diego Health.
The genetic score was tested in a multi-ethnic dataset of 80,491 men and was shown to be associated with age of onset of prostate cancer, as well as with age at death from prostate cancer.
With only a blood or saliva sample, a man’s genetic risk of prostate cancer can be estimated,” said Minh-Phuong Huynh-Le, MD, who is first author of the paper and was a resident physician at UC San Diego Health during the study. “Prostate cancer screening may reduce morbidity and mortality, but it should be targeted and personalized. Those at higher genetic risk might benefit from earlier and/or more frequent prostate cancer screening, and this genetic tool could identify those individuals.”
According to Dr. Seibert, however, more research still needs to be done as much of the data used for research continues to lack diverse representation. In fact, even the data for this study were missing clinical diagnosis information in men of African genetic ancestry.

We’ve been producing BOB Tales newsletters monthly for more than 20 years. During this time there have been articles that many new members haven’t seen, and some older members may have forgotten. So, we periodically re-run articles from past newsletters. The following is from August 2008.
Screenings and Lifestyle Changes Crucial to Longevity
We know that nearly half of all cancer deaths are preventable. More than that, the key to success doesn’t rest with some undiscovered therapies or treatments. Much of cancer’s toll can be reduced with simple precautions, such as lifestyle changes and routine screenings. But somehow that message isn’t getting through to enough people according to Carolyn “Bo” Aldige, president of the Cancer Research and Prevention Foundation, in Alexandria, VA.
The biggest threat, of course, is smoking. “You’d have to live on another planet not to know smoking causes cancer,” Aldige said. Smoking is the single-most preventable cause of death in U.S. society. Tobacco causes nearly one in five deaths in the United States, killing about 438,000 Americans each year, according to the American Cancer Society. Yet, about 45 million adults still smoke ─ about 23 percent of men and 19 percent of women.
Update 2020-2021: Cigarette smoking remains the leading cause of preventable disease, disability, and death in the U.S., accounting for more than 480,000 deaths every year, or about 1 in 5 deaths.
Okay, so you don’t smoke – great, but how is your diet? Experts estimate that about one in three of the 564,830 deaths from all forms of cancer this year (2008) will be related to poor nutrition, inactivity, weight, and obesity. Research has shown that excess calories cause mutations that start genes going down pathways that cause cells to divide out of control, and that’s when you have a cancer. “If everybody magically had the appropriate body mass index, we’d start seeing a lot less colorectal, breast, and prostate cancer,” Aldige said.
Then there’s melanoma, the deadly skin cancer that’s on the rise. An estimated 62,190 new cases of the disease will be diagnosed in the U.S. this year (2008), and 7,910 people will die of it, according to the American Cancer Society. But melanoma is highly curable if it’s caught in its early stages. The best way to do that: Check your own skin about once a month and become familiar with the pattern of moles, freckles, and other marks so you’ll spot any changes. And a skin exam should be part of a routine cancer checkup by a doctor or qualified health professional. While too much sun causes skin cancer, we need some sun every day ─ about 15 to 20 minutes worth, for vitamin D. The trick is to go out before 10 a.m. and after 4 p.m. during warm weather months. We may not be able to completely prevent all cancers, but we can substantially decrease our risk by doing the right things.
Finally, there’s a highly effective second line of defense against each of these cancers and many others ─ screenings. Doctors can test for these cancers, as well as testicular, cervical, and other kinds of malignancies, and often catch them before they’ve gone too far. And having the tests usually requires little time and causes only minimal discomfort.
Update 2020-2021: The American Cancer Society states that this year 106,110 melanomas will be diagnosed and 7,180 people are expected to die of melanoma, roughly twice as many men as women.

Don’t Just Stand There
In an effort to boost funding for basic and clinical proton therapy research on prostate cancer, pancreatic cancer, liver cancer, breast cancer, and more, we asked our members to donate $100 (or more) to Loma Linda University Cancer Center. In return, they’d receive an advance copy of Dr. William Preston’s book, Don’t Just Stand There – Realizing a Vision for Proton Therapy: Conversations with James M. Slater, MD, FACR. The response so far has been phenomenal. Thank you to all who’ve requested a copy.
 There are still books left! So, if you’d like a pre-published copy of this awesome book that likely won’t be available to the public until next year, please send a check for $100 or more, payable to “Loma Linda University Proton Cancer Research” and mail it to:
There are still books left! So, if you’d like a pre-published copy of this awesome book that likely won’t be available to the public until next year, please send a check for $100 or more, payable to “Loma Linda University Proton Cancer Research” and mail it to:
Loma Linda University Health ● Office of Philanthropy ● PO Box 2000 ● Loma Linda, CA 92354
Please notify Deb Hickey at [email protected] that you’ve sent in your check and your book will be mailed immediately.
This book, which contains high-quality color images and illustrations, is not only about Dr. Slater’s quest to create the world’s first hospital-based proton treatment center, it’s also a teaching guide. As the Proton Treatment & Research Center at Loma Linda was such an immense endeavor, Dr. Slater wondered if the aspects of conceiving, planning, and orchestrating such a project, among others he undertook, might be instructive to others. Over the years, he’d also met people in all walks of life, many of whom had dealt with large and complex problems. He was struck by some of the stories they told about their work. And although the fields or disciplines usually had nothing to do with medicine, many experiences were similar. And so, he kept this in mind while he worked on the book with Dr. Preston.
We’re sure you’ll thoroughly enjoy the book and we know it will occupy a place of honor in your home. And, you’ll be helping to fund basic and clinical proton research on prostate cancer, pancreatic cancer, liver cancer, breast cancer, and much more with your tax-deductible gift. Thank you!
What’s an Endowed Chair?
Chair is the term used to describe an endowment that provides a steady stream of income to fund the work of research scientists. LLUCC does not receive sufficient revenue from patient care to fund research. Life-saving research is dependent upon the generosity of individuals. With funded chairs, the organization is able to attract and retain some of the best researchers. In addition, scientists are able to dedicate all of their time to research. Without endowment earnings, they could spend a third of their time trying to raise money through grants. A minimum of $2.5 million is needed to fund a chair to support one researcher.
 Other Ways to Give
Other Ways to Give
- Donate to proton research online.
- Write a check to LLUCC Proton (Put “Marckini Chair” on the memo line) and mail to LLUH, Office of Philanthropy P.O. Box 2000, Loma Linda, CA 92354.
- Make an unrestricted gift (put “unrestricted” on memo line) so LLUH can use it where it’s needed most.
- Call Regina Joseph at 909-558-5010 to donate over the phone and/or to inquire about naming opportunities.


Colon Cancer Screening Age Lowered
 We have lots of colon cancer in our family: Bob’s grandparents (both), parents (both) and a sibling. So, we pay close attention to colon cancer screening.
We have lots of colon cancer in our family: Bob’s grandparents (both), parents (both) and a sibling. So, we pay close attention to colon cancer screening.
Until recently, the U.S. Preventive Service Task Force recommended that people at average risk for colon cancer begin screening (colonoscopy) at age 50. In May, the USPSTF lowered the screening age to 45, finalizing draft guidelines issued in October 2020 that will mandate insurance coverage at that age, according to USA Today May 19, 2021.
These new guidelines follow The American Cancer Society guidelines from 2016 recommending that the screening age be lowered to 45.
Since the mid-1990s, there has been a concerning increase in colorectal cancer among people under 50 years old, according to Dr. Kimmie Ng, director of the Young-Onset colorectal Cancer Center at Dana-Farber Cancer Institute. In 2020, for example, 11 percent of colon cancer and 15 percent of rectal cancers occurred in patients under 50 years of age. This is roughly double the numbers from just 10 years prior.
Dr. Douglas Rex, president-elect of the American Society for Gastrointestinal Endoscopy, reports that in the 45 to 50 age group, there are about 7,000 new colorectal cancer cases per year and about 1,800 deaths, accounting for about 50 percent of colorectal cancer diagnoses in the under-50 age group.
Lowering the recommended screening age will make colorectal cancer screening accessible and affordable to millions more Americans according to Dr. Ng, since U.S. health insurers are required to cover, at no charge to the patient, any service the USPSTF recommends with sufficient evidence, regardless of the cost.
Three Healthy Moves
A Parade Magazine series called “Live Smart” had three suggestions for improving your health.
Walk: Shoot for 30 minutes a day, but if that’s too much, start with 10-minute strolls says Cleveland Clinic exercise physiologist Christopher Travers, M.S. Walking helps manage your blood sugar, fight arthritis pain and helps keep your brain sharp.
Fight inflammation with food. Inflammation can clog your arteries, increase pain and fog your brain. Cleveland Clinic’s William Welches, D.O., Ph.D., says that inflammation comes from a biochemical reaction initiated by your immune system. Certain “bad carb” foods, such as white foods and sugar, can promote inflammation, while healthful foods, like veggies – especially cruciferous veggies – and fruit help to reduce inflammation. Andrea Dunn, Cleveland Clinic registered dietitian, suggests eating salsa. “It’s a great replacement for high-calorie dressings or dips, and helps increase your intake of vitamin C, fiber and inflammation-fighting antioxidants.”
Sleep smart. Psychologist, Michelle Drerup, director of behavioral sleep medicine at Cleveland Clinic says that “Sleep has a significant impact on our immune functioning.” Sleep deprivation also can result in heightened susceptibility to viruses of all types, including the common cold. Most adults require seven to nine hours sleep a night, she says. If you don’t feel refreshed when you wake up, you’re not getting enough sleep.

 You Can Beat Prostate Cancer: And You Don’t Need Surgery to Do It – Second Edition
You Can Beat Prostate Cancer: And You Don’t Need Surgery to Do It – Second Edition
Bob’s new book still sits in one of the top two positions on an Amazon “prostate cancer” search, and it continues to change lives. We regularly hear from recently diagnosed men or members of their families who tell us how much they learned from the book and how it’s changed their thinking.
A retired endodontist posted a review on Amazon stating, “Bob’s book, based on his years of research, afforded me the ability to ask the right questions of my urologist. With this book I feel I have the information that allows me to be the best advocate for my own health. Thank you, Bob, for being a true pioneer.”
Second Opinion ─ Treatment Canceled
One of the key points Bob makes in the latest edition of his book is that the interpretation
of biopsy slides is quite subjective, and it’s important to get a second opinion from a highly skilled and experienced pathologist. There are numerous documented cases of the initial reading being incorrect and the prescribed treatment (surgery or radiation) being unnecessary. Last month we heard from a gentleman who was diagnosed with Gleason 7 prostate cancer and was scheduled for surgery. After reading Bob’s book, he requested a second opinion on his biopsy slides from Dr. Jonathan Epstein’s lab at Johns Hopkins. He learned his Gleason score was, in fact, 3+3=6. Greatly relieved, he canceled his surgery and is doing active surveillance
Centers Sending Books to Prospective Patients
Many proton centers send Bob’s book to patients who make inquiries about proton therapy for prostate cancer. We’ve heard from several who tell us that Bob’s book has made a noticeable difference in patients’ decisions to choose proton therapy. The director of marketing for one proton center, which just purchased Bob’s new book, sent Bob the following message:
We love your new book. I haven’t seen our intake manager so excited in all the time we’ve worked together. We have always had a tremendous response from patients who received your previous book. It was hard to imagine it could be improved, but you’ve done it with the new edition! Thank you for continuing your mission to reach men facing prostate cancer. You are an inspiration and are greatly appreciated!
Did you find Bob’s new book helpful?
Please write a review on Amazon.
We’re happy to discount books in quantity (minimum 20) to anyone interested in spreading the word on proton therapy. Just send an email to Deb Hickey. Proceeds from book sales are used to help fund our efforts and to support proton therapy research.
The Kindle version is free to Kindle Unlimited members or can be purchased for $9.99 for non-members. The paperback price is $22.45. Buy You Can Beat Prostate Cancer second edition on Amazon or Lulu Press.
Recap: 2021 Virtual Proton Conference: Advancing the Future of Proton Therapy
The ninth annual National Association for Proton Therapy Conference – the second virtual event, due to the coronavirus pandemic – was held on April 14-16, 2021. Industry leaders and proton therapy experts from across the globe delivered comprehensive presentations on the latest research supporting the benefits of proton beam therapy. Keynote speakers, Ron Rivera, Washington Football Coach, and Grace Eline, pediatric cancer survivor and advocate, spoke about their experiences as proton therapy patients. Other discussion topics included flash therapy and other exciting advancements in proton therapy delivery; hot clinical topics in proton therapy, innovative solutions to advance the proton therapy insurance appeals process; an update on the Medicare Radiation Oncology Alternative Payment Model; and improving patient access to proton therapy through value-based initiatives. The robust agenda and interactive capability made the conference a valuable opportunity to access the latest information and resources in the proton world. Deb Hickey attended from her home in Medfield, MA. Her recap follows.

NAPT Executive Director, Jennifer Maggiore, and her team did another superb job pulling a comprehensive conference together. Although this is the second year they’ve had to conduct the event online and Deb again missed the personal interaction with her friends in the proton community, the outcome was impressive.
There were nearly 400 attendees at the live event, representing 240 organizations from 15 countries. The virtual space allowed the opportunity for attendees across the globe to engage with the proton therapy community in a truly unique way.
The following isn’t intended to be a comprehensive review of every presentation – instead, it includes highlights from the conference that we think would be of interest and value to our members
FLASH Therapy
There was a lot of talk about FLASH therapy and several presentations on the topic! Thursday morning, representatives from medical technology company IBA introduced the new therapeutic technique involving radiation treatment of tumors at ultra-high dose-rates, which reduces normal tissue toxicity while maintaining the effectiveness of conventional radiotherapy. They explained that while most studies to date have been performed using electron beams, FLASH radiation can also be delivered using protons and photons. Carbon delivery is also being studied.
Studies on the Effects of FLASH Therapy on Mice
Mass General Hospital and PENN Medicine researchers recently studied the effects of FLASH therapy in comparison to conventional radiation treatment on mice. Results showed a tremendous healthy tissue-sparing effect and a major difference in survival among the animals. In the MGH study specifically, none of the mice that received FLASH therapy died, while 60 percent of the mice that were treated with conventional therapy died.
Delivering Radiation in Less than a Second
In a subsequent presentation, Dr. James Metz, MD, Chairman of Radiation Oncology at the University of Pennsylvania, gave his take on FLASH therapy, letting attendees know he’s excited about the technology, but explained why treatment centers can’t move too fast.
 Dr. Metz described FLASH therapy as delivering ionizing radiation, whether it’s photons, electrons, or protons at doses faster than 40 Gy in less than a second, what he described as “remarkably high doses” in which you can give “potentially the entire course of radiation in less than a second.” He commented on several studies that found FLASH to be less toxic to normal tissues, while it’s just as effective on tumor control as conventional radiation .
Dr. Metz described FLASH therapy as delivering ionizing radiation, whether it’s photons, electrons, or protons at doses faster than 40 Gy in less than a second, what he described as “remarkably high doses” in which you can give “potentially the entire course of radiation in less than a second.” He commented on several studies that found FLASH to be less toxic to normal tissues, while it’s just as effective on tumor control as conventional radiation .
So, why is this important? According to Dr. Metz, FLASH therapy could completely revolutionize radiation if it can be broadly validated. Higher doses could potentially be delivered safely to tumors or established treatment could be given with reduced toxicity to critical organs. We could also deal with some of the challenges we have, such as organ motion.
Key Learnings Thus Far
According to Dr. Metz, key learnings for FLASH radiation thus far include:
- FLASH effect is real and has been demonstrated in electrons, photons, and protons
- FLASH shows normal tissue protection in a variety of areas
- FLASH shows at least similar tumor control to conventional radiation
- Stem cells appear to be spared more with FLASH radiation than conventional dose rate radiation
- Dosimetry and control of the beam are critical to see the FLASH effect – small perturbations in the beam can negate the effect
- FLASH effect is lost with reducing dose rate below 40 Gy/sec
- There is a window of impact with FLASH
- FLASH proton radiation has the potential to be a major disruptor in oncology because:
- It could significantly compress radiation treatments and radiation could become more like a surgical procedure;
- It could improve the quality of life of patients with reduced toxicity and time commitment;
- It could bring together biology and technology in new ways;
- It can cause different immune pathways to be activated and different gene expression, which means new opportunities for drug/radiation combinations;
- It opens the possibility of expanding to benign diseases in new ways;
- It has the potential to significantly reduce the cost of radiation and at the same time financially work well with Alternative Payment Models.
Not So Fast
Dr. Metz reiterated that although there’s a lot of excitement around FLASH and “we’re sure there will be a lot more on FLASH at future NAPT conferences, we’re only at the beginning of this technology.” Using FLASH therapy is not as simple as flipping a switch; in fact, there will be numerous technical adjustments that will need to be made; using FLASH therapy will require significant investments in existing facilities; there are likely numerous hidden costs; treatment centers will have to ensure proper safety systems as there could be devastating impacts if there are mistakes with FLASH delivery; and finally, the FDA will require clinical trials of FLASH.
We’re excited to see the evolution of this exciting technology!
Proton ARC Therapy
According to representatives from IBA, the next evolution in proton delivery is proton arc therapy (PAT). Arc therapy is treatment with the radiation continuously on as the gantry rotates around the patient. It’s different from traditional proton therapy where the beam is switched off between gantry movements. Preliminary results demonstrate potential clinical benefits including faster and simpler treatment delivery for prostate, head and neck, lung, and brain cancers.
Proton Reirradiation
In a panel titled “Hot Clinical Topics in Proton Therapy,” John Plastaras, MD, PhD, an associate professor in the department of radiation oncology at Penn Medicine, talked about reirradiation with proton therapy. He explained that the rationale for reirradiation has evolved with the advancement of improved therapies and diagnostic techniques in cancer. The benefits of reirradiation include control over symptoms, progression-free survival, and in some cases, a cure. He mentioned the risk of toxicity and secondary cancers with high cumulative radiation doses and the fact that many patients are fearful to reradiate, but said the treatment is becoming increasingly common. There are tools that allow reirradiation to be done more successfully such as improvements in the use of advanced imaging, as well as biomarkers such as circulating DNA and tumor cells, which allow physicians to pick up recurrences sooner and perform safer treatments.
Increasing Diversity, Equity, and Inclusion in Proton Therapy and Clinical Trials
Curtiland Deville, MD, associate professor of radiation oncology at Johns Hopkins University School of Medicine, spoke about health disparities and inequities in the use of proton therapy in the U.S. He specifically discussed clinical trial enrollment trends and barriers to minority clinical trial enrollment. If you recall, in a recent BOB Tales newsletter, we mentioned the COMPPARE clinical trial team was having difficulty increasing minority enrollment, so Deb was particularly interested in what Dr. Deville had to say.
A recent study of more than 1,000 cancer therapeutic trials found that patients who were Black or Hispanic were reportedly less likely to enroll in trials than patients who were white. Dr. Deville discussed the detriment this can have for underserved and disadvantaged groups. For example, there was limited data for African Americans in major prospective randomized trials that helped set the recommendation by the U.S. Preventive Service Task Force (USPSTF) in 2011 to stop PSA testing.
Barriers to participation for these groups include lack of awareness or understanding about trials and the potential benefits of being included; potential provider bias in terms of who’s offering the trials; access to care, insurance coverage and cost of care; linguistic, cultural or literacy-related issues, and lack of trust in the healthcare system and/or clinical research.
Dr. Deville introduced some recruitment and retention strategies for minority research participants such as inclusive study design and broadened study criteria, community outreach and engagement, cultural adaptations of study and marketing materials, workforce diversity, and accountability in health equity metrics.
The FDA also recently issued a statement on how to enhance diversity in clinical trials. They suggested broadening eligibility criteria, using inclusive trial design and methodological approaches, and improving study design by making trial participation less burdensome, adopting enrollment and retention practices that enhance inclusivness, and expanding access to clinical trials in general. Specifically, some of their recommendations included alternative follow-up, real-time monitoring strategies, and providing adequate incentives.
At the end of his presentation, Dr. Deville mentioned the COMPPARE trial as a great example of a study – the largest of its kind – that’s focused on minority inclusion. The COMPPARE team includes a minority engagement group to specifically include community members and patient advocates. In his NAPT presentation, COMPPARE engagement materials were also highlighted as adequately reflecting diversity. We were proud to hear this!
Medicare Radiation Oncology Bundled Payment Model
We’ve written about Medicare’s new payment model for radiation oncology services and its impact on proton therapy several times in our newsletters. We weren’t surprised that it was a big topic of discussion at the conference.
A Recap
In September 2019, the Center for Medicare and Medicaid Innovation (CMMI) proposed a new payment model for radiation oncology services. If approved, the mandatory model for those on Medicare would result in beneficiaries receiving reimbursement for proton therapy at the same national base rate as all other radiation modalities (including IMRT and brachytherapy). To be clear, Medicare would no longer cover proton therapy as it had in the past. Rather, it would cover the same amount for proton as it does for any other radiation treatment, reducing coverage levels significantly.
In November 2020, the Radiation Oncology Alternative Payment Model (RO APM) was released, and unfortunately, it wasn’t what we expected or wanted. The new rule shifts payment for radiation oncology reimbursement from a fee-for-service model (the most traditional healthcare payment model where providers are paid for each service) to a value-based bundled payment (covers all the care a patient receives during treatment for a specific illness, condition or medical event).
Particpation is mandatory for 30 percent (12) of proton centers selected randomly by zip code. This means, proton therapy at these facilities will be paid by Medicare at the same rate as other radiation treatment modalities, most of which are much less expensive.
The rule will be tested for five years and then reassessed.
CMS’ Reasoning
According to the Centers for Medicare & Medicaid Services (CMS), the RO APM Model was created to “promote quality and financial accountability” for providers and suppliers of radiotherapy services.
With the final model design, CMS is seeking to test whether making prospective episode payments to hospital outpatient departments, freestanding radiation therapy centers, and physician group practices for radiation therapy episodes of care preserves or enhances the quality of care furnished to Medicare beneficiaries while reducing Medicare program spending through enhanced financial accountability for RO APM Model participants.
We’ve noted several times that we’re not sure how this model creates quality. Rather, it seems it’s a way for Medicare to save money. In fact, CMS estimates the expected savings are $230 million.
Timing
The new model is set to go into effect after January 2022. This means the new model can’t be implemented before 2022; it doesn’t necessarily mean it will be carried out in January. In fact, implementation could be delayed further.
An Update from the NAPT 2021 Conference
Speaker Scott Stuecher of Veralon, a healthcare consulting company, presented a map
of the U.S. that showed the 9,000 participating zip codes. Of the 37 proton centers in operation at the time of this writing, 14 are located in these zip codes including Houston, Philadelphia, New York, and Southeast Florida.
Mitigation Strategies for Proton Centers
Speaker Kurt Morath, VP of operations at Proton Therapy Partners, offered mitigation strategies to participating centers, especially the importance of leveraging technology. He suggested increasing patient throughput and decreasing operational costs by working on technological advancements. He recommended reducing treatment planning time; improving treatment delivery; and using automation to spend less time on repetitive and manual tasks.
Hypofractionation and SBRT
Mr. Morath focused on the utilization of hypofractionation and SBRT (stereotactic body radiotherapy) and the benefits of transitioning to shorter treatment protocols. Not only do these methods provide cost-saving opportunities, patients are more satisfied; decreased fractions allow for an increase in a center’s capacity; and there would be a higher reimbursement per treatment course under the new rule.
Flash Therapy
Flash proton therapy was also highlighted. Though it’s an experimental treatment modality at this time, it could be one of the most significant advancements in cancer treatment in decades and offer a much lower-cost proton therapy option down the road.
Improving Patient Access to Proton Therapy
A three-oncologist radiation panel discussed improving patient access to proton therapy through value-based initiatives.
What is ‘value proposition?’
The concept of “value proposition” was first defined in 1988 as “a clear, simple statement of the benefits, both tangible and intangible, that the company will provide, along with the approximate price it will charge each customer segment for those benefits.”
So how is value proposition defined in regard to proton therapy? According to Deputy Director and Chief of Radiation Oncology at the Miami Cancer Institute Minesh Mehta, it’s “simply a statement of value to be delivered.” Dr. Mehta stated this must include an analysis of the deliverable benefits and costs to the customer (including insurers, society, and individuals). He defined value as “benefits minus cost,” and the cost includes not just economic and other risks, such as toxicities and the cost of managing toxicities, but also intangible benefits that we “often don’t talk about.”
A Sample Proton Value Proposition/‘Peace of Mind’
Dr. Mehta explained that proton therapy will either enhance or equal the tumor control probability achievable by other treatment options. And, it will do so with a reduction in the incidence, and/or risk of acute and/or long-term radiation-induced side effects. This may be achieved with a potential cost reduction, but it’s not necesssarily an ingredient of the value proposition that’s an absolute requirement. “But it could, in fact, lower cost if we could do safer hypofractionation and reduce the overall cost of managing radiation-induced side effects,” Dr. Mehta said. “The intangible component of this is the ‘peace of mind’ benefit.” Dr. Mehta said many patients who are “shopping around” for treatment are considering proton therapy for peace of mind. They’ve done their homework and they understand the advantages of proton therapy – most important, the sparing of healthy surrounding tissues.
A Systematic Review of the Cost and Cost-Effectiveness Studies of Proton Radiotherapy
Dr. Mehta referenced a 2016 article he and two other physicans published titled, A Systemic Review of the Cost and Cost-Effectiveness Studies of Proton Radiotherapy. Though the paper is dated, the key component is the understanding of the cost-effectiveness plan. Simply put, the ideal treatment plan is more effective with a lower cost versus a less effective plan with a higher cost. In the published paper, the authors reviewed 30 articles and extracted evidence to prove the cost effectiveness of proton therapy versus other treatment modalities.
Head and Neck Cancers
There was strong evidence in support of proton therapy for head and neck cancers by halving side effects and reducing costs. Since the paper was published, there have been several studies backing this up.
Pediatric Medulloblastoma
Data suggested that the lifetime (including morbidity management) cost for IMRT for treating children with medulloblastoma was more than $100k while the proton therapy cost was less – about $80k. As a result, the quality-associated life years gained in favor of proton therapy was significantly higher at 17.4 compared to 13.9 for photon therapy.
Esophageal Cancer
Cancer of the esophagus represents another treatment site where proton therapy could have a positive value proposition. This is primarily because tri-modality therapy – a combination of chemotherapy, radiation, and surgery – is accompanied by signficant toxicity risks. This can be measured using a mean total toxicity burden, which is much higher for IMRT than with proton therapy. This includes post-operative length of stay, which is much shorter after proton treatment; fewer cardiopulmonary and wound toxicities with proton therapy; and a reduction in 90-day mortality rates with proton therapy. These results suggest that when treatment is excessively toxic, the value of proton therapy shines simply by reducing morbidity, mortality, and cost.
Exploiting Hypofractionation
Dr. Mehta explained that hypofractionation represents an “important frontier to demonstrate the value proposition of proton therapy.” For example, the five-fraction protocol (SBRT) for intermediate-risk prostate cancer has been taking off. And according to Dr. Mehta, the five-fraction protocol – and even shorter protocols – for accelerated partial breast irradiation are “all the rage.” He referenced a paper in the International Journal of Radiation Oncology stating this may also be highly cost effective. Therefore, hypofractionation could build an even larger value-based case for proton therapy.
Studies: Proton Therapy vs. Photon Therapy
Speaker Brian Baumann, MD, assistant professor of radiation oncology at Washington University School of Medicine, talked about some comparative effectivness studies on proton therapy from a standpoint of value for acute and late toxicities. He discussed results of these studies in which proton therapy was associated with significantly fewer adverse events than photon radiotherapy. He referred specifically to a trial comparing proton to photon therapy for esophageal cancer where proton therapy significantly reduced the overall toxicity burden without worsening disease control outcomes. He also mentioned two recent studies that reported that proton therapy had a much lower risk of second cancers compared to IMRT.
As Dr. Mehta did, Dr. Baumann also discussed the major benefits of proton therapy over photon therapy for children with medulloblastoma. A study looking at 79 patients – 37 proton and 42 photon – who were treated with the same medulloblastoma protocols, found the proton cohort exhibited superior long-term outcomes in IQ, perceptual reasoning and working memory. In fact, the proton group had stable scores, from pre-radiation to post-treatment, in all domains except for processing speed, while the photon group had significant declines on all intelligence measures.
Successful Appeal Letter Writing
Isaac Valdez, vice president of clinical operations and business development at Apollo Healthcare, covered the steps involved in building an effective strategy for insurance appeal letter writing. Apollo Healthcare, established just last year, specializes in proton therapy access, prior authorization, referral management, and other operating functions. Their main goal is to “drastically improve the way patients gain access to advanced cancer treatments like proton therapy.”
Mr. Valdez directed his presentations to the proton centers, as most have dedicated teams of insurance appeals specialists on staff who fight for coverage on behalf of their patients, but we think the information will also help patients compose their own appeal letters.
According to Dr. Valdez, here are three components every appeal letter should include:
- Data: Include all pertinent data, such as the denial letter and other documentation.
- An Understanding of Your Audience: Know the different payor types – government group, self-funded plan, etc., as each has their own policies and guidelines.
- A Compelling Story: Explain why proton therapy is the best option for you.
He then explained the methodology for successful appeal letter writing:
- Begin with a desired outcome. This includes a request for an urgent review of your appeal in a timely manner. Also request a case-matched reviewer to be the decision-maker on the appeal.
- Include detailed information on the patient’s diagnosis and clinical history (age, medical complications including anatomy, genetic dispositions, and any “pertinent” co-morbidities) and exclude any information that doesn’t add to the case.
- Incorporate dosimetry details, making sure it’s easy to read and understand.
- Review, understand, and include the medical policy that the payor is basing the denial decision on. This lets the payor know you’ve done your homework. You may even find that some of the references used in the denial are outdated.
 Mr. Valdez also encourages patients to include images – diagnostic images, CT scans – in their appeals. “A picture is worth a thousand words,” he said. “Sometimes it’s better to just include a screenshot of your tumor versus describing it in text format.”
Mr. Valdez also encourages patients to include images – diagnostic images, CT scans – in their appeals. “A picture is worth a thousand words,” he said. “Sometimes it’s better to just include a screenshot of your tumor versus describing it in text format.”
Lifetime Achievement Award Winner
The National Association for Proton Therapy honored their 2021 Lifetime Achievement Award winner, Mr. Yves Jongen, world-renowned researcher and scientist, and founder of IBA (Ion Beam Applications). “Yves joins an illustrious group of distinguished NAPT Lifetime Achievement Award recipients including Mr. Len Arzt, Mr. Bob Marckini, Dr. James Cox, Dr. James Slater, Dr. Herman Suit, and Dr. George Laramore,” said speaker Bradlee Robbert, director of operations at UF Health Proton Therapy Institute. “All of these recipients have a history of distinguished service within NAPT and have greatly impacted proton therapy through innovation, advocation, education, and leadership. These are the core principles that we look for in nominees, and our 2021 recipient excelled in all of these qualities.” Mr. Robbert then played a special video detailing Mr. Jongen’s career.
Mr. Jongen founded IBA with a goal to advance particle therapy by inventing and developing a cyclotron particle accelerator that could accelerate charged particles up to half the speed of light through a magnetic field. Convinced that cost was the largest impediment to making proton therapy available to more patients, he then focused his attention on the development of a compact proton therapy system, resulting in the development of a single room solution that dramatically reduced the total cost associated with establishing a proton therapy center.
Congratulations to Mr. Yves Jongen!
The Future of Proton Therapy: Two Possible Paths
Brian Baumann, MD of Washington University School of Medicine, described two paths that the future of proton therapy could take. “There’s the path that I hope it goes down, and there’s the path that it might go down unless it’s given proper support by the government,” he said. He described that path as the “expensive, limited-value treatment that is strangled by the payors who don’t want to pay for it. And then this incredibly promising technology that has undeniable dosimetric advantages over X-ray withers on the vine.” Dr. Baumann said this is the reason he passionately defends proton therapy and has been arguing that the RO APM should exclude protons. “If you have a bundled payment model, and you include more expensive therapies like proton, you really could stunt the ability of the proton therapy community to generate the comparative effectiveness research that’s able to show that this treatment may be more expensive in the short term, but it actually pays for itself in the long run through reduced toxicity, less hospitalizations, etcetera.”
“If proton therapy is given the chance that it deserves,” Dr. Baumann continued, “then I think the future is very bright.” If proton therapy follows this path, he sees the treatment becoming much more common in 10 years, perhaps with most large centers having at least one proton machine. “And then perhaps proton therapy becomes the default modality for a lot of disease sites.”
Summary
We were blown away by the presentations and the amount of content at this conference. In the past year and a half, the proton therapy community has faced extreme challenges, but we’ve clearly persevered and continue to make extraordinary progress in advancing proton technology and improving access to proton therapy for cancer patients. We will continue to fight for proton therapy and hope to meet face to face with others in the proton community at the 2022 conference.



Last Month’s Brain Teaser
The statement below has been encoded using a simple substitution cipher: Each letter has been replaced with a different one, and the substitutions remain constant throughout. Can you decode it?
PVOTA QPT EQKT SMP CTMCOT UZM QPTX’N UJOOJXD NM EQWT VC NZTIP MUX. ─ LZVLW GTQDTP
Answer: Rules are made for people who aren’t willing to make up their own. ─ Chuck Yeager
Winner: The winner – a northern New Jersey resident, treated at LLUCC in 2008 – wishes to remain anonymous. Although, he did tell us he’s become somewhat of a “marketer” of Bob’s book after having read it and met Bob when he was visiting Loma Linda. “I told Bob his book almost convinced me to be treated with proton therapy … but it was Penn Medicine spending $280 million to build their own center that pushed me over the edge.”
New Brain Teaser
Something extraordinary happened on the 6th of May 1978 at 12:34 a.m. What was it?
Send your brain teaser answer to [email protected] for a chance to win a signed copy of Bob Marckini’s NEW second edition book, You Can Beat Prostate Cancer.
Top 10 Remarks by Golf Caddies (Source)
Golfer: Think I’m going to drown myself in the lake.
Caddy: Think you can keep your head down that long?
Golfer: I’d move heaven and earth to break 100 on this course.
Caddy: Try heaven ─ you’ve already moved most of the earth.
Golfer: Do you think my game is improving?
Caddy: Yes sir ─ you miss the ball much closer now.
Golfer: Do you think I can get there with a 5 iron?
Caddy: Eventually.
Golfer: You’ve got to be the worst Caddy in the world.
Caddy: I don’t think so, sir. That would be too much of a coincidence.
Golfer: Please stop checking your watch all the time. It’s a distraction.
Caddy: It’s not a watch ─ it’s a compass.
Golfer: How do you like my game?
Caddy: Very good, sir, but personally, I prefer golf.
Golfer: Do you think it’s a sin to play on Sunday?
Caddy: The way you play, sir, it’s a sin on any day.
Golfer: This is the worst course I’ve ever played on.
Caddy: This isn’t the golf course. We left that an hour ago.
…and the #1 best Caddy comment:
Golfer: That can’t be my ball ─ it’s too old.
Caddy: It’s been a long time since we teed off, sir.
Now That I’m Older … (Source)
Kids today don’t know how easy they have it. When I was young, I had to walk nine feet through shag carpet to change the TV channel.
Remember back when we were kids and every time it was below zero outside they closed school? Yeah, me neither.
I may not be that funny or athletic or good looking or smart or talented … I forgot where I was going with this.
I love approaching 80. I learn something new every day and forget five other things.
A thief broke into my house last night. He started searching for money, so I woke up and searched with him.
I don’t always go the extra mile, but when I do it’s because I missed my exit.
On Dieting … (Source)
My goal for 2020 was to lose 10 pounds. I have only 14 to go.
I needed to lose some weight, so I went on a three-month diet plan. I don’t want to brag, but I just finished it in 72 hours.
I know you’re supposed to eat three meals a day, but how many should I eat at night?
My doctor asked, “What’s your favorite exercise?” I replied, “Chewing.”
My fitness coach told me to bend down and touch my toes. I said, “I don’t have that kind of relationship with my feet. Can I just wave?”



Estate Planning Hints
BOB Member Ron Hendricks is Director, US Foundation for Trinity Western University. He regularly copies us on his “News from Ron” mailings, which are helpful hints on estate planning to the readers of his newsletters. We have found Ron’s suggestions to be timely and beneficial. With his permission we periodically share some of his wisdom with our membership. This segment is called . . .
Creating a Will
“Though it may seem hard to believe, I have never gotten around to making a will, but I’d like to do so now. My question is: Do I need to hire a lawyer to write my will, or can I draft it myself?”
It’s not hard to believe at all. Fewer than half of North American adults have a will, mainly because they haven’t gotten around to it, or they have put it off because they don’t want to think about dying. Having a will is important because it ensures that your money and property are distributed to the people and charities you desire to receive it after your death. If you die without a will, your estate will be settled in accordance with your state law. Details vary by state, but assets typically are distributed using a hierarchy of survivors. Assets go first to a spouse, then to children, then your siblings and so on.
The Question Remains … Do You Need a Lawyer?
It’s best to seek professional advice, especially if you have significant financial assets or a complex family situation like a blended family or a child with special needs. An experienced lawyer can help avoid family confusion, dysfunction, and squabbles after you’re gone.
Where to Store It?
Once your will is written, the best place to keep it is in a fireproof safe, a file cabinet at home, or in a safe deposit box at your bank. Make sure your executor knows where it is and has access to it. If a professional prepares your will, keep the original document at your lawyer’s office as well as a digital copy in the cloud. Also, be sure to update your will every three to five years, especially if your family or financial circumstances change or if you move to a different state.
Did you know? (Source)
- One quarter of your bones are in your feet. It’s true. There are 206 bones in your body and 52 of them are in your feet – 26 in each foot.
- The inventor of the Pringles can is buried in one. Fredric Baur developed the product in 1966 while working for Procter & Gamble. He was so proud of his invention that he asked his family to put his ashes in a Pringles can after he died. When he passed away at age 89, his children stopped at a Walgreens on the way to the funeral home to pick up the can.
- The Goodyear Blimp is the official bird of Redondo Beach. Redondo Beach is located close to Carson City, the Goodyear blimp’s home airport. In 1983, the city of Redondo Beach passed a resolution to make the blimp its official bird.
- Outer space is a one-hour car ride away. The Karman line, an altitude of 100 km (62 miles) above sea level is conventionally used as the start of outer space. So, if you could drive straight up, at a speed of 62 mph, you’d reach outer space in an hour.
- A cornflake in the shape of Illinois sold on eBay for $1,350. Two Virginia sisters discovered a cornflake, in 2008, that was shaped like the state of Illinois and put it up for sale on eBay. Monty Kerr, a trivia website owner from Austin, TX paid $1,350 to place it in his traveling pop culture museum.
Quote of the Month:
“The fact that we live at the bottom of a deep gravity well, on the surface of a gas-covered planet going around a nuclear fireball 90 million miles away and think this to be normal, is obviously some indication of how skewed our perspective tends to be.” – Douglas Adams



You’re Never Too Old to Dream
These people prove we can all get better with age …
Faujah Sing: Marathon Man
In February 2013, Faujah Sing became the oldest person to run a marathon at age 101. Astonishingly, Sing only began racing at age 89 after losing his wife and son but has since completed eight competitive races.
Min Bahadur Sherchan: Peace Maker
Min Bahadur Sherchan is the oldest person to reach the world’s highest peak, climbing Mt. Everest at the age of 76. Sherchan scaled the 29,035-foot mountain in May 2008 and at age 81, still holds the Guinness World Record for his accomplishment. Says Sherchan, “My main objective for climbing Everest was for world peace. I was determined to either climb the peak or die trying.”
Ida Keeling: Record Breaker
In 2012, 97-year-old Ida Keeling set a record for the 100 Meter Sprint at the USA Track and Field Eastern Regional Open Championships. She finished the race at 51.85 seconds, beating the previous record of 59.9 seconds for the 90-and-over age category. Keeling took up running at age 67 after several personal tragedies in her life, including the death of her husband and two of her sons.
Kane Tanaka: Last Woman Standing
The oldest verified living person is 118-year-old Kana Tanaka, from Japan. There are several others who’ve lived between 115 and 120 years, and one lady, Jeanne Calment from France, who lived 122 years and 164 days.
One of our members and a good friend of ours is 79 years old. His mother celebrated her 110th birthday on April 1. We wouldn’t be surprised if she breaks Tanaka’s and Calment’s records for longevity.
Low PSAs to all,
Bob Marckini and Deb Hickey
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
NO MEDICAL ADVICE: Material appearing here represents opinions offered by non-medically-trained laypersons. Comments shown here should NEVER be interpreted as specific medical advice and must be used only as background information when consulting with a qualified medical professional.