Dear Members (a note from Deb Hickey):
Ugh. It’s inevitable that bad things happen. You miss your flight. Your car is stolen. Your cat dies. And sometimes, really bad things happen. These things drown out everything else in your life. They cut you to the bone. They force you to reconsider who you think you are.
Most of you reading this are familiar with one thing in particular – being diagnosed with “The big C.” Being told you have cancer is like an unexpected knuckle thrust to the throat. And then your life is changed forever.
Then what?
If you are blessed to come out the other side, you could change your life’s direction and use your experience to help others. As I’ve written several times before, that’s what my father Bob Marckini did. After his prostate cancer diagnosis and treatment, he joined the Loma Linda University Cancer Center Advisory Council, presented at proton-related events around the country, counseled newly diagnosed men and their family members from all over the world, launched the BOB organization, and wrote two books. Many have told us he’s saved their lives. And ─ soon to be 78 ─ he’s still at it, as you know.
My dad could have gone through treatment and spent his 60s and 70s retired, with a golf club in one hand and a snorkel in the other. But instead, he chose to make something awesome out of something awful.
Pastor and author Charles R. Swindoll said, “Life is 10 percent what happens to you and 90 percent how you react to it.” He emphasized the importance of attitude – and that we have a choice as to the attitude we embody. Granted, it’s not always easy to wake up and say, “I think I’d like to be positive today,” when your house has just burned down. It takes practice. It takes work. But it is possible.
A month ago, my daughter’s school announced they’d invited a guest speaker (virtual) by the name of Chris Waddell to share his story with students and families. He was going to talk about making opportunities out of tragedy. I’d never heard of Mr. Waddell, but I thought the topic was interesting, so I marked my calendar. The presentation was last week, and it took about three minutes before my jaw dropped and the tears flowed. Read about Chris Waddell and how he turned tragedy into triumph in our Final Thought section this month.
Also, this month we provide an update on the COMPPARE trial – the first study of its kind comparing the quality of life, side effects, and cure rates for prostate cancer patients treated with proton therapy or photon therapy (IMRT). We also discuss the serious infections that can result from prostate biopsies, including one member’s frightening experience after he contracted sepsis. Can the flowering plant, black cohosh, help minimize the effects of ADT? Find out in this issue. And, we have an update on the extraordinary progress made in Israel where more than a third of their population has been fully vaccinated against COVID-19 … and much more!
Special note: Next month we have some exciting news to share from Loma Linda on a new cancer therapy that will be a huge complement to proton therapy. Stay tuned!
As always, we welcome and encourage your feedback. Please send an email to [email protected].
Deb Hickey
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
In This Issue:
- Study Update: COMPPARE – Proton vs. IMRT for Prostate Cancer
- COMPPARE – A Patient’s Perspective
- Sepsis Infection from Prostate Biopsy – Frightening Story
- Black Cohosh for Hot Flashes Caused by ADT?
- COVID Vaccines Work!
- Featured Member Story: “If the Road Looks like a Snake, Take it!”
- Loma Linda’s Historic Philanthropic Effort Closes After Raising Millions
- Exercise is Good for the Brain



Study Update: COMPPARE – Proton vs. IMRT for Prostate Cancer
COMPPARE stands for “A Prospective COMparative Study of Outcomes with Proton and Photon RAdiation in PRostate CancEr.”
The COMPPARE trial will compare the quality of life, side effects, and cure rates for prostate cancer patients treated with proton therapy or photon therapy (IMRT).
Why should you care?
A study like this has never been done. And as you know, many health insurers refuse to cover proton therapy for
prostate cancer due to its higher cost and unanswered questions about its effectiveness compared to photon therapy. The COMPPARE study will attempt to answer the question, once and for all, as to whether or not there are discernible differences between proton therapy and IMRT in treating prostate cancer. Results of the study could resolve disagreements that are restricting patients’ access to proton therapy, particularly with regard to private medical insurers’ coverage and reimbursement policies.
Give me the details.
The study, which is being led by Nancy Mendenhall MD, Professor, Dept. of Radiation Oncology and Medical Director, University of Florida Health Proton Therapy Institute, will follow 3,000 men between the ages of 30-85 across the U.S. who will be treated with either protons (1,500) or IMRT (1,500). Participants will answer brief surveys regarding treatment choice, quality of life, and side effects for at least three years.
In addition, proton therapy patients can choose to participate in a randomized trial that will evaluate whether quality of life, side effects, and prostate cancer cure rates differ between patients receiving the standard treatment protocol (44 treatments) versus a shorter protocol (20-24 treatments).
Bob Marckini is on the study’s executive board and Deb Hickey serves as a patient stakeholder.
So, what’s the latest?
As of last month, there are 51 sites activated; 48 are enrolling participants; and we’ve reached 40 percent of our accrual goal. This is impressive, given the local and global challenges and slowdowns presented by
COVID-19.
“I am awed by the dedication displayed by our team, participating sites, patient stakeholder group, minority engagement group, and most of all our COMPPARE enrollees, to conduct research that will improve the ability of future patients to make informed decisions based on knowledge of the comparative outcomes of conventional radiation and proton therapy in prostate cancer.” ─ Dr. Nancy Mendenhall
Is it easier to obtain health insurance coverage if I’m on the trial?
This question was asked at our last COMPPARE team meeting, and unfortunately the answer isn’t completely clear. According to Dr. Mendenhall, there are several large insurance agencies that have agreed to cover patients if they’re on national comparative trials, however some of them agree only if those trials are randomized. Others will cover patients if the national trial is recommended by ASTRO for evidence development. “It’s regional,” Dr. Mendenhall explained. “For example, Blue Cross Blue Shield has many entities – all separate businesses with separate policies – and they’re not always consistent with each other.” Dr. Mendenhall noted that insurers are more likely to cover if the patient agrees to the randomized trial.
► BOB Comment: This doesn’t mean you shouldn’t appeal if you’re denied coverage. We’re seeing many denials overturned by those who fight and fight hard. Be sure to ask the proton center for help if you intend to appeal.
When will the trial be completed?
Although we may have an interim analysis around the two-year mark, final data will be reported in 2026.
COMPPARE – A Patient’s Perspective
 COMPPARE’s Patient and Caregiver Stakeholders are a diverse group of prostate cancer survivors and caregivers. They each provide valuable input which helps set priorities and ensure the trial is designed to answer questions important to them and those considering treatment for prostate cancer. One such stakeholder is John W. “Jack” Wilmer, Jr.
COMPPARE’s Patient and Caregiver Stakeholders are a diverse group of prostate cancer survivors and caregivers. They each provide valuable input which helps set priorities and ensure the trial is designed to answer questions important to them and those considering treatment for prostate cancer. One such stakeholder is John W. “Jack” Wilmer, Jr.
“Patient stakeholder participation in COMPPARE is important because the patient, more than anyone else, can best describe the experience of selecting a treatment alternative, and the results and effects of that treatment choice,” Jack said.
When Jack was diagnosed with prostate cancer in 2011, he began exhaustive research into his treatment options. He spoke with dozens of friends and acquaintances to gain their perspective, and also met with specialists at major brachytherapy, IMRT, and proton therapy centers. He ultimately chose proton therapy and was treated at the University of Florida Proton Therapy Institute (UFPTI).
Jack quickly gained perspective on the vital importance of proton therapy as he shared his gantry with young brain cancer patients, many of them children. They needed the precision offered by protons. Conventional radiation can cause nausea, extreme fatigue, trouble with speech and memory, as well as longer-term complications like learning difficulties and growth problems. Proton therapy, however, minimizes radiation exposure to healthy, growing tissue and therefore it’s ideal for pediatric brain cancer patients.
Jack became interested in being a part of the COMPPARE trial after a conversation with Dr. Nancy Mendenhall during his treatment. At the time, she was just developing the research study. “I hope that COMPPARE results in insurance companies and Medicare being as willing to cover proton therapy as they are for IMRT or other treatment alternatives, so that a patient’s choice of treatment is not affected by financial considerations,” he said.
Sepsis Infection from Prostate Biopsy – Frightening Story
 One of our members, “Lee,” recently wrote to tell us about a frightening experience he had as a result of his prostate biopsy.
One of our members, “Lee,” recently wrote to tell us about a frightening experience he had as a result of his prostate biopsy.
Lee underwent a standard 12-core transrectal ultrasound-guided (TRUS) biopsy in early 2020. Both prior and subsequent to the procedure, he took his prescribed Cipro antibiotic to minimize the risk of infection from the needle passing through the rectal wall into the prostate.
When his temperature spiked to well over 100° the day after the procedure, he falsely assumed he’d come down with COVID-19, never thinking it may be an infection from his biopsy. His primary care physician ordered a COVID test which was negative.
Lee’s temperature continued to rise over the next 24 hours. He began to experience severe chills and then started shaking uncontrollably. The hospital emergency room was his next stop. Blood tests in the ER revealed he had acute sepsis which was linked to his prostate biopsy.
His condition continued to deteriorate. He told us, “I was in critical condition at that point. It was now a race against time to find an IV antibiotic to counter the gram-negative E coli that had entered my bloodstream.” His body had rejected the Cipro antibiotic that he took before and after his biopsy.
After eight days in the hospital, followed by two weeks of home health care, Lee recovered from this very serious, life-threatening event.
He said the good news/bad news of the situation was that he tested negative for COVID, but positive for prostate cancer. “I feel blessed to have undergone proton therapy and am honored to be a member of the BOB,” he told us.
Serious infections from prostate biopsies are not that uncommon.
In Bob Marckini’s new book, he writes about this subject in Chapter 18, Ten Steps for Taking Control of the Detection and Treatment of Your Prostate Cancer. Step 4 states, “Manage Your Biopsy Test if Above Steps Lead to a Decision to Schedule a Biopsy.” In that section Bob states:
Unfortunately, about 5 percent of patients who undergo transrectal biopsies experience infections, including dangerous sepsis, with up to 3 percent requiring hospitalization. The reason for this is that the standard antibiotic given to patients prior to biopsy is Ciprofloxacin (Cipro). While Cipro is generally an excellent medication in a class of drugs called quinolone antibiotics, used to prevent and treat bacterial infections, a small percentage of patients have bacteria in their intestines that are quinolone resistant, which means Cipro may not prevent an infection.
A simple and inexpensive Culture and Sensitivity (C&S) test involves taking a swab of the rectal area and analyzing it for quinolone resistance. If the bacteria in your gut is quinolone resistant, your doctor can prescribe an alternative antibiotic, such as Doxycycline or Bactrim.
In the same chapter, Bob comments on a second technique for preventing infection:
Another alternative is to have the biopsy done through the perineum (space between scrotum and anus), as this prevents infection from fecal matter getting into the bloodstream. While not commonly done, this technique has been used over the years with much success in controlling infection.
This last technique reduces the probability of infection from 4-5 percent for the standard TRUS biopsy to less than 0.2 percent for the transperineal biopsy. We wrote about the benefits of the transperineal prostate biopsy in last month’s BOB Tales.
Lee learned about the C&S swab test mentioned above, but only after his harrowing experience. Why urologists don’t do this simple and inexpensive test for all patients prior to biopsy, we don’t know.
Lee’s experience is certainly a good reason why patients should take seriously the underlying theme of Bob’s book: to take control of your health; learn everything you can about your diagnosis and any medical procedure you are considering; ask questions; and get a second opinion.
 Black Cohosh for ADT Caused Hot Flashes?
Black Cohosh for ADT Caused Hot Flashes?
Androgen deprivation therapy (ADT) – also called hormonal therapy – is often prescribed to men who are being treated for moderate to advanced prostate cancer. It’s also commonly used for men with recurrent prostate cancer. We have lots of members who are on ADT.
Up to 80 percent of patients on ADT experience hot flashes (sometimes called hot flushes), and about a third of them report this as their most troublesome side effect. Sometimes the symptoms improve over time and other times they persist for as long as the patient is receiving ADT. These hot flashes can significantly impact a patient’s quality of life.
There are many medications, both prescription and over the counter, that can be used to treat hot flash symptoms with varying degrees of benefit. Prescription drugs that are commonly used to combat the effects of hot flashes include Megace (megestrol acetate), clonidine, gabapentin, and selective serotonin reuptake inhibitors (SSRIs).
We recently heard from a member who reported substantial improvement with his troublesome hot flashes after taking a natural substance called black cohosh. This herb is from a perennial plant native to North America and has a long history of use by American Indians for treating musculoskeletal pain, fever, cough, pneumonia, and menstrual irregularities. European settlers used black cohosh to support women’s reproductive health.
Black cohosh has been used more recently to treat menopausal symptoms (including hot flashes), heart palpitations, tinnitus, vertigo, sleep disturbances, nervousness and irritability.
In his note to us, the member said:
I don’t frequent health food stores or take a lot of vitamins; I’m generally a cynic about those sorts of things. I wouldn’t have tried the black cohosh if the recommendation hadn’t come from my physician. That said, I do believe it’s been of significant help.
I had my first Lupron shot in early or mid-July. By August I was having five or six hot flashes a day. They came on suddenly, and when they did, all I could do was stand still with my arms away from my sides and run sweat. Since I began taking the black cohosh, I’ve had fewer flashes; they’re far less severe; and they seem to be of shorter duration. So I’m a believer.
We can’t recommend black cohosh, but we do think it’s something you may want to discuss with your physician if you’re on ADT and are experiencing hot flashes.
COVID Vaccines Work!
 Alan Feingold, MD, Medical Director, Occupational & Environmental Medicine, South Miami Hospital, publishes daily reports on the status of the pandemic. His reports are based on data from the Institute for Health Metrics and Evaluation (IHME) at the University of Washington and other reliable sources.
Alan Feingold, MD, Medical Director, Occupational & Environmental Medicine, South Miami Hospital, publishes daily reports on the status of the pandemic. His reports are based on data from the Institute for Health Metrics and Evaluation (IHME) at the University of Washington and other reliable sources.
In a recent update, Dr. Feingold reported on the extraordinary progress made in Israel where more than a third of their population has been fully vaccinated. Out of the 3.4 million vaccinated people who were more than seven days after their second vaccine injection, only 4,711, or 0.14 percent were found to be positive for the virus, and of those, only 907, or 0.03 percent developed symptoms of COVID-19. “This is powerful evidence of vaccine effectiveness,” according to the Israeli health insurance organizations, known as Kupat Holim and the Health Ministry.
This same report is forecasting sharp declines in new cases throughout the U.S. as well as deaths from COVID-19. Based on the current trend, IHME projects that daily infections in the U.S. will drop from more than 65,000 on April 1, 2021, to fewer than 6,000 by July 1, 2021 (i.e. more than 90 percent). And, during that same period, daily deaths in the U.S. are projected to drop from 845 to 73 (also more than 90 percent). This is truly good news!
Subscribe to Dr. Feingold’s daily reports by emailing him at [email protected].
“If the Road Looks like a Snake, Take it!”
Introduction by Bob Marckini
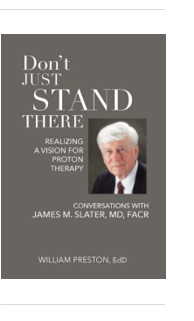
Jerry Slakoff is a dear friend. I first met him 16 years ago when he was researching treatment options for his prostate cancer. He chose proton therapy at Loma Linda and had excellent results. We’ve stayed in touch ever since.
Those of us who are old enough will remember a terrific TV series, Route 66, a CBS drama that premiered in October 1960. It was the story of two young men, Tod Stiles (Martin Milner) and Buz Murdock (George Maharis), who dropped everything to explore the country in a Chevy Corvette convertible, ostensibly to search for meaning in their lives; the story was about the human condition. They met people from all walks of life; they were in and out of trouble; and they were forced by circumstances to confront their demons.
Fast forward 60 years and picture this: an octogenarian and a nonagenarian in a fast and sleek sports car, and a story eerily similar to that of Milner and Maharis. The following short story is about a new chapter in Jerry Slakoff’s life, in his own words. At one point on this latest journey, his 90-year-old riding partner, who was at the wheel asked, “Where do you want to go next?” Jerry’s responded, “Just look at the map. And if the road looks like a snake, take it!”
“Keep going, guys …”
By Jerry Slakoff
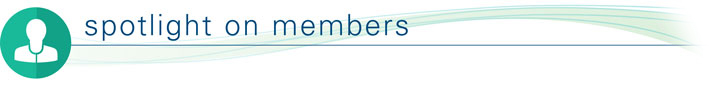
What do you do after prostate cancer at age 68? The first thing I did was to get on my Goldwing motorcycle and spend the next 18 glorious years touring the USA, Canada, and Mexico from April through September each year. I rode a total of about 360,000 miles on back roads, over mountain passes, through awesome national parks and breathtaking scenery from 200 feet below sea level to the thinnest air I have ever been in at 14,400 feet above sea level. I’m 83, and after a motorcycle riding career of 30 years and 800,000 miles in the saddle, I decided to pack it in.
 So, I asked my good friend Ed Pittman, a great driver at 90-years-young, a car collector, and past president of the Sedona Car Club with a doctorate in geology, if he would like to take a 10-state tour throughout the Northwestern part of the U.S with me.
So, I asked my good friend Ed Pittman, a great driver at 90-years-young, a car collector, and past president of the Sedona Car Club with a doctorate in geology, if he would like to take a 10-state tour throughout the Northwestern part of the U.S with me.
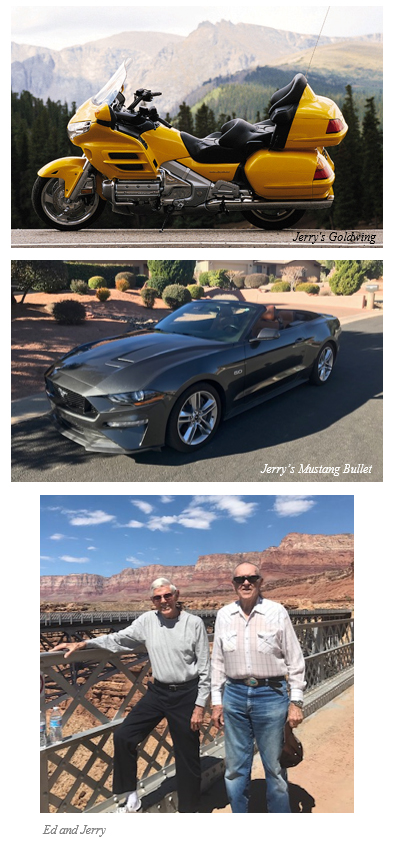
An immediate “YES!” prompted the next question, “What kind of car would make the trip lots of fun?” A fleeting moment was spent contemplating the possibility of a 2020 mid-engine Corvette. Looking at each other, we started to laugh. Knowing that the car was about four inches off the ground. I said, “Sure, we won’t have to go to the gym during the trip because every time we get out of the car, we’ll have to roll out onto the street and climb up the side of the car to stand.”
After some more discussion about the pros and cons of each option, I concluded that a 2020 GT Mustang Bullet with 500+ ponies – that are anxious to get up and go – would be a hoot to carve out the mountain roads that were awaiting us.
Taking this trip with your own private geologist was a spectacular benefit I never expected. Ed methodically explained all the types of mountain ranges, lava fields, canyons, and how this magnificent earth that we were traveling over was formed. We took turns driving three-hour shifts with the majority of the roads being those that had plenty of zigs and zags, lots of mountains and NO interstates. Ed was ecstatic that I was able to find such great roads. I let him know I’d traveled on most of them before, only on a motorcycle. I said, “Just look at the map, and if the road looks like a snake … TAKE IT.”
Ed was driving as we approached Winthrop, WA. The speed limit had been 70 mph, but as we got closer to town, a speed limit sign read 25 mph. Rather than jamming on the brakes, he coasted into town at about 40 mph.
Bingo! The obvious speed trap instantly produced the local sheriff – clearly a speed trap for tourists. “License and registration please. You do know there’s a 25 mph limit in town,” said the officer.
Ed gave him his license and told the officer that his passenger/friend was the owner of the car and had the registration. I asked if it was all right to get the temporary papers out of the glove box and he said, “Sure.” As I looked for the papers, I glanced over to see the officer holding Ed’s license in one hand, reading it, and in the other hand he started to count with his fingers as he was mouthing “… 50 … 60 … 70 … 80 … 90.” The officer looked at us and said, “Hey, you guys are no spring chickens! I never gave a ticket to a 90-year-old and I’m not going to start now. Take it easy and have a good time, gentlemen. And by the way, that’s one nice looking car.” ─ Jerry Slakoff, Proton Graduate, March 2005
Jerry’s message to our members:
“Keep going guys … you have plenty of good times ahead of you.”
Coloradan Members Stepped Up
Colorado State Rep. Karen McCormick is proposing legislation to make it easier for Coloradans to access proton therapy by prohibiting insurers from applying a higher standard of clinical evidence for coverage of proton therapy than the health benefit plan applies for other radiation therapy treatment, as well as using “experimental” as a justification for denying treatment.
Rep. McCormick’s team contacted the BOB for help in finding former proton therapy patients living in Colorado who’d be willing to share their proton stories in support of the Bill. Deb Hickey sent an email to more than 200 Coloradoan BOB members. Many of them not only volunteered to share their stories, they offered to testify in favor of the bill at a committee meeting. We were proud of the responses we received from members and Rep. McCormick’s team was thrilled and thankful.
Following is one member’s response to our request.
I’m a proponent of proton therapy as I’m among thousands of men who’ve been treated successfully. More than 15 years ago I was diagnosed with prostate cancer … I was determined to find the best treatment and thus found myself scheduled for DaVinci surgery in Denver. As an engineer I thought I’d found the best treatment available. Not so. I found out about proton therapy (a story in itself); cancelled my surgery; and headed for Loma Linda. I’m so glad I did. Today many proton centers have been built around the world. In my view, it’s proven technology. It’s expanded to treatments of other diseases affecting men and women. I will help you in any way I can above and beyond testifying in favor of this bill.
Thank you to all our Coloradan members who responded to our request for help. This is what the BOB is all about!
We were recently informed the bill has been delayed. Stay tuned as we learn more.

Historic Philanthropic Effort Closes After Raising Millions
 Loma Linda University Health announced a record $476,832,220 was raised for Vision 2020 – The Campaign for a Whole Tomorrow. The conclusion of the eight-year fundraising effort, which advanced the organization’s goal of furthering clinical care, education, and research, was celebrated during a virtual celebratory event last month
Loma Linda University Health announced a record $476,832,220 was raised for Vision 2020 – The Campaign for a Whole Tomorrow. The conclusion of the eight-year fundraising effort, which advanced the organization’s goal of furthering clinical care, education, and research, was celebrated during a virtual celebratory event last month
Richard H. Hart, MD, DrPH, Loma Linda University Health president, expressed his sincere appreciation to each and every person who supported the campaign for contributing to the success of such an amazing accomplishment.
“We are so grateful for each supporter who gave through their commitment to our mission,” he said. “It is because of the unwavering support of our donors who responded beyond our expectations that Vision 2020 has had an incredible impact on our campus and has made a difference in the lives of those we serve every day.”
The $476 million raised exceeded the campaign’s original goal of $366 million. This was the largest philanthropic effort ever undertaken by Loma Linda University Health, with the funds going toward:
- Clinical care: to construct a new adult hospital and expanded children’s hospital, designed to meet California’s seismic building codes for healthcare facilities;
- Education and research: to support the training of the next generation of healthcare professionals, and challenge the boundaries of scientific research at Loma Linda University Health;
- Wholeness: to expand knowledge and practice for how people around the world can enjoy lives of wholeness and health.
Rachelle Bussell, senior vice president for advancement, echoed Hart’s gratitude to everyone who supported the campaign.
“Together, we have accomplished something truly remarkable,” she said. “As Vision 2020 comes to its conclusion, it’s exciting to realize this isn’t actually the end of something, but the beginning of a bright future for Loma Linda University Health.”
Many of our members contributed to Vision 2020. We are deeply grateful – because of you, Loma Linda is transforming the future of healthcare.
If you’d like to make a gift to thank Loma Linda University Health for their pioneering efforts that made your proton treatment possible, or to acknowledge the BOB organization for our BOB Tales newsletter or the services we provide, please consider one of the following.
- Donate to proton research online.
- Write a check to LLUCC Proton (Put “Marckini Chair” on the memo line) and mail to LLUH, Office of Philanthropy P.O. Box 2000, Loma Linda, CA 92354.
- Make an unrestricted gift (put “unrestricted” on memo line) so LLUH can use it where it’s needed most.
- Call Regina Joseph at 909-558-5010 to donate over the
- phone and/or to inquire about naming opportunities.
There are still books left!
 In an effort to boost funding for basic and clinical proton therapy research on prostate cancer, pancreatic cancer, liver cancer, breast cancer, and more, we asked our members to donate $100 (or more) to Loma Linda University Cancer Center. In return, they’d receive an advanced copy of Dr. William Preston’s book, Don’t Just Stand There – Realizing a Vision for Proton Therapy: Conversations with James M. Slater, MD, FACR. The response so far has been phenomenal. Thank you to all who’ve requested a copy.
In an effort to boost funding for basic and clinical proton therapy research on prostate cancer, pancreatic cancer, liver cancer, breast cancer, and more, we asked our members to donate $100 (or more) to Loma Linda University Cancer Center. In return, they’d receive an advanced copy of Dr. William Preston’s book, Don’t Just Stand There – Realizing a Vision for Proton Therapy: Conversations with James M. Slater, MD, FACR. The response so far has been phenomenal. Thank you to all who’ve requested a copy.
There are still books left! So, if you’d like a pre-published copy of this awesome book that likely won’t be available to the public until next year, please send a check for $100 or more, payable to “Loma Linda University Proton Cancer Research” and mail it to:
Loma Linda University Health ● Office of Philanthropy
PO Box 2000 ● Loma Linda, CA 92354
Please notify Deb Hickey at [email protected] that you’ve sent in your check and your book will be mailed immediately.
This book, which contains high-quality color images and illustrations, is not only about Dr. Slater’s quest to create the world’s first hospital-based proton treatment center, it’s also a teaching guide. As the Proton Treatment & Research Center at Loma Linda was such an immense endeavor, Dr. Slater wondered if the aspects of conceiving, planning, and orchestrating such a project, among others he undertook, might be instructive to others. Over the years, he’d also met people in all walks of life, many of whom had dealt with large and complex problems. He was struck by some of the stories they told about their work: although the fields or disciplines usually had nothing to do with medicine, many experiences were similar. And so, he kept this in mind while he worked on the book with Dr. Preston.
We’re sure you’ll thoroughly enjoy the book and we know it will occupy a place of honor in your home. And, you’ll be helping to fund basic and clinical proton research on prostate cancer, pancreatic cancer, liver cancer, breast cancer, and much more with your tax-deductible gift. Thank you!


 You Can Beat Prostate Cancer: And You Don’t Need Surgery to Do It – Second Edition
You Can Beat Prostate Cancer: And You Don’t Need Surgery to Do It – Second Edition
We are up to 70 reader reviews on Amazon. Almost all are five-star. Last month we reported on our first poor review from a reader who became sold on proton therapy, only to learn halfway through the book that younger men with private insurance would likely be denied coverage. So, he chastised us for not mentioning this earlier in the book. We’ll take care of that in the next edition.
We should point out that some younger men who have been initially denied coverage are winning their appeals and having their proton therapy paid for; it sometimes takes a lot of work. Others are discovering that some of the larger private insurers will pay for proton therapy if the patient is participating in a clinical trial, such as the COMPPARE or PARTIQoL trials comparing proton therapy to IMRT. When these trials are completed, we are hoping and expecting that private insurers will have no choice but to pay for proton therapy.
Following is the latest review on Amazon – one of the best we’ve seen.

Prostate issues? This is the place to start. If you’ve been diagnosed with prostate issues you will probably be in denial (Me? Cancer? No way!). You may feel lost and overwhelmed. I did.
Most likely your doctor will not recommend a specific course of treatment, but will lay out a bewildering set of options. Mine did.
Don’t go into the decision process blindly and DO NOT opt for surgery without a clear understanding of the other courses open to you. You must take control of your own health plan. Here’s what to do:
1) Don’t panic. You have many good choices.
2) Bring your loved ones into the discussion. They will be your support and your strength.
3) BUY THIS BOOK! Written by a self-described “recovering engineer,” the author, Robert Marckini, goes through the options, the treatments, the pros and the cons. The writing is direct, straightforward, and clear enough for a reader with only basic medical knowledge. However, for the detail oriented there is a wealth of information, citations, and referrals to other sources in the index and attachments.
If your goal in selecting a treatment plan is to be able to say, “I made the best decision I could,” this book is your essential tool.
Did you find Bob's new book valuable?
Please write a review on Amazon.
And remember, we’re happy to discount books in quantity (minimum 20) to anyone interested in spreading the word on proton therapy. Just send an email to [email protected]. Proceeds from book sales are used to help fund our efforts and to support proton therapy research.
The Kindle version is free to Kindle Unlimited members or can be purchased for $9.99 for non-members. The paperback price is $22.45
Buy You Can Beat Prostate Cancer second edition on Amazon or Lulu Press.


Exercise is Good for the Brain
 Drs. Mehmet Oz and Michael Roizen published an article last month in the Houston Chronicle and it was picked up in several other media outlets. The title of the article is, Physical Activity Plays Key Role in Boosting Brain Power. This subject should be of great interest to our members.
Drs. Mehmet Oz and Michael Roizen published an article last month in the Houston Chronicle and it was picked up in several other media outlets. The title of the article is, Physical Activity Plays Key Role in Boosting Brain Power. This subject should be of great interest to our members.
It’s been widely known that regular exercise can result in significant benefits for the heart, liver, lungs, digestion, and endocrine systems, as well as other bodily functions. But, they say, the most important benefit is to aerobic fitness and cognition. The article points out:
Studies have shown that when you exercise regularly, you have better mental health (less depression), stronger decision-making skills (executive function), and are less prone to dementia. You also have better neural function and efficiency because exercise-increased blood flow, ups “food delivery” of glucose and lipids to the brain and increases available oxygen. And the more you exercise, the more physical and cognitive reserves (that is, “backup”) you build up.
The brain neurotransmitter, dopamine, seems to play an important role in this process. A recent study, published in Medicine & Science in Sports & Exercise, reported this finding. Dopamine plays a key role in brain function and cognition. It is produced when you exercise. An hour of yoga, six days a week increases dopamine levels according to one study. And, while exercise stresses your body, in a healthful way, it also reduces the hormone, cortisol, which is produced by emotional stress. This is clearly a win-win.
The authors recommend 300 minutes of physical activity weekly, including 20 minutes of aerobics/cardio three times a week. They also suggest that improving your nutrition can reinforce the brain benefits of exercise. Iron, niacin, folate, and vitamin B6 deficiencies can reduce dopamine levels that could negatively impact your brain and emotions. They recommend visiting the National Institutes of Health’s website to find which foods contain these important nutrients.


We’ve been producing BOB Tales newsletters monthly for more than 20 years. During this time there have been articles that many new members haven’t seen, and some older members may have forgotten. So, we periodically re-run articles from past newsletters. This one from August 2006 is titled:
Prostate Radiation Doesn’t Increase Rectal Cancer Risk
Men who receive radiation therapy for prostate cancer are not at any appreciable increased risk of developing rectal cancer compared to those not given radiation therapy, according to a new study. Researchers have hypothesized that one disadvantage of using radiation to kill the cancer cells in the prostate is that it might also make men more likely to develop cancer in the nearby rectum.
Doctors found that rectal cancer developed in 0.7 percent of men who received radiation, 0.3 percent of men treated with surgery, and 0.8 percent of the men given neither treatment. Earlier studies had suggested a link between radiation and rectal cancer, but once doctors had adjusted for the age differences between all the men in the irradiated and non-irradiated groups, they could not find any significant increased risk of rectal cancer in the irradiated men compared to those not given radiation therapy.

National Proton Conference: Next month!
 The National Association for Proton Therapy (NAPT) is the voice of the proton therapy community ─ providing education and awareness for the public, professional, and governmental stakeholders about the benefits of proton therapy for treating cancer.
The National Association for Proton Therapy (NAPT) is the voice of the proton therapy community ─ providing education and awareness for the public, professional, and governmental stakeholders about the benefits of proton therapy for treating cancer.
Join NAPT for the ninth annual National Proton Conference, April 15 & 16, 2021. NAPT will bring together the community in a virtual format that builds on the success of their 2020 virtual education opportunities with the addition of new opportunities and features.
This year NAPT continues their mission to educate and increase awareness about the clinical benefits of proton therapy, ensure patients' choice and access, and to encourage cooperative research and innovation. NAPT is committed to move the proton industry forward and look forward. The proton community has united through the opportunities these challenging times have presented and their continued goal is to connect the brightest minds and visionaries in the field to advance the future of proton therapy ─ a future shaped by collaboration to initiate, illuminate, and innovate.
Topics will include …
- Latest research on proton therapy
- Proton therapy insurance coverage and reimbursement
- Flash therapy
- Developing and incorporating particle therapy into a cancer program
- Updates on key health policies impacting cancer care
- Trends in particle therapy for the future
- Ensuring value in alternative payment models



Last Month’s Brain Teaser
When liquid splashes me, none seeps through.
When I am moved a lot, liquid I spew.
When I am hit, color I change,
And color, I come in, quite a range.
What I cover is very complex,
And I am very easy to flex.
What am I?
Answer: I’m your skin!
Winner: The winner of the March BOB Tales Brain Teaser is Rees Harward from Midlothian, TX.
Rees was diagnosed with prostate cancer on March 8, 2016. “My wife and I didn’t know what to make of my diagnosis and had no idea what we were going to do about it,” said Rees. “I remember feeling scared, apprehensive, and somewhat in denial.”
Rees’ urologist suggested surgery, but fortunately for him, there were two life experiences he’d had that prompted him to question that suggestion.
Rees’ father, who passed in 1998, was a family physician in southern California. “You’d think I’d believe a doctor’s opinion is gospel having had a father who was a doctor,” Rees said. But he remembered his dad making house calls in the 50s and 60s. When he knew he couldn’t help a patient, he’d recognize his limits and send them to a major hospital, like Loma Linda University Health, where they could get the care they needed. This told Rees his dad’s patients and their needs were his priority; He didn’t always assume he knew best.
The other experience Rees had was with his youngest son. He was born with a serious heart defect. His doctor suggested he have surgery immediately or he’d die. Then he said something that might be surprising to some, but not to Rees because he’d grown up watching his father. His son’s doctor suggested his son not be treated at the hospital where he worked because they didn’t have much experience with the surgical procedure his son needed. Instead, the doctor recommended a hospital in Birmingham, AL. The pediatric cardiologist there was the one who developed the procedure.
“We were on a plane that afternoon,” said Rees. “Thirty years later, my son is healthy and living a normal life, thanks to that doctor who cared more about his patient than the hospital he worked for.”
How does this relate to Rees’ prostate cancer? After his urologist recommended surgery, Rees was unsure, so he began his own research into treatment options. “I found proton therapy and the Loma Linda University Cancer Center website during an Internet search,” he said. “I remembered immediately that Loma Linda was the hospital my father would send his patients to, and a lightbulb went on.” After digging a little further, Rees found the ProtonBob.com website which led him to the Texas Center for Proton Therapy – just a half hour from his home in Midlothian. Everything was coming together.
Rees was treated with a combination of hormonal therapy and proton therapy in May 2017. Today, he’s doing well and says his experience made him and his wife stronger in their faith. “We’re so thankful to have witnessed God’s hand at work at the Texas Center, especially with the children. In fact, I’ve thought many times that God allowed proton therapy to be developed for children. I, and a lot of other old farts, are just a side benefit of proton therapy.”
New Brain Teaser
Four cars come to a four-way stop, all coming from a different direction. They can’t decide who got there first, so they all go forward at the same time. They do not crash into each other, but all four cars go. How is this possible?
Send your brain teaser answer to [email protected] for a chance to win a signed copy of Bob Marckini’s NEW second edition book, You Can Beat Prostate Cancer.
Sometimes Kids are the Only Ones to Make Sense
 A 3-year-old boy went with his dad to see a litter of kittens. On returning home, he breathlessly informed his mother, “There were two boy kittens and two girl kittens!”
A 3-year-old boy went with his dad to see a litter of kittens. On returning home, he breathlessly informed his mother, “There were two boy kittens and two girl kittens!”
“How did you know?” His mother asked.
“Daddy picked them up and looked underneath,” the boy replied. “I think it’s printed on the bottom.”
Another 3-year-old put his shoes on by himself. His mother noticed that the left shoe was on the right foot. She said, “Son, your shoes are on the wrong feet.”
He looked up at her with a raised brow and said, “But Mom. They’re the only feet I got!”
On the first day of school, about midmorning, the kindergarten teacher said, “If anyone has to go to the bathroom, hold up two fingers.”
A little voice from the back of the room asked, “How will that help?”
Comedian George Carlin on Aging
Do you realize that the only time in our lives when we like to get old is when we’re kids? If you’re 10 years old or younger, you’re so excited about aging that you think in fractions. “I’m four and a half.”
When you get into your teens, you simply jump to the next number. “I’m gonna be 16.” You could be 12, but you’re gonna be 16. Eventually.
Then you finally become 21. Even the words sound like a ceremony. You become 21!
Then you turn 30. What happened there? Makes you sound like bad milk. He turned … we had to throw him out.
What’s wrong? What changed?
You become 21. You turn 30. You’re pushing 40. You reach 50. Then you make it to 60. By then you’ve built up so much speed, you hit 70. After that, it’s a day-by-day thing. You hit Wednesday …
When you get into your 80s; you hit lunch, you hit 4:30. And it doesn’t end there …
Into the ’90s, you start going backward. “I was just 92.”
Then a strange thing happens. If you make it over 100, you become a little kid again. “I’m 100 and a half.”

Quote of the Month: “The only difference between a tax man and a taxidermist is that the taxidermist leaves the skin.” —Mark Twain




“What happened to your legs?”
“I went to my mailbox at the end of the street,” Chris said. “As I was getting out of my car and putting my chair together, this little girl rode by on her bike. She said, ‘What happened to your legs?’”
Chris Waddell always thought the lessons he learned in sports would provide the foundation for success later in life. As a promising ski racer at Middlebury College, VT in 1988, he had no idea how profoundly one moment could change and paradoxically enhance that conviction. On December 20 of that year, Chris’ ski popped off in the middle of a turn. He fell, broke two vertebrae, and damaged his spinal cord. He was paralyzed from the waist down.
Because of the accident, Chris learned and achieved more than he could have ever imagined. Just one year later, he was back on the slopes on a monoski. A little more than two years later, he was named to the U.S. Disabled Ski Team.
Chris went on to become the most decorated male skier in Paralympic history, winning 12 medals over four games. He was inducted into the U.S. Ski and Snowboard Hall of Fame and the Paralympics Hall of Fame. The Dalai Lama honored him as an “Unsung Hero of Compassion.” Middlebury College presented him with a Doctorate in Humane Letters. National Public Radio (NPR) named his 2011 commencement speech at Middlebury one of the “best commencement speeches ever.” He’s been featured in numerous publications, including Skiing Magazine, National Geographic Explorer, Forbes, and People Magazine who named him one of “The 50 Most Beautiful People in the World.” Chris has also appeared on Dateline and The Oprah Winfrey Show.
Chris is now a successful motivational speaker. He speaks to the resilience of the human condition, with topics ranging from leadership to adversity to quality of life. He founded the One Revolution Foundation to “create a world where individuals with disabilities are seen for their potential instead of their limitations.”
The little girl asked, “So, you’ll never walk again?”
“No, probably not,” Chris answered.
As she began to ride away, she said, “That’s too bad.”
Chris thought, I wanted to stop her and say, it’s really not too bad. I don’t know what I would have done had I not had my accident. But I highly doubt I would have been the best in the world at anything. That’s an amazing gift.
Watch a video about Chris’ 7-day climb up Mt. Kilimanjaro on a custom-made 4-wheel mountain bike. As the reporter telling the story said, “He climbed the tallest peak in Africa to be heard.”
“It’s not what happens to you. It’s what you do with what happens to you.”
Low PSAs to all,
Bob Marckini and Deb Hickey
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
NO MEDICAL ADVICE: Material appearing here represents opinions offered by non-medically-trained laypersons. Comments shown here should NEVER be interpreted as specific medical advice and must be used only as background information when consulting with a qualified medical professional.