Dear Members (a note from Bob Marckini):
About 18 years ago, during a visit to the Proton Treatment & Research Center at Loma Linda, I met William Preston, EdD, a medical educator, writer, and editor. Dr. Preston holds an appointment as Associate Professor of Radiation Medicine at Loma Linda University. We crossed paths several times over the years and became friends during the time he was collaborating with the late Dr. James M. Slater on several technical publications.
A few years ago, Bill began working with Dr. Slater on a book about his quest to create the world’s first hospital-based proton treatment center. I was honored to be asked to review the manuscript recently and was impressed with Bill’s writing style and especially his ability to capture the essence of the man and the genius, Dr. James Slater. Bill understood and clearly illustrated the monumental challenges Dr. Slater faced. I was also pleasantly surprised to see a section in the book about our organization, the Brotherhood of the Balloon – how and why we came to be, our mission, and our impact on the proton movement.
.jpg)
The book – yet to be published – has dozens of high-quality color images and illustrations, but my favorite is shown here – a photo of me with my hero, Dr. James Slater (“Call me Jim,” he always insisted).
One gentleman who played a prominent role in the Loma Linda project was Philip Livdahl. At the time the project started, he was deputy director of the Fermi National Accelerator Laboratory (Fermilab) in Batavia, IL. Phil became the chief physicist on the project, and, as fate would have it, when the project was nearing completion, he was diagnosed with prostate cancer. Phil became the first prostate cancer patient to be treated entirely with protons at Loma Linda. He later became a member of our group and a good friend. There are several photos of Phil in the book along with many others who played key roles in the development of the world’s first hospital-based proton center.
Our feature story this month is an abstract of this book and some of the details behind why Dr. Slater felt so strongly about proton therapy; how The James M. Slater, MD, Proton Treatment and Research Center at Loma Linda came to be; how and why the book title, Don’t Just Stand There, was chosen; and why the incredibly humble Dr. James Slater allowed this book to be written.
But here’s the best news: We’re also including information in this month’s BOB Tales on how you can get your hands on a copy of this awesome book long before it becomes available to the public. Be sure to click-through and read the story.
Another important article this month is on a breakthrough imaging technology that researchers and physicians consider a “game changer” in the staging of prostate cancer. Initially, the test was developed to help identify tiny prostate cancer lesions throughout the body when patients experienced a cancer recurrence after surgery or radiation. But many think this exciting new technology may also be an important tool in the staging of prostate cancer even before primary treatment. This is another article you won’t want to miss.
We also have an update on Medicare’s new rule on reimbursing for proton therapy, another topic that’s of great importance to our family members and friends who are interested in following our path to proton therapy for treating prostate cancer or other cancers.
Deb and I are occasionally in contact with an old friend who’s known and loved by so many of our members. He’s an individual who was instrumental in the growth and development of our group from the beginning, over 20 years ago. He’s also had considerable positive impact on my life. This month we are including two short articles and a great photo of our dear friend, Dr. J. Lynn Martell and his lovely wife, Karen.
There’s much more in this month’s BOB Tales. As always, we welcome and encourage your feedback. Please send an email to [email protected].
Bob Marckini
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
In This Issue:
- Special Story: “Don’t Just Stand There – Realizing a Vision for Proton Therapy: Conversations with James M. Slater, MD, FACR”
- New Imaging Technique is a “Game Changer”
- FDA Approves New Oral Hormone Therapy Drug for Prostate Cancer
- Medicare’s New Rule and Its Impact on Proton Therapy
- Exercise, Diet Can Immprove Bone Health for Prostate Cancer Patients
- Does Eating Late at Night Increase Cancer Risk?
- The Truth About Brain Supplements



Soon to be Released: “Don’t Just Stand There – Realizing a Vision for Proton Therapy: Conversations with James M. Slater, MD, FACR”
By William Preston, EdD
Where It All Began
 Proton radiation therapy has been available since the mid-1950s, but until 1990 only in physics laboratories that featured accelerators not specifically designed for patient treatments. That year, however, Loma Linda University Medical Center opened the first hospital-based proton facility in the world. Today there are 37 treatment-dedicated proton facilities in the United States, and more than 50 others in countries across the globe. It all started at Loma Linda, thanks to the vision, research, and persistence of Dr. James M. Slater.
Proton radiation therapy has been available since the mid-1950s, but until 1990 only in physics laboratories that featured accelerators not specifically designed for patient treatments. That year, however, Loma Linda University Medical Center opened the first hospital-based proton facility in the world. Today there are 37 treatment-dedicated proton facilities in the United States, and more than 50 others in countries across the globe. It all started at Loma Linda, thanks to the vision, research, and persistence of Dr. James M. Slater.
Dr. Slater died on Dec. 26, 2018, just a few days shy of his 90th birthday. Many of our members knew him personally, and many more knew he was the inspiration, creator, and driving force behind the Loma Linda center, a facility that’s borne his name since 2007. Those who knew him also knew he was loath to call attention to himself; he invariably gave credit to his colleagues who helped develop the center and operate it after it opened. For Dr. Slater, the proton center was all about patients’ relief from suffering; it wasn’t about him.
Not Just Another Story
From time to time over the years, Dr. Slater was asked to tell the story of how the proton facility at Loma Linda came to be. In the early 1990s, in fact, he began working on a comprehensive history. That effort continued, on and off, for the next 15 years.
However, the book never was finished; other projects always came up, usually involving exciting research that might lead to better patient care. A colleague joked with Dr. Slater that he was too interested in the next problem to be bothered with looking back. He would laugh, but didn’t deny it. In the spring of 2014, however, Dr. Slater met with his colleague and science writer, William Preston, for a series of talks. They discussed writing about the experience of developing the proton facility. Dr. Slater didn’t want to simply rehash the history of the proton center; he’d been interviewed many times; and books, articles, and videos had resulted from those interviews. Instead, he was willing to tell the story, including some of his personal history, only if it could be something other than just another retelling.
Don’t Just Stand There is the result. Dr. Preston wrote it based on interviews with Dr. Slater in 2014 and 2015; on many papers that he and Dr. Slater had worked on for medical journals; and on numerous talks they’d had over the years. It tells something of Dr. Slater’s experiences as a child and young man; describes events in his physician training that led him to proton therapy; and offers stories about the proton synchrotron at Loma Linda and the development of what is today the James M. Slater, MD, Proton Treatment & Research Center (also known as the Loma Linda University Cancer Center or LLUCC).
A Teaching Tool
At Dr. Slater’s insistence, the book also attempts to teach. Several times during their discussions in 2014, Dr. Slater told Dr. Preston that he often wondered if some elements of the history of the long-term projects he worked on at Loma Linda might be instructive to others. The Proton Treatment & Research Center was an immense undertaking, as was developing computer-assisted treatment planning, which he began in the late 1960s. It occurred to him that some aspects of conceiving, planning, and orchestrating these large projects may apply to any number of other large projects, whether in medicine or other disciplines in life. Over the years Dr. Slater met people in all walks of life, many of whom had dealt with large and complex problems. He was struck by some of the stories they told about their work: although the fields or disciplines usually had nothing to do with medicine, many experiences were similar. Often these common experiences involved solving great problems and accomplishing something for the common good. Many of these experiences involved working with other people.
The Great Problem
The great problem Dr. Slater wanted to solve as a radiation oncologist was the suffering that cancer patients experienced, not only from the disease but also from its treatment. When Dr. Slater began practicing radiation therapy in the mid-1960s, the latter was a significant concern. He was appalled and distressed at the side effects that radiation therapy could cause, effects that were sometimes so severe that treatments had to be suspended for a time, thus compromising the physician’s ability to treat the cancer successfully. He realized that the core reason for these side effects was exposure of too much normal tissue during radiation treatments. He was not willing to accept that this need be so; he thought there had to be better ways.
Dr. Slater’s solutions - precision radiotherapy planning and proton radiation therapy - alleviated both problems. In this way, and working with others, he contributed to the common good.
Big Problem Solving
Although the book includes some elements of Dr. Slater’s story at Loma Linda, it’s not the comprehensive history that Dr. Slater once started to write. However, it places that story in the context of problem solving, especially big problems that require preparation, commitment, will, energy, and persistence. Dr. Slater viewed his efforts in developing a computer-assisted therapy planning system and the world’s first hospital-based proton treatment center as examples of what others have done to solve other problems in medicine and in other disciplines or endeavors. He thus hoped that his work, as told in this book, would help others who contend with large problems. Dr. Slater believed there’s a common core that applies to great endeavors everywhere. Therefore, this book attempts to place his life and work in a larger context, which he hoped the reader will find informative and, perhaps, inspiring.
Although Dr. Preston is the author of the book, he insists the story is Dr. Slater’s, told as Dr. Slater wished.
Don’t Just Stand There?
The title, Don’t Just Stand There, arose out of one of the conversations Dr. Slater and Dr. Preston had in 2014. Dr. Preston asked Dr. Slater to relate some of his experiences as a young man working in logging and mining camps in Utah. In those camps, Dr. Slater said men valued each other for what they could do and how well they could do it. There was much to be done: trees had to be felled; stumps had to be pulled; logs had to be cleared; stones had to be removed from the roads; tunnels and hillsides had to be blasted. Work had to get done, and everyone was expected to play his part without supervision. As Dr. Slater said, “If there’s a job to do, you don’t just stand there, you do it!”
Dr. Preston thought those words fit the work Dr. Slater had accomplished at Loma Linda. When confronted with the problem of improving radiation therapy in ways that would reduce side effects and suffering, he did something about it. He kept at it for more than 20 years before the proton center opened at Loma Linda, and he continued to keep at it for the rest of his life. Figuratively … he didn’t just stand there.
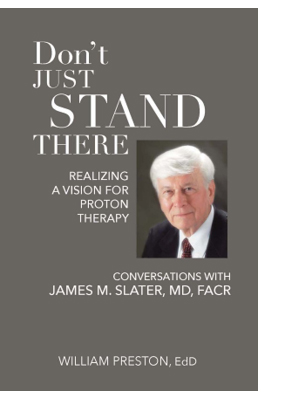 Pre-published Book Available to BOB Members
Pre-published Book Available to BOB Members
It will probably be several months to a year or more before the book is published and available for sale to the general public. But here’s the good news: We managed to get our hands on a bunch of copies of the completed book. It will likely be offered, when published, for around $30.00. We’re hoping to raise funds for proton research by offering a copy of the book to anyone who makes a contribution to proton research at Loma Linda for $100 or more.
If you’d like to have a copy of this awesome book, please send a check for $100 or more, payable to “Loma Linda University Proton Cancer Research” and mail it to:
Loma Linda University Health • Office of Philanthropy • PO Box 2000 • Loma Linda, CA 92354
Please notify Deb Hickey at [email protected] that you’ve sent in your check and she’ll mail you a book.
We’re sure you’ll thoroughly enjoy the book and we know it will occupy a place of honor in your home. And, you’ll be helping to fund basic and clinical proton research on prostate cancer, pancreatic cancer, liver cancer, breast cancer, and much more with your tax-deductible gift.
Thank you!

New Imaging Technique a “Game Changer”
Source: University of California, San Francisco
Full body PET/CT scans have been used for years to detect cancerous lesions in humans. They’re commonly used to find metastatic cancer sites following a cancer recurrence from months to years after treatment. We’ve written about several of these tests in previous newsletters. These PET/CT scans include C-ll Choline, C-11 Acetate and most commonly used, fluciclovine PET (also called the Axumin scan) among others.
The New Standard-of-Care?
One new test that has shown considerable promise is Gallium-68 prostate-specific membrane antigen imaging – or the Ga-68 PSMA PET/CT scan. This test uses a highly sensitive drug that is extremely effective in detecting prostate cancer throughout the body. It’s so effective, it often identifies cancer that is missed by current standard-of-care imaging techniques. Researchers are reporting that the Ga-68 PSMA scan is so precise, it should become the new standard-of-care for initial prostate cancer staging as well as evaluation of patients with recurrent cancer.
Tracer Helps Pinpoint Lesions
Recently, the FDA approved the use of Gallium-68 for PSMA PET/CT scanning as a result of research conducted at UCSF and UCLA. Ga-68 is a radioactive tracer that’s injected into the body. The tracer attaches to prostate-specific membrane antigen proteins helping physicians pinpoint the location of the cancerous lesions.
PSMA PET vs. Axumin Scan
When comparing Ga-68 PSMA PET/CT scan to the most commonly used Axumin scan, researchers found the PSMA PET was able to detect significantly more prostate cancer lesions than the Axumin in men with recurrent cancer.
UCLA and UCSF researchers are strongly recommending this new test be used on men with high-risk cancers as part of their initial staging as well as men with recurrent cancer after surgery or radiation.
Who Offers PSMA CT/PET?
UCLA and UCSF are the only medical centers in the U.S. offering PSMA CT/PET imaging through FDA approval. Other medical centers have applied for expedited FDA approval and are expected to adopt this new technology when the approval is granted. In the meantime, a few centers are conducting clinical trials using Ga-68 PSMA PET/CT imaging technology.
“‘Game changer’ is almost an understatement for how prostate cancer patient care could be improved by this technique,” said Jonathan Simons, MD, CEO of the Prostate Cancer Foundation, which has invested more than $26 million in PSMA research over the past few years. Dr. Simons considers the UCLA/UCSF PSMA results a “milestone achievement.”
Possible Breakthrough in Treating Oligometastatic Disease
In the past, metastatic prostate cancer was considered essentially incurable and was routinely treated systemically (hormones, chemo, other drugs), with the intent of slowing disease progression.
Because of improvements in imaging techniques, physicians have recently begun treating some metastasis (usually fewer than five lesions, called “oligometastasis”) with curative intent using focal therapies. The Ga-68 PSMA development adds even more importance to an imaging test that can accurately detect metastatic lesions throughout the body.
No doubt we’ll be hearing much more about Ga-68 PSMA PET/CT scanning in the near future.
Learn more at NYTimes.com and Cancer.gov.
 FDA Approves New Oral Hormone Therapy Drug for Prostate Cancer
FDA Approves New Oral Hormone Therapy Drug for Prostate Cancer
The FDA recently approved Orgovyx (relugolix), an oral androgen deprivation therapy (ADT) drug, for men with advanced prostate cancer.
“[The] approval marks the first oral drug in its class and it may eliminate some patients’ need to visit the clinic for treatments that require administration by a health care provider,” said Richard Pazdur, M.D., director of the FDA’s Oncology Center of Excellence. “This potential to reduce clinic visits can be especially beneficial in helping patients with cancer stay home and avoid exposure during the coronavirus pandemic.”
Orgovyx is a once-daily tablet that works by rapidly suppressing testosterone. It’s also been associated with a 54 percent lower risk of major adverse cardiovascular events compared with Lupron (leuprolide).
Medicare’s New Rule and Its Impact on Proton Therapy
In September 2019, the Center for Medicare and Medicaid Innovation (CMMI) proposed a new payment model for radiation oncology services. If approved, the mandatory model for those on Medicare would result in health systems receiving reimbursement for proton therapy at the same national base rate as all other radiation modalities (including IMRT and brachytherapy). To be clear, Medicare would no longer cover proton therapy as it had in the past. Rather, it would cover the same amount for proton as it does for any other radiation treatment, reducing coverage levels significantly.
In November 2020, the Radiation Oncology Alternative Payment Model (RO APM) Final Rule was released, and unfortunately, it wasn’t what we expected or wanted.
The Final Rule
The new RO APM rule shifts payment for radiation oncology reimbursement from a fee-for-service model (the most traditional healthcare payment model where providers are paid for each service) to a value-based bundled payment (covers all the care a patient receives during treatment for a specific illness, condition, or medical event).
Particpation is mandatory for 30 percent (12) of proton centers selected randomly by zip code. This means proton therapy at these facilities will be paid by Medicare at the same rate as other radiation treatment modalities, most of which are much less expensive.
The rule will be tested for five years and then reassessed.
CMS’ Reasoning
According to the Centers for Medicare & Medicaid Services (CMS), the RO APM Model was created to “promote quality and financial accountability” for providers and suppliers of radiotherapy services. With the final model design, CMS is seeking to test whether making prospective episode payments to hospital outpatient departments, freestanding radiation therapy centers, and physician group practices for radiation therapy episodes of care preserves or enhances the quality of care furnished to Medicare beneficiaries while reducing Medicare program spending through enhanced financial accountability for RO APM Model participants.
► BOB Comment: We’re not sure how this model creates quality. Rather, it seems it’s a way for Medicare to save money. In fact, CMS estimates the expected savings are $230 million.
Timing
The new model was set to go into effect on Jan. 1, 2021. However, the National Association for Proton Therapy (NAPT), along with the American Society for Radiation Oncology (ASTRO) and other major stakeholders, urged CMS and Congress to delay the start date and make reforms to alleviate the reduction in reimbursement to our health systems caring for cancer patients. Furthermore, the timeline proved untenable for cancer centers in the midst of managing essential care for vulnerable patients during the coronavirus pandemic.
Fortunately, CMS agreed to a six month delay. Shortly thereafter, Congress pushed the date even further – from July 2021 to January of the following year. This means the new model can’t be implemented before 2022; it doesn’t necessarily mean it will be carried out in January. In fact, impementation could be delayed further. This is good news for those in the proton community as it gives stakeholders more time to understand the details and advocate for regulations that ensure greater access to proton therapy.
Fallout for Participants
The implications for the practices chosen to participate in the RO APM Model are alarming, especially considering the economic distress already caused by COVID-19. According to ASTRO, the pandemic has resulted in a 20 to 30 percent reduction in revenue for the average radiation oncology practice and has even forced layoffs. Implementation of the new model will also cause issues beyond a considerable reduction in reimbursement. Participants will likely need a new technology infrastructure for coding and billing procedures. And costs for adapting these and other requirements could be significant.
“Financially, the RO Model will bring more pain to practices,” said Dave Adler, vice president of advocacy at the American Society for Radiation Oncology (ASTRO). “According to the final rule, the RO Model will cut payments to group practices by 6% and hospital outpatient departments by 4.7%. Amazingly, these cuts are deeper than what CMS estimated in its proposed rule.”
Adler also says the rule fails to consider the many good faith recommendations that were provided to CMS by ASTRO, NAPT, radiation oncology stakeholders, patients, and Congress. These groups devoted an unprecedented amount of time and effort to engage with CMMI to help develop a payment model that would consider savings and quality improvements while providing stable payments to sustain physician practices.
Impact on Proton Therapy
Over the next year, proton therapy stakeholders will work together with congressional leaders to assess the impact the RO APM Model will have on the proton community. They will also make the case that the flawed model jeopardizes patient access to proton therapy by potentially limiting the development of new facilities and placing existing proton centers in a financially fragile position. Furthermore, the model threatens research and innovation as well as emerging technologies that require large capital and operating investments.
Stay tuned and stand ready for another possible email or letter-writing campaign to CMS or Congressional leaders.
► BOB Comment: It’s important for readers to understand the RO APM Model will not affect patient care. Patients will receive the same quality care whether they’re treated at a participating practice or not.



We’ve been producing BOB Tales newsletters monthly for 20 years. During this time there have been articles that many new members haven’t seen, and some older stories members may have forgotten. So, we periodically re-run articles from past newsletters. Following are excerpts from an article, written by Bob Marckini, in our February 2011 newsletter – exactly 10 years ago – detailing Dr. Lynn Martell (Former D.Min. Executive Director of Special Services at Loma Linda University Cancer Center) and his wife Karen’s annual Christmas dinners.
Loma Linda Director Invites 65 Patients Home for Christmas Dinner
A little more than 10 years ago, while I was in treatment at Loma Linda, Dr. J. Lynn Martell stood up at a LLUCC Wednesday night meeting in mid-December and asked the group, “How many of you will be here during the Christmas Holidays?” A bunch of hands went up. Next, he said, “No one should spend Christmas in a lonely apartment. I’d like to invite you all to come to my home and have Christmas dinner with me and my family.” About 65 people accepted Lynn’s invitation and spent Christmas with the Martell family.
I didn’t learn until later that Lynn’s invitation that night was spontaneous. He hadn’t discussed it with his wife, Karen (or “Saint” Karen as I often refer to her). That was the beginning of a tradition that’s lasted to this day.
This past December, the Martells opened their home, for the 11th Christmas, to proton patients who were away from home. Seventy accepted their invitation.
.jpg) A good time was had by all. Lynn and Karen’s family helped to prepare their home, move furniture, decorate the house and serve guests.
A good time was had by all. Lynn and Karen’s family helped to prepare their home, move furniture, decorate the house and serve guests.
Note: When the Martells eventually ran out of room, some patients had to eat in the bathroom. This is just one more excellent example of how LLUCC’s “Make Man Whole” mission works.
Where are they now?
Dr. J. Lynn Martell has had a huge impact on us from the very beginning. When Lynn was at Loma Linda University Health, he recognized the value and potential for the Brotherhood of the Balloon long before we did, and he did everything possible to encourage and support our growth. We wouldn’t be an organization today ─ with 10,000 members in 39 countries, helping people learn about proton therapy and raising millions of dollars for proton research and other worthy causes ─ if it hadn’t been for Lynn’s steadfast support and encouragement over the years.
Bob and Deb stay in touch with Lynn and his wife, Karen. Lynn pastors the Los Alamitos SDA Church in Cypress, CA, with Karen as the prayer team leader. Both have had their health challenges, and both are doing well today we’re happy to report.
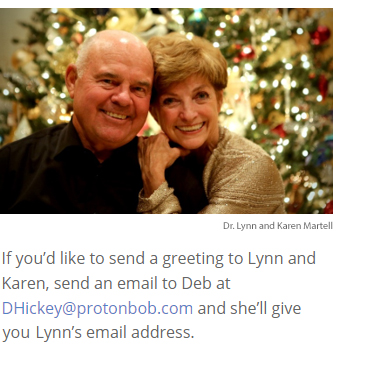 Karen and Lynn recently posed for a Christmas photo, which we’d like to share with you. They’re warm and friendly smiles haven’t changed in 20 years. Last month Lynn celebrated his 80th birthday. He’s quite active; he’s enjoying life; and he regularly reminds us that, “God is good!” And we agree.
Karen and Lynn recently posed for a Christmas photo, which we’d like to share with you. They’re warm and friendly smiles haven’t changed in 20 years. Last month Lynn celebrated his 80th birthday. He’s quite active; he’s enjoying life; and he regularly reminds us that, “God is good!” And we agree.
Member Feedback
We receive tons of emails from BOB members, especially around the holidays. Member Ted Smathers of Golden, CO sent a Christmas greeting to Bob. Following is an excerpt:
Fifteen years ago I drove from Loma Linda to Golden, CO having completed my proton treatment at LLUCC and it seems like yesterday. You and I can both rejoice for Loma Linda, proton therapy, and the health we have.
Please say “hello” to Deb. The BOB newsletter is an outstanding product and so well put together. I always look forward to the publication.
Let’s have a great 2021 and put 2020 in the rearview mirror.
Amen to that!
Here’s a message Deb received from BOB member Stuart Cooper of Roslyn Heights, NY, in response to the opening memo in our last newsletter:
Congratulations on twenty years cancer-free to Bob! For me it’s almost 16 years. I was 51 in February 2005 and I was urged by my doctor to have surgery. I was just about set to confirm the procedure when I learned about proton therapy and Loma Linda. I did my due diligence and realized I had the best chance of cure and quality of life with proton radiation. I moved from New York to California for eight weeks, and it was the best decision of my life. Today, my PSA is low and my quality of life 100 percent.
Thank you, Bob, for your wise advice and counsel at that time and thank you, Deb, for your activism and dedication.
Here’s another response to Deb’s memo written by BOB member John W. Harrison, Col. USAF Retired:
What a great story and so well written!
I underwent proton therapy for prostate cancer at age 78 in 2001 at Loma Linda. The fact that I’m still here is proof of the life-saving treatment!
As an old, retired fighter pilot, I’ve faced many challenges in my lifetime, including over 400 missions in Vietnam. I thought my advanced prostate cancer diagnosis would be my final challenge. Then, a fellow airman told me of his bout with prostate cancer and his superb treatment with proton therapy at Loma Linda University Cancer Center. I immediately set up a consult and was shortly approved for treatment. It was the smartest medical decision I’ve ever made. Everyone ─ from the doctors down to the medical technicians were so dedicated and professional I knew the treatment was going to be successful.
I’ll be forever grateful.
We got lots of feedback on Deb’s opening memo! Here’s another message sent by BOB member Jim Bodino of Grandy, NC:
That was such a heartfelt letter from an adoring, loving, and thankful daughter. Your father deserves your tribute since he’s been the engine and driving force in the fight against prostate cancer, both curable and preventive.
You should also take a bow for the contributions you’ve made to me and countless others in the “proton family.” Believe me, your dedication and information are much appreciated.
Here’s a message sent by BOB member Moss Gropen of San Diego, CA:
It was March, 2014, and I was just diagnosed with prostate cancer as a lad of 56. After doing some research, I told my wife I’d be driving from our house to the just-built Scripps, about six miles away, for proton treatment every day for a while.
Fast forward, and I’m a balloon guy. And, believe it or not, my memories of cancer treatment are actually pleasant. Thanks to this great technology and the brilliant, kind staff at Scripps*, when others ask about my prostate cancer, I say… “Ain’t no thang!” I also think, “Thank God ... and save your prayers for those who really need them...”
Moss wrote in a follow-up email:
Please feel free to pass along my name and email address to any guy who’s gotten the bad news and could use some uplifting views on this copacetic approach to treatment. Having the option of an effective treatment with minimal side effects is a real “game changer” because, for the newly-diagnosed and others, it knocks down the fear factor. And when you cut down on fear, you pile on hope.
We think our members are really great. It must be the protons …
*California Protons Cancer Therapy Center


 You Can Beat Prostate Cancer: And You Don’t Need Surgery to Do It – Second Edition
You Can Beat Prostate Cancer: And You Don’t Need Surgery to Do It – Second Edition
Bob’s book continues to gain momentum as emails from readers attest. It still sits in the No. 1 position on an Amazon search for books on “prostate cancer,” where it’s one of more than 4,000 books on the subject. The book has 57 five-star reviews; here’s what one reader posted last month:

Do your own research even though Bob Marckini did it for you, and thoroughly: Bob’s book is a thorough, in-depth look into the treatments and therapies for prostate cancer and highlights proton radiation therapy. It’s an easy read and not too technical. When it does get technical, Bob does a great job breaking it down into understandable language. I devoured this book; laughed out loud and welled up on numerous occasions. If you’ve heard the words, “you have prostate cancer,” READ THIS BOOK!
Several proton centers have been sending out Bob’s book when patients make inquiries. The book is always favorably received and heavily influences the patient’s treatment decision. How do we know this? They tell us.
Did you find Bob’s new book valuable? Please write a review on Amazon.
Reminders
We’re happy to discount books in quantity (minimum 20) to anyone interested in spreading the word on proton therapy. Just send an email to [email protected]. Proceeds from book sales are used to help fund our efforts and to support proton therapy research.
The Kindle version is free to Kindle Unlimited members or can be purchased for $9.99 for non-members. The paperback price is $22.45
Buy You Can Beat Prostate Cancer second edition on Amazon or Lulu Press.


Our Generous Members
Many of our members have made gifts to the Robert J. Marckini Endowed Chair for Proton Therapy Research at Loma Linda. Gifts range from a few dollars to tens of thousands, and in a couple of cases, more than a million dollars. Some have given once; many give annually, and some give monthly through automatic bank transfers. Several who’ve made gifts weren’t even treated at Loma Linda, but they appreciate the role they played in their ability to have proton therapy. This warms our hearts. It sends a strong message that members appreciate the pioneering work that Dr. James Slater, Dr. Jerry Slater, and the team did to make proton therapy available to cancer patients. It also tells us you appreciate the work we do keeping our 10,000 members in 39 countries together and informed about the latest developments in prostate cancer prevention, diagnosis, treatment in general, and proton therapy in particular, as well as some of the peripheral topics we cover in our newsletter.
And remember, if you make a contribution to proton research at Loma Linda for $100 or more, you can get a free copy of Don’t Just Stand There – Realizing a Vision for Proton Therapy mentioned in the opening memo. Just send a check, payable to “Loma Linda University Proton Cancer Research,” and mail it to:
Office of Philanthropy
Loma Linda University Health
PO Box 2000
Loma Linda, CA 92354
*Notify Deb Hickey at [email protected] that you’ve sent in your check and she’ll mail you a book while they last.
More Ways to Give Back
- Donate to proton research online.
- Write a check to LLUCC Proton (Put “Marckini Chair” on the memo line) and mail to LLUH, Office of Philanthropy P.O. Box 2000, Loma Linda, CA 92354.
- Make an unrestricted gift (put “unrestricted” on memo line) so LLUH can use it where it’s needed most.
- Call Regina Joseph at 909-558-5010 to donate over the
- phone and/or to inquire about naming opportunities.

Exercise, Diet Can Improve Bone Health for Prostate Cancer Patients
All men lose bone mass or density as they age, but the risk is compounded for those who’ve been diagnosed with prostate cancer.
How can prostate cancer affect bones?
Men may experience bone-related problems as a result of prostate cancer or its treatment. In advanced prostate cancer, the most common site of metastases (spread outside the prostate) is to the bones, potentially causing pain. Men who are treated with hormone therapy for prostate cancer may experience bone loss, fracture, or joint pain. Androgen deprivation therapy (ADT) works by blocking the production of testosterone, which plays a critical role in keeping bones strong. Patients on hormone therapy may also take longer to recover from a bone fracture than other men.
How to Improve Bone Health
 Patients can strengthen and maintain bone density by participating in weight-bearing, aerobic and resistance exercises such as brisk walking, swimming, climbing stairs, hiking, jumping rope, or even step aerobics. Exercise has been proven to have positive impacts on quality of life, fatigue, lean muscle mass, muscle strength, physical function, and balance. However, it’s important to note that no single exercise plan works best for everyone. And consult with your doctor before starting any exercise program.
Patients can strengthen and maintain bone density by participating in weight-bearing, aerobic and resistance exercises such as brisk walking, swimming, climbing stairs, hiking, jumping rope, or even step aerobics. Exercise has been proven to have positive impacts on quality of life, fatigue, lean muscle mass, muscle strength, physical function, and balance. However, it’s important to note that no single exercise plan works best for everyone. And consult with your doctor before starting any exercise program.
Getting the proper nutrients can also improve bone health. Men on ADT should be sure to get enough calcium and vitamin D – preferably together, as vitamin D (which may improve muscle strength and function) helps the body absorb calcium and phosphorous (which are good for bone health). Data have shown that a daily dose of vitamin D (800 IU) reduced hip fractures for people aged 65 or older.
► BOB Comment: It appears that those with prostate cancer in their families should pay attention to their vitamin D levels. A blood test that measures 25-hydroxyvitamin D can give you important information about vitamin D levels in your body.
Dr. Charles “Snuffy” Myers, noted prostate cancer expert (retired), often recommended his patients take vitamin D3 supplements.
While vitamin supplements can be beneficial, eating whole foods ─ such as fresh fruits and vegetables, whole-grains, healthful sources of protein (such as fish, eggs, and beans), and healthful fats (like olive oils, nuts, and avocados) ─ is also important. Patients should avoid sugar-sweetened drinks and excess salt as well.
Patients should also not smoke or drink alcohol in excess as both can contribute to poor bone health.
The Truth About Brain Supplements
Keith Roach, M.D. Weill Cornell Medicine, has a syndicated newspaper column, To Your Good Health. In a recent article, an 84-year-old gentleman with failing memory asked about the advisability of taking brain supplements advertised in the media. Following is part of Dr. Roach’s response:
A careful review of the published data (where there is any) reveals no consistent evidence that supplements are effective in the treatment or progression of Alzheimer’s disease. There may be one exception: vitamin E*. Patients who want to try that in reasonable doses (consult with your physician on this) may have a modest benefit. These benefits are likely to be smaller than with the approved prescription treatments for Alzheimer’s disease, and even those are fairly small in most cases.
Regular moderate exercise; a mostly plant-based diet high in fruits, vegetables, and legumes and with moderate fish and low meat; and cognitive exercises are all much more likely to show benefit than any medication or supplement. Conditions that can adversely affect brain health, especially poorly controlled diabetes, and blood pressure, should be aggressively treated.
*Be careful. A study reported in the Journal of the American Medical Association (JAMA) in 2011 reported that, “Dietary supplementation with vitamin E significantly increases the risk of prostate cancer in healthy men.”

National Proton Conference: April 2021
 The National Association for Proton Therapy (NAPT) is the voice of the proton therapy community ─ providing education and awareness for the public, professional, and governmental stakeholders about the benefits of proton therapy for treating cancer.
The National Association for Proton Therapy (NAPT) is the voice of the proton therapy community ─ providing education and awareness for the public, professional, and governmental stakeholders about the benefits of proton therapy for treating cancer.
Join NAPT for the ninth annual National Proton Conference, April 15 & 16, 2021. NAPT will bring together the community in a virtual format that builds on the success of their 2020 virtual education opportunities with the addition of new opportunities and features.
This year NAPT continues their mission to educate and increase awareness about the clinical benefits of proton therapy, ensure patients' choice and access, and to encourage cooperative research and innovation. NAPT is committed to move the proton industry forward and look forward. The proton community has united through the opportunities these challenging times have presented and their continued goal is to connect the brightest minds and visionaries in the field to advance the future of proton therapy ─ a future shaped by collaboration to initiate, illuminate, and innovate.
Topics Will Include …
- Latest research on proton therapy
- Proton therapy insurance coverage and reimbursement
- Flash Therapy
- Developing and incorporating particle therapy into a cancer program
- Updates on key health policies impacting cancer care
- Marketing and Public Relations
- Trends in particle therapy for the future
- Ensuring value in alternative payment models
- Best practices for clinical and business operations



 How Dogs Are Sniffing Out COVID-19, Cancer, and More …
How Dogs Are Sniffing Out COVID-19, Cancer, and More …
Dogs are known for their keen sense of smell. In fact, dogs have smell receptors 10,000 times more sensitive than humans’. Dogs can sniff in parts per trillion, which is three orders of magnitude more sensitive than today’s available instruments. According to a study published in Frontiers in Veterinary Science, “a dog could detect the equivalent of one drop of a liquid in 20 Olympic-size swimming pools. Their powerful sensory system allows dogs to detect diseases, pathogens, cadavers, lost/criminal persons, and other biological targets…”
As people become sick, their body chemistry changes. Depending on the disease, dogs are able to detect these changes and alert doctors to illnesses before they even begin to affect the body.
A new study has found, “canines have a 76 percent to 100 percent accuracy rate at detecting individuals with the coronavirus simply by smelling their sweat samples.” Around the world, trainers are working with dogs to detect COVID-19 in humans and they’re reporting extraordinary results. Though findings haven’t been peer reviewed or published, scientists speculate that canines could help control the pandemic because they can screen hundreds of people in under an hour, which is much less expensive than traditional testing methods.
Dogs’ olfactory abilities have fascinated scientists for decades. In 2006, a study showed that dogs were able to detect breast cancer in women with 90 percent accuracy. A 2015 study revealed dogs were able to sniff out prostate cancer via urine samples with 93 percent accuracy. In fact, dogs have been taught to detect cervical, colorectal, lung, stomach, liver, ovarian, and thyroid cancers in many cases far sooner than laboratory tests ever could.
So, should we stop mammograms, pap smears, and PSA tests for a visit to the labrador retriever? Not quite, though scientists are working with canines to determine a specific cancer “scent” that can be detected by computer. And some day, our personal tech devices may be able to alert us to changes in our normal body odor that could signal disease, but until then we should continue to visit our doctors.
 If There Were Only 100 People on Earth …
If There Were Only 100 People on Earth …
What would the world look like if there were only 100 people on earth? Journalist Eye did an interesting story on this subject a few months ago. It was titled, Amongst 100 Persons in the World, Only Eight Can Live or Exceed the Age of 65. They pointed out there are more than seven billion people on earth. Then they asked the question, “What would the world look like if someone produced a statistical report condensing the seven billion people to only 100?” It would look something like this:
.jpg)
They conclude with this: “If you have your own home; eat full meals and drink clean water; have a mobile phone; can surf the Internet; and have gone to college, you have little reason to complain. Amongst 100 persons in the world, only eight can live or exceed the age of 65. If you’re over 65 years old be content and grateful. Cherish life. Grasp the moment. You didn’t leave this world before the age of 64 years like the 92 persons who’ve gone before you. You are already the blessed amongst mankind.”



Last Month’s Brain Teaser
What nine-letter word remains a valid word as each of its letters is successively removed?
Answer: STARTLING
Remove the L, and the word becomes: STARTING
Remove one T, and the word becomes: STARING
Remove the A, and the word becomes: STRING
Remove the R, and the word becomes: STING
Remove the other T, and the word becomes: SING
Remove the G, and the word becomes: SIN
Remove the S, and the word becomes: IN
Remove the N, and the word becomes: I
Winner: Jim Devine of Marriottsville, MD
In an email to Deb, Jim wrote:
Thank you! God bless you – and your dad – in your noble and compassionate work. I’m an 82-year-old, six-year survivor of prostate cancer thanks to him, proton therapy, and Loma Linda. I still play golf (badly) and walk for exercise most days. I also enjoy every day with my loving wife.
Congratulations, Jim! Your signed copy of Bob’s book is in the mail.
New Brain Teaser
B, E, J, Q, X, Y AND Z are the only letters in the alphabet not included among the first letters of a certain group of names. What is the name of the group?
Don’t give up too quickly ─ it may be easier than you think! Send your brain teaser answer to [email protected] for a chance to win a signed copy of Bob Marckini’s NEW second edition book, You Can Beat Prostate Cancer.
A Wise Man Once Said …
Many women like to marry military men ─ they can cook, sew, and make beds. And, they’re in good health and already used to taking orders.
Eventually you reach a point when you stop lying about your age and start bragging about it.
Some people try to turn back their odometers. Not me, I want people to know why I look this way: I’ve traveled a long way and some of the roads weren’t paved.
You know you are getting old when everything either dries up or leaks.
Old age is when former classmates are so gray, wrinkled and bald, they don't recognize you.
Long ago when men cursed and beat the ground with sticks, it was called witchcraft. Today it’s called golf.
Walmart Greeter
Young people forget that we old people had a career before we retired …
Charley, a new retiree-greeter at Walmart, just couldn’t get to work on time. Every day he was 10-15 minutes late. But he was a good worker. He was tidy, sharp-minded, and a real credit to the company and obviously demonstrating their “Older Person Friendly” policies.
One day the boss called him into the office for a talk. “Charley, I like your work ethic. You do a bang-up job when you finally get here; but your tardiness is quite bothersome.”
“Yes, I know, boss. I’m sorry. I’ll work on it.”
“Well, good! You’re a team player – that’s what I like to hear.”
“Yes sir. I understand your concern and I will try harder.”
Seeming puzzled, the manager went on to say, “I know you’re retired from the armed forces, Charley. What did they say to you if you showed up late so often?”
The old man looked down at the floor, then smiled and said with a grin, “They usually saluted and said, ‘Good morning, Admiral, can I get your coffee, sir?’”
Reflecting on 2020 …
The dumbest thing I bought last year was a planner.
I was so bored recently, I called Jake from State Farm just to talk to someone.
2019: Stay away from negative people. 2020: Stay away from positive people.
The world has turned upside down. Old folks are sneaking out of the house and their kids are yelling at them to stay home.
This morning I saw a neighbor talking to her dog. It was obvious she thought her dog understood her. I came into my house and told my cat. We laughed a lot.
Every few days, try your jeans on to make sure they fit. Pajamas will have you believe all is well in the kingdom.
Does anyone know if we can take showers yet or should we just keep washing our hands?
I hope the weather is good tomorrow for my trip to the backyard.
Never in a million years could I have imagined I’d go up to a bank teller wearing a mask and ask for money.

Quote of the Month: “Money can’t buy happiness, but somehow it’s more comfortable to cry in a Mercedes than in a Yugo.” —Unknown




I Will Live Forever
Bob Marckini lost a good friend, Dave, a few months ago. At his memorial service, Dave’s wife showed Bob something Dave had carried in his wallet for more than 40 years. It was yellowed and creased and torn in several places, but the message was as fresh as could be. It was an essay by Robert Test, titled, I Will Live Forever.
The day will come when my body will lie upon a white sheet neatly tucked under four corners of a mattress located in a hospital; busily occupied with the living and the dying. At a certain moment a doctor will determine that my brain has ceased to function and that, for all intents and purposes, my life has stopped. When that happens, do not attempt to instill artificial life into my body by the use of a machine, and don’t call this my deathbed. Let it be called the bed of life, and let my body be taken from it to help others lead fuller lives.
Give my sight to the man who has never seen a sunrise, a baby’s face or love in the eyes of a woman.
Give my heart to a person whose own heart has caused nothing but endless days of pain.
Give my blood to the teenager who was pulled from the wreckage of his car, so that he might live to see his grandchildren play.
Give my kidneys to the one who depends on a machine to exist from week to week.
Take my bones, every muscle, every fiber and nerve in my body and find a way to make a crippled child walk.
Explore every corner of my brain. Take my cells, if necessary, and let them grow so that, someday a speechless boy will shout at the crack of a bat, and a deaf girl will hear the sound of rain against her window.
Burn what is left of me and scatter the ashes to the winds to help the flowers grow.
If you must bury something, let it be my faults, my weaknesses, and all prejudice against my fellow man.
Give my sins to the devil. Give my soul to God.
If by chance, you wish to remember me, do it with a kind deed or word to someone who needs you. If you do all I have asked, I will live forever.
Bob Marckini and Deb Hickey
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
NO MEDICAL ADVICE: Material appearing here represents opinions offered by non-medically-trained laypersons. Comments shown here should NEVER be interpreted as specific medical advice and must be used only as background information when consulting with a qualified medical professional.