Dear Members (a note from Deb Hickey):
For the first time ever, I sat down and wrote a recap of the National Proton Conference within a week of attending. Typically we include a paragraph or two about the event in the May issue opening memo, and then spend a month sifting through notes and photos in an effort to include a comprehensive recap in the June issue, but I was so triggered by the material presented this year, I couldn’t stop myself from writing. Additionally, Bob Marckini attended the COMPPARE Activation Workshop the week before I headed to Miami for the proton conference. Consequently, we both wanted to report on important details from these events which resulted in a much longer newsletter than usual—thus, a double issue was conceived. And be forewarned, my review is quite extensive. You may want to visit the bathroom, grab a cup of tea, and park yourself on the sofa.
 In my opinion, the speakers and attendees at this year’s National Proton Conference were more passionate about proton therapy than ever before. The presentations and discussions were energetic, informative, and even emotional at times. The most talked about topics were health insurance reimbursement (not surprising), advancements in proton therapy technology, ongoing and upcoming clinical trials, and the importance of collaboration in an effort to fight for easier access to proton therapy. I discuss these issues in detail in this issue. But before I do, I wanted to write about one presentation that left the audience (even the camera man) in tears.
In my opinion, the speakers and attendees at this year’s National Proton Conference were more passionate about proton therapy than ever before. The presentations and discussions were energetic, informative, and even emotional at times. The most talked about topics were health insurance reimbursement (not surprising), advancements in proton therapy technology, ongoing and upcoming clinical trials, and the importance of collaboration in an effort to fight for easier access to proton therapy. I discuss these issues in detail in this issue. But before I do, I wanted to write about one presentation that left the audience (even the camera man) in tears.
When Raymond Rodriguez-Torres took the stage to talk about the Live like Bella Foundation, I already knew it was going to be emotional; his title slide included a large logo with the name of the foundation in child’s handwriting with the words, “End Childhood Cancer” beneath it. And then Mr. Rodriguez-Torres began to talk about his daughter.
Bella was born in December 2002 and although she had some developmental delays from low oxygen at birth, she was healthy and happy. Five years later, the bubbly little girl had an unexpected seizure and was diagnosed with stage four alveolar rhabdomyosarcoma.
Shortly thereafter, Bella became paralyzed from the waist down and was told by doctors she’d never walk again and had only weeks to months to live. At first, Rodriguez-Torres felt depleted, like he couldn’t do anything, but with the help of a friend, and eventually an entire community, he was able to pick himself up and move forward.
 Someone gifted the Rodriguez-Torres family with a website; worldwide prayer teleconferences began; Raymond penned a book, Why Not Me?: A True Story About a Miracle in Miami; the family organized charity events and raised thousands for pediatric cancer research; and Bella’s fight was even recognized by celebrities.
Someone gifted the Rodriguez-Torres family with a website; worldwide prayer teleconferences began; Raymond penned a book, Why Not Me?: A True Story About a Miracle in Miami; the family organized charity events and raised thousands for pediatric cancer research; and Bella’s fight was even recognized by celebrities.
During this time, Bella was one of the first children in South Florida to receive proton therapy in 2007. She conquered paralysis and started walking again. At one point, she was cancer-free for two years. Her treatment, along with the unconditional love and support of family and friends and prayers from around the world, allowed Bella to live six more years.
Bella passed away on May 28, 2013. “She was 3-foot-9, bald, but packed quite a punch,” Rodriguez-Torres said. The Live Like Bella Foundation was founded in her memory the following month.
In addition to a comprehensive review of this year’s NAPT conference in Miami, this month’s BOB Tales is one of the best, in my humble opinion. There are two special news stories—1) The COMPPARE clinical trial to compare proton therapy to IMRT for treating prostate cancer has kicked off, and 2) Tennessee just passed a proton therapy law that we believe will have big implications for other states. We also cover a broad range of other important topics including the possibility of short-term ED after prostate needle biopsy; reports that the number of prostate cancer cases is decreasing worldwide, with the largest decrease in the U.S.; holding insurance companies accountable for wrongfully denying coverage; the role of stress hormones in prostate cancer health disparities, and much more. We hope you enjoy it!
Deb Hickey
As always, we welcome and appreciate your feedback on our newsletter. Just send an email to [email protected].
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
In this Issue:
- Proton vs. IMRT: COMPPARE Trial Activated
- Tennessee Passes Proton Therapy Law
- Short-term ED after Prostate Needle Biopsy
- Prostate Cancer Diagnoses, Deaths Decreasing Worldwide; Largest Decrease in U.S.
- Insurance Denied When Most Needed
- Professor Receives NIH Grant to Study the Role of Stress Hormones in Prostate Cancer Health Disparities
- National Association for Proton Therapy Conference Recap

Proton vs. IMRT: COMPPARE Trial Activated
This is big news. The clinical trial to compare proton therapy to IMRT for treating prostate cancer has been kicked off. The COMPPARE trial is funded by the Patient-Centered Outcomes Research Institute (PCORI). The project leader is the dynamic Dr. Nancy Mendenhall, medical director from the University of Florida Health Proton Therapy Institute, the sponsoring organization. Information presented here can also be found on the COMPPARE website.
Bob Marckini serves on the Executive Board and Patient Stakeholders group and Deb Hickey serves on the Caregivers-Stakeholders group. The COMPPARE team consists of the Executive Board, Co-Investigators and Researchers, Coordinating Center Staff, Patients and Caregivers Stakeholders, Minority Engagement Group, Insurance and Vendor Stakeholders, and the Advanced Technology Consortium. Participants in each of these categories can be found here.
Partner organizations supporting the COMPPARE project include 100 Black Men of America, Inc., the Prostate Health Education Network, the Brotherhood of the Balloon, and The Prostate Net.
The COMPPARE Activation Workshop was held in Amelia Island, FL from March 22 to 24. The photo below includes some of the participants in this year’s workshop. The workshop program can be found here.

Below are key points regarding the COMPPARE trial. Note: This isn’t intended to be a complete or comprehensive review of the study.
- The COMPPARE trial will run for a minimum of 60 months (five years).
- 3,000 patients will participate—1,500 proton and 1,500 IMRT.
- 45 treatment sites (proton and IMRT combined) are participating in the study. Only a few sites are approved to register patient/participants at this time, but all 45 sites are expected to be registering patients for the trial in the coming weeks.
- Age eligibility: 30 to 80
- Patients allowed to participate in this study will include those with a low-, intermediate-, or high-risk localized prostate cancer diagnosis; and no previous prostate cancer treatment (other than short-term ADT).
- Excluded from this study are patients with metastatic disease, very low-risk prostate cancer, prior prostate surgical procedure including TURP, history of invasive rectal area malignancy, active IBD, or prior pelvic radiation treatment.
This is a large prospective, controlled study comparing patient results including disease-free survival as well as quality of life (QOL) issues and toxicity (side effects) between parallel groups of men with prostate cancer treated simultaneously at proton therapy facilities and IMRT facilities in the U.S.
The proton group will be further split into two groups. One group will receive standard proton therapy and the other will receive moderately hypofractionated treatment (higher doses, fewer treatments).
Additionally, there will be analysis of a variety of treatment related issues, including a comparison by race (black vs. white), age (65 and under vs. over 65), and prostate cancer aggressiveness for all endpoints. Participants are being asked to complete pretreatment surveys and will respond to periodic surveys after treatment ends. Some of the specific outcome measures will include bowel, urinary and sexual function.
 An important point to mention here is that patients will choose the treatment they want, i.e. proton or IMRT. If a patient decides to participate in the study, his treatment plan won’t change, and all of his treatments will be “standard of care.” By participating in the trial, the patient is agreeing to complete surveys periodically, which will help researchers determine if there are differences between proton therapy and IMRT. The results of this study will be of significant value in helping future patients with their treatment decisions.
An important point to mention here is that patients will choose the treatment they want, i.e. proton or IMRT. If a patient decides to participate in the study, his treatment plan won’t change, and all of his treatments will be “standard of care.” By participating in the trial, the patient is agreeing to complete surveys periodically, which will help researchers determine if there are differences between proton therapy and IMRT. The results of this study will be of significant value in helping future patients with their treatment decisions.
Watch the COMPPARE trial patient recruitment video.
We encourage you to visit the COMPPARE website to learn more about this important study. We will be providing updates in future issues of BOB Tales.
Tennessee Passes Proton Therapy Law
 BOB member Don Denton was treated in 2011 at UFHPTI. He told Bob Marckini that Bob’s book was a key reason he chose proton therapy for his prostate cancer. Don’s insurer initially denied coverage; but Don fought the battle through the appeals process, and eventually won.
BOB member Don Denton was treated in 2011 at UFHPTI. He told Bob Marckini that Bob’s book was a key reason he chose proton therapy for his prostate cancer. Don’s insurer initially denied coverage; but Don fought the battle through the appeals process, and eventually won.
Don lives in Tennessee, a state that has three proton centers, and Don has devoted an enormous amount of his time and energy spreading the word on the benefits of proton therapy within his state, as well as attempting to turn the tide on insurers denying coverage. Don founded the Tennessee Cancer Patient Coalition in 2015 and has been lobbying local media and working with the Tennessee Legislature promoting proton therapy bills for the past several years. Don is justifiably happy with something that has just happened in his state. We asked him to write an article about it for this issue of the BOB Tales and here it is:
By a vote of 26-1 in the Senate and 94-0 in the House, the Tennessee Legislature recently passed the Proton Therapy Access Act. I’m delighted to report that Gov. Bill Lee signed the bill into law on April 25th. It represents a small but significant step toward all Tennesseans having access to the world’s most advanced cancer treatment available in their own state.
Per capita, Tennessee ranks number 22 in cancer diagnoses, but number 5 in cancer deaths and number 1 in proton therapy treatment capacity. It’s a strange anomaly that shouldn’t exist. The new proton law will help correct this problem.
The bill, known as SB 0195/HB 0184, requires the state-funded insurance plan for people covered by it to cover hypo-fractionated proton therapy at the same reimbursement rate as conventional IMRT. It will positively impact 300,000 state employees and their dependents.
Achieving this milestone hasn’t been easy and has taken more than five years to reach. The Tennessee Legislature prides itself on being fiscally conservative and business friendly. It has steadfastly refused any proton therapy insurance coverage that would have a fiscal impact or be considered a mandate. This year’s bill satisfies both conditions, since proton therapy is being offered at no cost increase to the state, taxpayers, insurance company or cancer patient, and since it applies only to a state-funded plan, it isn’t a mandate on private business.
Virtually the same bill passed last year, but it was vetoed by the previous governor. One significant accomplishment by the proponents of the bill has been to correct the misrepresentations of the insurance lobby that has opposed it for so many years. Again, this year’s bill represents a first step. With each year proton therapy advocates will press for expanding coverage to all Tennesseans. The war certainly isn’t over; in many ways it has just begun.
Note: The two primary proponents in Tennessee’s legislative efforts have been Provision Healthcare, the owner of two proton centers in the state, and my organization, the Tennessee Cancer Patient Coalition.
BOB Comment 1: In the article Don notes that Tennessee ranks number 1 in proton therapy treatment capacity. We questioned him on this, because other states like Florida and California have more treatment rooms than Tennessee, but what Don was referring to is the fact that the two Provision proton centers (Knoxville and Nashville) have a total of eight treatment rooms and St. Jude has two, for a total of 10 treatment rooms for a state population of 6.77 million people, or one treatment room per 677,000 people. This probably is a higher ratio of treatment rooms per capita than Florida or California.
BOB Comment 2: Another BOB member who is a highly respected political figure in his state has also been working tirelessly to pass legislation in favor of proton therapy insurance coverage for treating prostate cancer. He is making great progress and we hope to be able to make an announcement on this in next month’s BOB Tales.
Short-term ED after Prostate Needle Biopsy
The transrectal prostate biopsy is the most common type of biopsy (biopsies can also be transurethral or perineal). In a recent study, researchers analyzed the rate of erectile dysfunction (ED) in patients under-going transrectal ultasound-guided prostate biopsy.
Details
Eighty candidates (average age 64.8) were enrolled. They completed a standard diagnostic questionnaire one month before, and one, three, and six months after they were biopsied. Those with a previous history of ED were excluded from the study.
Results
Results showed that transrectal needle biopsy of the prostate causes progressive ED. According to researchers, the relationship is not affected by the biopsy result, prostate volume, or the PSA level.
The reasons are unclear as to why the transrectal biopsy caused progressive ED, though experts suggest multiple factors could ultimately influence or disrupt normal erectile function after prostate biopsy including type of anesthetic, age, psychological stress, and damage to the neurovascular bundles (the last being uncommon). ED associated with prostate biopsy typically lasts a few weeks.
Other Studies
Two older studies also found that men may develop ED after prostate biopsy. In 2015, researchers studied 220 men who underwent transrectal prostate biopsy. The men’s ED was assessed before the biopsy and again at one, four, and 12 weeks afterward.
ED was more severe at all three intervals, however the team didn’t say the needle caused physical damage in this nerve-intensive area that led to ED. Researchers were again unclear as to why ED declined but they also thought “psychological stress” could be a factor.
Researchers noted that those who had a benign biopsy had a fairly quick return to baseline in terms of their ED. They also said a prostate cancer diagnosis “can influence a man’s erectile function after prostate biopsy.”
Another study, published in 2016, examined ED after transrectal prostate biopsy. Four weeks after the biopsy, about a third of the men had some degree of ED.
Before a biopsy, men should discuss with their urologists the possibility of short-term ED.
Prostate Cancer Diagnoses, Deaths Decreasing Worldwide; Highest Decrease in U.S.
Rates of prostate cancer cases and deaths have declined or stabilized in most parts of the world, according to a new study CNN shared. The U.S. had the largest recent decrease in disease incidence.
Previous studies have outlined considerable variation in prostate cancer rates due to factors including detection practices, availability of treatment, and genetic factors.
“By comparing rates from different countries, we can assess differences in detection practices and improvements in treatment,” said MaryBeth Freeman, lead study author and senior associate scientist of surveillance research at the American Cancer Society.
Freeman said the findings confirm the benefits of PSA screening. She noted that in the U.S., incidence rates rose from the 1980s to the early 1990s, and then declined from the mid-2000s through 2015, largely due to increased use of PSA screening.
PSA screening is less available in poorer nations. As a result, men in those areas are more likely to be diagnosed at later stages of disease and more likely to die, according to Freeman.
Freeman noted that some nations plan to scale back recommendations for PSA screening due to concerns about overtreatment. Dr. Eric Horwitz, professor of medicine at Fox Chase Cancer Center in Philadelphia, said this line of thinking is “potentially problematic.”
 The U.S. Preventive Services Task Force recommends that men aged 55 to 69 undergo periodic screening after they’ve discussed the risks and benefits with their doctor. They suggest the decision of whether or not to screen should be an individual one. They further recommend men age 70 and older should not be screened, as the harms outweigh the benefits for this age group.
The U.S. Preventive Services Task Force recommends that men aged 55 to 69 undergo periodic screening after they’ve discussed the risks and benefits with their doctor. They suggest the decision of whether or not to screen should be an individual one. They further recommend men age 70 and older should not be screened, as the harms outweigh the benefits for this age group.
“The screening recommendations were changed recently after further analysis of the U.S. data and we’re seeing more high-risk prostate cancer diagnoses that require treatment,” said Horwitz, who wasn’t involved with the study.
Freeman said future studies should monitor trends in mortality rates and late-stage disease to assess the impact of reduction in PSA testing in several countries.
Insurance Denied When Most Needed
 This story is not about prostate cancer, but many of you can relate to dealing with health insurance issues for proton therapy coverage. Please read Miriam’s story and how she’s holding her insurance company accountable. Then, consider taking a stand.
This story is not about prostate cancer, but many of you can relate to dealing with health insurance issues for proton therapy coverage. Please read Miriam’s story and how she’s holding her insurance company accountable. Then, consider taking a stand.
Recently, the California Supreme Court decided to let stand a state appeals court ruling that paved the way for $91 million in fines against a UnitedHealthcare subsidiary, a major victory for California patients who were wrongfully denied life-saving treatment. The scale of violations by the insurer—more than 900,000 improper denials—demonstrates the power imbalance between patients and insurers.
Miriam’s Story
Though Miriam Tariq wasn’t one of the 900,000 denials mentioned above, she learned firsthand how overwhelming a fight with an insurer can be when she was diagnosed with breast cancer in her early 20s. Not only was she forced to struggle with a life-threatening diagnosis; she also had to fight her health insurer for physician-recommended treatment.
 Results from a routine genetic test revealed that Miriam was predisposed to secondary cancers due to a genetic condition. Therefore her doctors ruled out traditional radiation treatment as too risky and recommended proton therapy because it would significantly reduce the risk of developing secondary cancers. “It was a no-brainer to everyone but UnitedHealthcare,” said Miriam. The company denied her claim based on outdated 2012 clinical guidelines, referring to proton therapy as unproven and unnecessary. However, the guidelines had long been updated to recommend proton therapy for breast cancer patients.
Results from a routine genetic test revealed that Miriam was predisposed to secondary cancers due to a genetic condition. Therefore her doctors ruled out traditional radiation treatment as too risky and recommended proton therapy because it would significantly reduce the risk of developing secondary cancers. “It was a no-brainer to everyone but UnitedHealthcare,” said Miriam. The company denied her claim based on outdated 2012 clinical guidelines, referring to proton therapy as unproven and unnecessary. However, the guidelines had long been updated to recommend proton therapy for breast cancer patients.
Following the denial, there was a peer-to-peer review between the insurer and Miriam’s physician. According to Miriam, the insurer’s representative wasn’t qualified to review her case as she wasn’t a radiation oncologist and had no knowledge about proton therapy.
Miriam started proton therapy at California Protons while continuing to fight for insurance coverage. While undergoing treatment, she took her denial fight to the California insurance commissioner. Six months after she completed treatment, the commissioner overruled UnitedHealthcare and sided with Miriam’s doctors.
Though Miriam’s situation ended well, her experience illustrates a problem with a system where broken insurance processes make it nearly impossible for cancer patients to receive the best care. Miriam said, “While cancer interrupted my senior year of college at UC Santa Barbara, my insurer’s actions caused me the most stress.”
Like Miriam, many cancer patients are left waiting as insurers drag them through appeals while their cancers grow. In fact, a report from the Alliance for Proton Therapy Access revealed that four in 10 cancer patients are denied care that their doctors recommend and wait more than five weeks on average before receiving a final denial.
It’s time for federal legislators to examine this problem and put a stop to improper denials. Please join advocates across the country in calling on lawmakers to adopt principles of a Cancer Patients’ Timely Treatment Bill of Rights into legislation.
Professor Receives NIH Grant to Study the Role of Stress Hormones in Prostate Cancer Health Disparities
Carlos A. Casiano, PhD, Professor of Basic Sciences and Associate Director of the Center for Health Disparities and Molecular Medicine (CHDMM) at Loma Linda University Health, was recently awarded by the National Cancer Institute an R21 grant of $378,015 to explore the contribution of a protein called glucocorticoid receptor (GR) to prostate cancer health disparities. GR is activated by the glucocorticoid hormone cortisol in response to stress, and mediates molecular events that help the body respond to stressful events. However, lifetime cumulative exposure to stress may lead to chronically elevated levels of cortisol and increased GR function, contributing to the development of chronic diseases.
African American men experience more lifetime cumulative stress than other racial groups, and suffer from a disproportionately high incidence and mortality of prostate cancer. Elevated GR function has been recently linked to increased resistance to therapies for advanced prostate cancer, such as androgen deprivation therapy and chemotherapy, but the molecular mechanisms are unknown. In pilot studies supported by the CHDMM, Casiano’s team observed that exposure of prostate cancer cells to glucocorticoids caused the activation of GR and genes associated with chemotherapy resistance.
The two-year grant will explore if GR function is more elevated in prostate tumors from African American men compared to men from other racial groups, and investigate how it contributes to chemotherapy resistance. Casiano’s team will conduct molecular studies using cellular and animal models of prostate cancer, and biospecimens from prostate cancer patients and controls. The team will also mine data from psychosocial and socioeconomic surveys provided by African American men participating in Project CHANGE, a community engagement initiative sponsored by the CHDMM in collaboration with Loma Linda University’s schools of Behavioral Health and Nursing that seeks to increase awareness of prostate cancer among Black men. The goal will be to identify potential links between chronic psychosocial stress and early markers of aggressive prostate cancer.
Casiano’s research could help discover biological factors that contribute to the aggressiveness of prostate cancer in African American men. This would lead to the future development of more effective treatments for therapy-resistant prostate cancer, and the reduction of racial disparities in prostate cancer mortality. This research will be conducted at the CHDMM in collaboration with Susanne Montgomery (Associate Dean for Research, School of Behavioral Health) and a team of basic and clinical investigators in the CHDMM, the Center for Genomics, the Departments of Urology and Pathology, the Cancer Center, and the Schools of Nursing and Allied Health.

We have been producing BOB Tales newsletters monthly for more than 18 years. During this time there have been important articles that many new members have not seen, and some older members may have forgotten. So, we decided to periodically re-run some articles from past newsletters. This one is from January 2005.
The PSA Bump
One of our members had a pretreatment PSA of 5.4. As expected, following treatment his PSA began to fall to below 2.0. But then it rose to 2.8 and higher. A month of antibiotics for possible infection didn’t seem to make a difference, as his PSA climbed to 5.0.
He wanted a recheck of his PSA, but his urologist said it would be a waste of time and suggested he immediately begin triple blockade hormone therapy. Instead he went to see an oncologist who rechecked his PSA, which was back down to 1.8. Another check a month later reported 1.4 and it has continued to drop. So things seem to be back on track, thankfully.
What’s the message here? Don’t panic if you experience a bump in your PSA. Always recheck a suspicious PSA reading. Get a second opinion, and even a third, if appropriate.
PSA bumps are common, especially during the first couple of years after treatment.

A Note from Bob Marckini (BOB Tales, Dec. 2013)
Until I became involved in helping Loma Linda raise money for proton research, I had a very different perspective on charitable solicitations. Sure, I dutifully made weekly contributions at church, threw a few dollars into the Salvation Army bucket, and occasionally wrote a check to St. Jude’s hospital or some other worthy cause. But the contributions were generally small and often given begrudgingly. The ubiquitous mail solicitations promptly went into the waste basket, unopened.
Today I have a completely different perspective on charitable giving. Through my involvement in the LLUCC Advisory Council along with other BOB members who serve, I’ve had the opportunity to see firsthand how important every contribution is to advancing basic or clinical research programs. I’ve seen how the money is used to cure diseases, save lives, and preserve the quality of lives. I’ve also seen firsthand how important philanthropy is to institutions like Loma Linda University Health. And I’ve learned how difficult it is to raise money, and how very hard it is to ask someone to contribute to a charity you are connected with or feel passionately about.
I’ve come to believe that everyone at some point in their lives should involve themselves with a charity by volunteering their time and committing their resources. You’ll learn a lot about how necessary charitable giving is, and you’ll help the institution with their important work. You’ll also feel good about yourself.
Today the amount my wife and I give to church and charities is far greater than what we’ve given in the past, and we give with enthusiasm. We no longer automatically dump mail solicitations in the trash. We contribute annually to Loma Linda and have designated part of our estate plan to Loma Linda. We do this enthusiastically because we’ve seen how desperately the money is needed and what good our contributions can do.
Most of us have far more material things in our lives than we need, and we continually add to them. Supporting proton research is a great opportunity to divert a portion of that spending to a better place; to do something that will have a lasting benefit for generations to come. Please consider giving something back.
How to Give to Proton Therapy Research
- Donate Online: Visit the LLUCC website.
- Send a Check: Make it out to “LLUCC Proton” with “Marckini Chair” on the memo line and send to: LLUH, Office of Philanthropy, P.O. Box 2000, Loma Linda, CA 92354.
- Make a Call: Contact Regina Joseph at 909-558-5010.
Recap: 2019 National Proton Conference
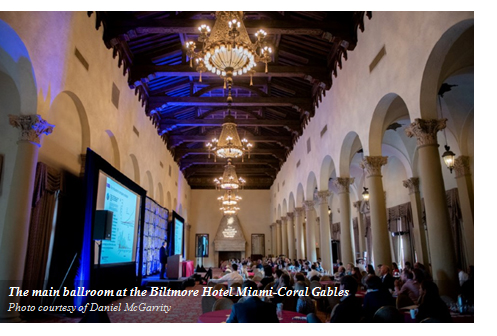 The seventh annual National Proton Conference was held at the Biltmore Miami-Coral Gables from March 24 - 27. The goal of this year’s conference was to serve as an extension of NAPT’s mission to educate and increase awareness about the clinical benefits of proton therapy; ensure patient choice and access; and to encourage cooperative research and innovation.
The seventh annual National Proton Conference was held at the Biltmore Miami-Coral Gables from March 24 - 27. The goal of this year’s conference was to serve as an extension of NAPT’s mission to educate and increase awareness about the clinical benefits of proton therapy; ensure patient choice and access; and to encourage cooperative research and innovation.
The event was attended by proton center clinical and administrative leaders representing 29 U.S. proton centers and some overseas. Additional attendees included representatives of hospitals and medical centers who are either building proton centers or considering building proton centers; attorneys from several international law firms who spoke about disruptors in the health plan marketplace, proton therapy patient litigation, and coverage and reimbursement issues; and vendors who design and make equipment, products, and systems that support proton therapy and related technologies. There were also two eloquent opening speakers this year: Keynote speaker, Barbara L. McAneny, MD, president, the American Medical Association, and guest speaker, Florida Sen. Marco Rubio.
.jpg) Scott Warwick, NAPT’s executive director, and the conference planning committee assembled an impressive program featuring remarkable presentations covering relevant topics facing proton therapy today and into the future. The conference consisted of numerous panel discussions, as well as an exhibit hall with 24 displays highlighting the latest in proton treatment center design and medical devices used to enhance treatment and minimize side effects. More than 280 attended this year’s conference—a new record.
Scott Warwick, NAPT’s executive director, and the conference planning committee assembled an impressive program featuring remarkable presentations covering relevant topics facing proton therapy today and into the future. The conference consisted of numerous panel discussions, as well as an exhibit hall with 24 displays highlighting the latest in proton treatment center design and medical devices used to enhance treatment and minimize side effects. More than 280 attended this year’s conference—a new record.
As mentioned in last month’s BOB Tales, Deb Hickey was asked by NAPT for the second time to speak on a panel. This year’s topic was Patients as Advisers and Partners. Following are highlights from the conference that we think would be of interest and valuable to our readers, in addition to a recap of Deb’s presentation.
Prior Authorization Hurts Patients and Physicians
The conference kicked off with a keynote presentation by Dr. Barbara McAneny, president of the American Medical Association. She spoke about the AMA’s goal to attack the dysfunction in the healthcare system by removing obstacles and burdens that interfere with patient care—primarily, prior authorization. Prior authorization forces physicians to have to contact their patients’ insurance companies to obtain approval before the treatment they recommend to their patients can begin. This process of submitting paperwork and following up with insurers takes doctors and their staff a significant amount of time. As a result, treatment is often delayed for weeks as insurers review requests. And when time is wasted, patient health can suffer.
 The AMA recently surveyed 1,000 doctors on the issue of prior authorization. They uncovered some disturbing statistics about what happens to patients when they have to wait for prior authorization before they can be treated. Ninety-one percent of the physicians said the prior authorization process had a negative impact on patients, which caused adverse results. In many cases, patients abandoned treatment due to delays caused by cumbersome prior authorization requirements.
The AMA recently surveyed 1,000 doctors on the issue of prior authorization. They uncovered some disturbing statistics about what happens to patients when they have to wait for prior authorization before they can be treated. Ninety-one percent of the physicians said the prior authorization process had a negative impact on patients, which caused adverse results. In many cases, patients abandoned treatment due to delays caused by cumbersome prior authorization requirements.
Dr. McAneny and her team at the AMA have partnered with healthcare providers and health plans to identify opportunities to improve the prior authorization process. Their goal is to promote safe, timely, and affordable access to evidence-based care for patients; enhance efficiency; and reduce administrative burdens. She stressed the importance of communication and collaboration to achieve those goals, including getting Congress involved. The AMA launched a grassroots website to support this effort.
Dr. McAneny spoke specifically about barriers to patients receiving proton therapy. She stressed the importance of collaboration—among proton centers and others in the industry—to track patient results; get patient stories to the press; use social media to educate and spread awareness; and contact state legislators.
Socioeconomic Disparities in Health
Florida Sen. Marco Rubio took the stage to discuss the need to make proton therapy more widely available to those who need it. He noted the extraordinary disparities in accessing healthcare depending on where you live. A friend of Rubio’s was recently diagnosed with breast cancer. He encouraged her to get multiple opinions on treatment, including proton therapy, even if she had to go out of state. That brought up questions as to why less invasive treatments, like proton therapy, were not suggested by her doctor. Often, the treatment isn’t easily accessible and more often than not, physicians are uninformed about proton therapy.
 Rubio stated that to make proton therapy more easily accessible, it’s key to look at it from both the state and federal level.
Rubio stated that to make proton therapy more easily accessible, it’s key to look at it from both the state and federal level.
In an ideal world, where all medical decisions are made using analytics at lightning speed, the rate of innovation would accelerate rapidly. To make that happen, we need regulation and federal acknowledgement, which Rubio plans to initiate.
He spoke about the lack of long-term thinking in the healthcare industry and that there’s more interest in short-term gain. “I believe it’s a priority not to simply extend life, but to ensure there is quality of life,” he said. “This requires more investment at the basic level of research.”
Sen. Rubio also mentioned a new dynamic among patients: they educate themselves easily by going online—and in turn, they approach their healthcare provider and demand the best available treatment. However, this isn’t universally true. Socioeconomic background matters. Socioeconomic status underlies three determinants of health: care, envirormental exposure and behavior. Reducing these disparities requires new policy initiatives addressing components of economic status—income, education, and occupation.
Rubio also spoke candidly about his personal experience with pediatric cancer in the family. “I watched a family member go through cancer treatment for years—first with leukemia, and then myeloma,” he said. “From age 11 to 17, he lived with a port and antibiotics. He didn’t go to school. He didn’t have a childhood.” Through watching his family member suffer, Rubio saw the human side of cancer. He told attendees that this boy had recovered and was looking at a career in cancer research. “We should encourage our children to get interested in cancer research,” he said. “Attracting more people in this profession is critical for the future of our country.”
Topics, Discussions, and Comments that Caught Our Interest
Disruptors/Disruptions in the Health Plan Marketplace
- Emerging technologies in artificial intelligence, blockchain, cloud computing, and genomics fields are likely to become more prevalent in healthcare over the next 10 years.
- Major players outside the industry have grasped the magnitude of this opportunity—Amazon, CVS, Apple and others.
- Healthcare is fertile for disruption for many reasons: there’s a constant need by the patient/consumer to “want better,” mostly because they’re taking over more and more financial responsibility; there’s also a high level of consumer dissatisfaction with healthcare.
- Among the most important players in healthcare’s disruption story are the patients. After years of dealing with limited options, consumers have choices.
- In the world of millennials, everything is digital; they’re using apps to make purchases and access healthcare; and they can pick among a variety of delivery models, including telemedicine, home health, concierge care, and self-help.
- While healthcare has a long way to go before it can be considered consistently customer-centered, these new channels offer consumers qualities they look for from other service providers including convenience, attentiveness, timeliness, value, and price transparency.
 What can we expect to see in the next five to 10 years and how can we prepare for it?
What can we expect to see in the next five to 10 years and how can we prepare for it?
- It’s all about consumers and they want convenience.
- It’s about being preemtive—have a product or service that the consumer doesn’t know he wants or needs, but once you get him to use it, he can’t imagine life without it.
- It’s about price transparency—exactly how much will this cost? Think outside the box—people you think have nothing to do with healthcare will become our future partners.
- At the cutting edge is proton therapy, yet everyone else is going to be innovative and looking to build better and greater technologies.
- Figure out how you belong. Where, in the past, doctors had the greatest knowledge, now patients do.
- Think like Steve Jobs; he never talked to the consumer about the iPhone; he just created it. Now everyone has one.
Proton Therapy Reimbursement Issues
 There’s a short-range view from lots of insurers, so they don’t want to insure.
There’s a short-range view from lots of insurers, so they don’t want to insure.- The insurance companies and healthcare industry aren’t hurting; there were massive profits last year—$56B in revenues with a profit of $3+B; others in range of $10-20B with profits of $1B for the quarter. If you took all the charges for proton therapy, it wouldn’t add up to any one of those quarterly profits for an insurer, certainly not for the entire group. Insurance companies are looking at a quarterly basis—a timeline of 1-5 years seems like a long time when thinking about quarterly earnings.
- What are the insurers’ reasons for not covering proton? They define it as “investigational.” A second way to deny coverage is to create delays—they don’t update their policies; they use others to do the initial screening; there are multiple layers to go through for approval; and they make unnecessarily high levels of evidence requirements for any changes in their policies and approval process.
- Most insurance claim reviewers have no idea what they’re doing; “their solution is to pull out an old policy and act like English is a second language.”
- Proton centers need to look at a different way of doing things, including having a centralized patient navigator, and adding a financial person, managed care coordinators, two coders to do all denials management, and perhaps a medical dosimitrist on the patient authorization team.
An Overview of the Proton Therapy Patient Litigation in Oklahoma: Ron Cunningham vs. Aetna Life Insurance Co.
The attorneys who worked on Ron Cunningham’s case, as well as the radiation oncologist who testified at the trial, presented the details of this case to NAPT attendees. Deb felt it was one of the highlights of the conference and a huge step in highlighting the critical problems with health insurance reimbursement for proton therapy
Ron Cunningham, a retired Oklahoma City firefighter, had battled for justice for his wife for 3 ½ years. Orrana was diagnosed with Stage IV nasopharyngeal cancer in November, 2014 when she was just 53 years old. She was diagnosed a couple of months after they’d finished building a house (almost entirely with their own two hands) on a farm in eastern Oklahoma County.
 The Cunninghams immediately sought medical advice in Oklahoma City and were told, due to the complexity of her disease, they should go to MD Anderson. The doctors there evaluated Orrana and determined she needed proton therapy. Her tumor was at the base of her skull, adjacent to multiple “critical structures” in her head—her brain, her optic nerves, and her brain stem. The MD Anderson physicians told Ron and Orrana they could kill the tumor with either proton therapy or traditional radiation, but proton therapy would increase the chances that she’d be cured without devastating side effects, including (among others) blindness, loss of memory and loss of the sense of taste.
The Cunninghams immediately sought medical advice in Oklahoma City and were told, due to the complexity of her disease, they should go to MD Anderson. The doctors there evaluated Orrana and determined she needed proton therapy. Her tumor was at the base of her skull, adjacent to multiple “critical structures” in her head—her brain, her optic nerves, and her brain stem. The MD Anderson physicians told Ron and Orrana they could kill the tumor with either proton therapy or traditional radiation, but proton therapy would increase the chances that she’d be cured without devastating side effects, including (among others) blindness, loss of memory and loss of the sense of taste.
For obvious reasons, the Cunninghams wanted proton therapy, so MD Anderson submitted a request for coverage to Aetna on their behalf. The evidence at trial showed three Aetna nurses and three Aetna in-house “medical doctors” denied the claim because proton therapy is “experimental or investigational.” An Aetna medical director, previously an internal medicine/family practice doctor who hadn’t treated a patient for 25 years, also denied the claim. Furthermore, the Aetna doctors had never heard of the duty of good faith; had never received any training on the obligations owed by Aetna to its insureds under Oklahoma law; were sorely overworked; and were receiving sizable bonuses each year, based in part on the profit of Aetna. Each of the medical directors spent about 30-45 minutes reviewing the claim (including a 150-plus page appeal package sent to them by MD Anderson), and at trial, they claimed to have read everything in the file in that amount of time.
Also, the evidence at trial was that none of the medical directors even read the insurance contract before denying the claim. Instead, they relied on Aetna’s “Clinical Policy Bulletin” as the basis of their denial, which is not a part of the insurance contract Aetna sold the Cunninghams. Furthermore, it’s outdated, skewed and cherry-picked in the way it refers to the medical literature, and not designed to decide claims, but only to serve as a resource for the Aetna medical directors if they need it.
After the denials, Ron went to his bank in Oklahoma and borrowed $92,082.19—the cost of Orrana’s treatment—against the dream house he and Orrana had built.
Orrana was treated with proton therapy, and it appeared to work. She was released to go home after six weeks, and got to “bang the gong” at MD Anderson, symbolizing the end of her treatment. Still, the evidence was the financial stress of the whole situation (in addition to the fact she was battling cancer) weighed on her heavily. After arriving home, Orrana developed an outbreak of herpetic encephalitis—her brain had swelled, causing her brain stem to herniate and she passed away. Ron filed his lawsuit shortly thereafter.
The jury found:
- Aetna breached its insurance contract with the Cunninghams and awarded them the $92,082.19 they paid out of pocket. This could be important in the course of the ongoing effort by the insurance industry to restrict access by patients to protons. In effect, the jury determined the experimental and investigational exclusion in the policy does not apply to exclude proton therapy in this situation.
- Aetna acted in reckless disregard of the duty of good faith and fair dealing it owed the Cunninghams in connection with the way it investigated and evaluated their request for coverage for proton therapy.
The jury awarded compensatory damages for the emotional distress caused by Aetna’s repeated denials. They awarded Mr. Cunningham $500,000 individually. Then they awarded Mrs. Cunningham’s estate $15 million. The attorneys on the case also proceeded to a punitive damage phase of the trial, arguing to the jury that to send Aetna away without punishing them for what the jury had already found was reckless conduct wouldn’t be a just result. The jury agreed and awarded another $10 million. This brought the total verdict to $25,592,089.19.
Ron Cunningham says his goal has always been to bring Aetna’s conduct into the public light, hoping Aetna will change the way it does things in the future. He doesn’t want what happened to Orrana to happen to anyone else.
Advocating for Today’s Cancer Patient
- The American Cancer Society is leading the fight for a “world without cancer” by:
- Investing in promising cancer treatments;
- Funding research that’s promising;
- Working to remove barriers to cancer care;
- Working to improve access to care; to make it accessible and affordable.
- Access to care and information should be easy.
- They have a live 1-800 helpline operating 24/7 (1-800-227-2345).
- The website includes a live chat function.
- Via the two methods mentioned above, patients have access to trained specialists who speak multiple languages; they can connect patients to local and national resources.
- The AMA offers a transportation program intended to provide service to patients at no cost.
- Volunteers have donated their cars and personal time to transport patients.
- Car dealerships have made their cars available to patients.
- The AMA has partnered with ride-sharing services like Lyft and public transit, as well as other non-emergency transport providers.
- The AMA has partnered with hotels to provide lodging assistance to patients at either no cost or low-cost. There’s a large number of patients who use this service while undergoing proton therapy treatment.
- The Alliance for Proton Therapy Access works to make sure all cancer patients seeking proton therapy receive fair and timely payment decisions from their health insurers.
- Too many people are suffering undue health risks, anxiety, and financial hardship when insurers subject them to lengthy, confusing appeals processes that delay and in some cases, deny treatment.
- Their mission is to attain a fast, fair, and transparent insurance review process for cancer patients in need of proton therapy.
- The Alliance has helped many patients reach and communicate with the media (sometimes just the threat of going public has reversed denials).
- They are fighting for better public policy with a national education and advocacy campaign and their online advocacy toolkit.
Clinical Trials in Proton Therapy
- Proton Therapy vs. IMRT for Prostate Cancer
- The COMPPARE Trial: Patients will enter the trial after choosing proton therapy or IMRT to treat their cancer; they won’t be randomized; they’ll receive the same standard of care treatment; and comparison of results will include patient-reported quality of life; physician-reported toxicity interventions; and disease control as measured by freedom from PSA progression.
- Hypotheses for the trial include:
- Patient-reported quality of life results: Proton therapy will reduce bowel dysfunction and rectal toxicity compared with IMRT.
- Proton therapy will produce disease control equal to or superior to IMRT.
- Moderately fractionated (20 fractions) proton therapy will be as effective and safe as standard fractionated (39 fractions) proton therapy.
- After a slow start, there are 80 patients enrolled and 15 in the pre-enrollment process. They are awaiting activation of all other sites, and then looking to accrue rapidly. The goal is to enroll 3,000 patients—1,500 per arm.
- Proton Therapy vs. Photon for Esophageal Cancer – Hypotheses:
- Proton therapy for esophageal cancer improves the dosimetric sparing of the heart and lungs compared to IMRT.
- Toxicity sparing effects may translate to improving quality of life and possibly provide overall survival benefit.
- Proton Therapy vs. Photon for Breast Cancer – Hypotheses:
- Radiotherapy plays a major, curative role in the treatment of patients with breast cancer.
- Because of incidental radiation to the heart, radiotherapy carries increased risks of cardiovascular morbidity and mortality.
- Proton therapy, by reducing the volume of heart exposed to radiation in the treatment of breast cancer, has the potential to lessen the morbidity of radiation therapy compared to photon therapy.
The Benefits of Proton Therapy for Pediatric Patients
- Pediatric Brain Cancer
- Dose matters: Even small dose differences to important brain regions can have a significant impact on neurocognitive function. The more radiation—the more damage done.
- Location matters: some areas of the brain do more heavy lifting than others in regard to neurocognition.
- The ability to spare dose to important regions in the brain can improve a child’s neurocognitive potential and preserve quality of life.
- Protons provide the best radiation tool for minimizing excess dose to brain regions outside the target volume.
Advantages in Proton Technology
 There was lots of interest in “flash” proton radiation therapy—ultra-high-dose rate external beam therapy delivered in less than one second in hypofractionated form.
There was lots of interest in “flash” proton radiation therapy—ultra-high-dose rate external beam therapy delivered in less than one second in hypofractionated form.
- Flash proton therapy was tested on mice.
- Flash dose rate caused little skin reaction.
- Whole brain flash irradiation spares memory.
- In administering whole animal radiation, with conventional radiation, all mice were dead within 10 days. With flash proton radiation, the mice were alive at two weeks and recovery of stem cells suggested protection of blood lines.
- Researchers also measured gastrointestinal crypt cells under conventional and flash conditions. With flash, crypt cells were preserved; also showed crypt regeneration.
- The best clinical evidence is that this effect is real and could translate to larger animals.
- Flash RT allows dose escalation that has anti-leukemic effects as tested on animals.
- Flash offers a rare opportunity that could completely transform the field of radiation.
- There’s a large body of evidence starting to emerge.
- Proton Arc Therapy
- The arc technique could enhance dose conformity at tumor level while reducing total patient dose.
- With arc therapy, treatment time is shorter, more efficient, and patient comfort is improved.
Lifetime Achievement Award Winner
George Laramore, MD, PhD, FACR, FASTRO, of the Seattle Cancer Care Alliance Proton Therapy Center and the University of Washington is this year’s NAPT Lifetime Achievement Award winner. This award recognizes pioneers in the field of particle therapy who have brought honor and distinction to the field. Dr. Laramore will join an esteemed group of recipients including Dr. Herman Suit, Dr. James Slater, Dr. James Cox, Bob Marckini, and Len Arzt.
 Dr. Laramore led numerous clinical trials, both early phase and randomized trials to test the value of neutron therapy for patients. As an author or co-author of 14 clinical trials examining neutron therapy, Dr. Laramore is one of the foremost clinical trialists in particle beam therapy. Further underscoring his reputation in the field of particle beam therapy, in 1997, Dr. Laramore was issued a patent for Boron Neutron Capture Therapy Enhancement of Fast Neutron Radiotherapy.
Dr. Laramore led numerous clinical trials, both early phase and randomized trials to test the value of neutron therapy for patients. As an author or co-author of 14 clinical trials examining neutron therapy, Dr. Laramore is one of the foremost clinical trialists in particle beam therapy. Further underscoring his reputation in the field of particle beam therapy, in 1997, Dr. Laramore was issued a patent for Boron Neutron Capture Therapy Enhancement of Fast Neutron Radiotherapy.
Dr. Laramore was a tireless proponent of bringing proton beam therapy to the Pacific Northwest. The SCCA Proton Center opened for treatment in Seattle in March 2013, due in large part to Dr. Laramore’s tireless advocacy and his steadfast belief in the science of proton beam therapy
“I am overwhelmed by NAPT giving me this award, particularly in view of the outstanding Radiation Oncologists who have previously received it,” said Dr. Laramore. I have spent most of my professional life working with particle radiation of one form or another — first neutrons and then protons. While not appropriate for every cancer patient, it is clear to me that there are many patients who can be best served by proton therapy. I am so grateful I have been able to help make this treatment available to them.” He also said, “I want to acknowledge the support of my wife and family during this journey.”
 Patients as Advisers and Partners
Patients as Advisers and Partners
On the “Patients as Advisers and Partners” panel, Deb Hickey spoke about the BOB and our strong and growing community of men who are willing to share with others their very personal lives because they’re so thankful for proton treatment. She talked about the many ways our members help us achieve our goal of spreading awareness and educating others about proton therapy by connecting with people in their community and educating them about proton therapy and also answering their questions about treatment and life after treatment. Our members do this through:
- Writing testimonials for our website;
- Agreeing to “Life After Proton” short stories on our website;
- Forwarding information from our newsletter or the entire newsletter to family and friends;
- Using the BOB PowerPoint to address their local community: Lions Clubs, church groups, support groups, work groups, retirement communities, etc.;
- Volunteering to be on our former patient reference lists (nearly 40 separate lists);
- Ordering and handing out Bob Marckini’s book to family, friends and acquaintances; place the book in doctor’s offices, libraries, etc.;
- Creating and maintaining their own blogs about proton therapy;
- Writing books about their experience with proton treatment;
- Engaging in political efforts;
- Establishing local support groups.
Deb also spoke about the COMPPARE trial and the key role the BOB will play in helping to accrue proton patients.
Summary
This is just a sampling of the events at NAPT 2019. Every NAPT conference allows members of the proton community to network, share information, discuss challenges, and build relationships. The take-away from the Miami conference is that the world of proton therapy is still growing rapidly and much progress is being made on all fronts. Many are getting more involved in the proton therapy “movement,” including large health organizations, international law firms, and politicians; and we are working together on behalf of patients to achieve easier access to proton therapy, change and update medical insurance policies, create new technologies to equip patients with better care.
Until next year in Nashville!
Upcoming: LLUCC Proton Charity Invitational
 The Loma Linda University Proton Charity Invitational began 28 years ago to help fund proton therapy research so clinicians and researchers can continue their work in basic and clinical research to aid people in the fight against cancer. This year’s event will be hosted by John Cook at The Club at Morningside—the first Jack Nicklaus-designed course in the Coachella Valley.
The Loma Linda University Proton Charity Invitational began 28 years ago to help fund proton therapy research so clinicians and researchers can continue their work in basic and clinical research to aid people in the fight against cancer. This year’s event will be hosted by John Cook at The Club at Morningside—the first Jack Nicklaus-designed course in the Coachella Valley.
The invitational begins on Monday, May 6, 2019. View the detailed brochure or contact Tricia Murdoch Zmaj for more information: Call 909-558-3742 or email [email protected].

Missed Cancer Screenings Linked to Earlier Death from Non-cancer Causes
Those who skip cancer screenings may be more likely than those who don’t to die prematurely from causes unrelated to malignancies, a U.S. study suggests. The researchers think skipping screenings may be an indicator for generally neglecting one’s health.
“Non-compliance with medical procedures has also been linked, in this and other studies, to other unhealthy lifestyle factors such as obesity and smoking, and to lower education,” said study co-author, Dr. Paul Pinksy of the National Cancer Institute.
Researchers examined data on 64,567 adults (average age 62) who were told to get screened for lung and colorectal cancers. Men were also advised to get tested for prostate cancer and women for ovarian cancer. Overall, 55,065 participants (85 percent) did what they were told and 6,954 (11 percent), didn’t. Within 10 years, those who didn’t get screened were 73 percent more likely to die of non-cancer causes than participants who got all of their screenings, the study found. Some screening was better than none at all, the researchers also found.
Even after researchers accounted for other factors linked to earlier death including smoking, obesity, and multiple chronic medical issues, compliance with cancer screenings still mattered.
“There is no way that getting screened for cancer can reduce the risk of dying of causes totally unrelated to screening,” said Dr. Deborah Grady of the University of California, San Francisco, who co-wrote an accompanying editorial. “What probably accounts for this association is the fact that people who follow advice to undergo screening have a lot of other health-related behaviors. It’s likely that it’s these sorts of behaviors that reduce the risk of dying.”
A Shockingly Large Majority of Health News on Social Media is Fake or Misleading
 You may be surprised to learn how much false information is on social media, especially Facebook. Health Feedback, a bipartisan network of scientists who collectively assess the credibility of health media coverage, worked together with the Credibility Coalition to examine the 100 most popular health articles of 2018—specifically, those with the highest number of social media engagements. Of the top-10 shared articles, they found that three quarters were either misleading or included false information. Only three were considered “highly credible.” Some lacked context of the issue, exaggerated the harms of a potential threat, or overstated research findings. Many writers either twisted data or simply couldn’t properly interpret it. Others, it seems, had an agenda.
You may be surprised to learn how much false information is on social media, especially Facebook. Health Feedback, a bipartisan network of scientists who collectively assess the credibility of health media coverage, worked together with the Credibility Coalition to examine the 100 most popular health articles of 2018—specifically, those with the highest number of social media engagements. Of the top-10 shared articles, they found that three quarters were either misleading or included false information. Only three were considered “highly credible.” Some lacked context of the issue, exaggerated the harms of a potential threat, or overstated research findings. Many writers either twisted data or simply couldn’t properly interpret it. Others, it seems, had an agenda.
The Health Feedback team believes the large number of “shares” of misleading news is partly due to sensationalized headlines that grab readers’ attention (e.g. clickbait). “This means the general public is more likely to come into contact with misleading information than accurate ones on social media,” says the research team.
Considering that social media algorithms incentivize engagement, this is not surprising: Fake news spreads more quickly and broadly than the truth in all categories of information, according to a recent report in Science. False or exaggerated stories often prey on people’s fear, disgust, or surprise. People are more likely to share what they emotionally connect with.
Health Feedback found that fake health news predominantly spreads on Facebook. The social media platform accounts for 96 percent of shares of the top-100 articles. Apparently the social media giant is aware of the issue and deleted dozens of pages dedicated to fringe or holistic medicine in an apparent crackdown on pseudoscience last year. However, its health news purge attracted criticism by those who viewed it as an attack on holistic or Eastern health practices as Facebook removed rather large accounts focused on health, natural remedies, and organic living.
According to Susan Krenn, executive director of the Johns Hopkins Center for Communication Programs, there’s been a sizable increase in inaccurate and downright false stories on social media platforms. Unfortunately, such postings possess far more sway than content outlets. Furthermore, when you see something posted on your social media site that comes from your peers, colleagues, or family members, you’re inclined to believe it.
BOB Comment: Numerous organizations are working on ways to tackle this problem. For example, developers and publishers are trying to build more thoughtful and balanced communities around their news. The Credibility Coalition, mentioned above, is working on a Web standard to support the detection of false and unreliable content.
Also, while researching this topic, we found a (credible) website offering tips and suggestions for how to spot false news, as well as an interesting article from Time, called “How Your Brain Tricks You Into Believing Fake News.”

New Amazon Review
 If you have prostate cancer, read this now! … This book opened my eyes to the different treatment options available. I’d never heard of proton therapy. Every doctor you see will recommend what they “do” for your treatment, not what may or may not be the best for you. Take the time to research your options and start with this book.
If you have prostate cancer, read this now! … This book opened my eyes to the different treatment options available. I’d never heard of proton therapy. Every doctor you see will recommend what they “do” for your treatment, not what may or may not be the best for you. Take the time to research your options and start with this book.
Thank you, Donald T. We think you hit the nail on the head.
Click here to write a review of Bob’s book. We read and appreciate every single one. More important, every review helps others find their way to proton therapy. Amazon’s most recent search engine algorithm for using reviews to boost a product’s visibility on specific search terms gives more weight to recent reviews, so we still need them!
Did you know?
- 70 percent of Amazon shoppers never click past the first page of results.
- 35 percent of Amazon shoppers click on the first product featured on a search page.
- The first three products siphon away around 64 percent of the clicks.
Buy Bob's book online, in bulk, or in Spanish.
Online: Paperback: $19.00--•--Kindle: $7.99--•--NOOK Book: $9.99--•--Apple iBook: $9.99
In Bulk: Conctact us for a discount price list. Proceeds from book sales support proton therapy research through the Robert J. Marckini Endowed Chair at LLUCC.
In Spanish: Buy the print version or in eBook format.

Keep Food Fresh Longer
The average family wastes thousands of dollars a year in spoiled foods. There are several things you can do to solve that problem:
- Lightly butter the exposed side of a cheese block, wrap the block in waxed paper and put it in a plastic bag.

- Puncture the plastic bags in which you bring home produce to avoid trapping moisture that causes spoilage.
- Freeze fruits and veggies that you will not use quickly
- Wrap the crown of a bunch of bananas with plastic wrap. This slows the release of ethylene gas, which causes ripening.
- Bundle herbs and keep them in a vase or glass of water rather than the refrigerator and trim the stems.
- Store counter items away from windows; sunlight causes faster ripening.
- Wrap lettuce, broccoli, and celery in aluminum foil before refrigerating them.
- Keep mushrooms in paper bags, not plastic.
- Store tomatoes upside (stem side) down on the counter.
More tricks for making groceries last longer can be found here.
Completely False Famous Predictions
- “The Americans have need of the telephone, but we do not. We have plenty of messenger boys.” —Sir William Preece, Chief Engineer, British Post Office, 1878
- “It’ll be gone by June.” —Variety Magazine on Rock ’n Roll, 1955
- “And for the tourist who really wants to get away from it all, safaris in Vietnam.” —Newsweek, predicting popular holidays for the late 1960s
- “When the Paris Exhibition [of 1878] closes, electric light will close with it and no more will be heard of it.” —Oxford professor Erasmus Wilson
- “A rocket will never be able to leave the Earth’s atmosphere.” —New York Times, 1936

Last Month’s Brain Teaser
You’re standing in a hallway with three light switches on the wall, each of which turns on a different lamp inside a closed room. You can’t see inside the room, and you can’t open the door except to enter the room. You can enter the room only once, and when you do, all the lamps must be turned off. How can you tell which switch turns on which lamp?
Answer: Turn on the right switch and leave it on for two minutes. After two minutes, turn
on the middle switch and leave it on for one minute. When that minute is up, turn off both switches and enter the room. One light bulb will be hot (1st switch) and one will be warm (2nd switch). The cold bulb will correspond to the switch you didn’t turn on.
Winner: BOB member Jere Christner is the April brain teaser winner. Living in rural Sitka, AK, Jere and his family are far from any major health facilities; the mainland is over 60 miles east. So, while visiting their daughter in Oregon in 2013, Jere made an appointment for a physical. During the exam, his doctor detected a lump in his prostate and ordered a biopsy. The results indicated that Jere had prostate cancer. “My urologist discussed treatment options with my wife and me, but proton therapy was never mentioned,” Jere said.
Shortly thereafter, Jere was at a party and ran into an old co-worker. “I told him I’d been diagnosed with prostate cancer and he told me another co-worker had just returned from southern California after getting proton treatment for prostate cancer and he was doing great,” Jere said. He later contacted his old colleague and heard about his treatment experience firsthand. “That conversation was the answer to my prayers,” Jere said.
Jere went on to have proton treatment in early 2014 at LLUCC. Today he’s healthy and feeling well. He talks about proton therapy to the people in his community and says three of them have gone to LLUCC for treatment.
Thank you for spreading the word and educating others about proton therapy, Jere. And congratulations on winning last month’s brain teaser! Your signed copy of Bob Marckini’s book is in the mail.
New Brain Teaser
What years from the 1900s and 1800s are the same year when read upside down?
Hint: This is a lot easier to solve than it looks.
Send your answer to [email protected] for a chance to win a signed copy of Bob Marckini’s book, You Can Beat Prostate Cancer.
Glorious Insults
These classics are from an era before the English language got boiled down to four-letter words.
- “He had delusions of adequacy.” —Walter Kerr
- “He has all the virtues I dislike and none of the vices I admire.” —Winston Churchill
- “I have never killed a man, but I have read many obituaries with great pleasure.” —Clarence Darrow
- “He has never been known to use a word that might send a reader to the dictionary.” —William Faulkner (about Ernest Hemingway)
- “Thank you for sending me a copy of your book; I’ll waste no time reading it.” —Moses Hadas
- “I didn’t attend the funeral, but I sent a nice letter saying I approved of it.” —Mark Twain
- “He has no enemies, but is intensely disliked by his friends.” —Oscar Wilde
- “I am enclosing two tickets to the first night of my new play; bring a friend, if you have one.” —George Bernard Shaw to Winston Churchill … “Cannot possibly attend first night, will attend second … if there is one.” —Winston Churchill, in response
- “He is a self-made man and worships his creator.” —John Bright
- “Some cause happiness wherever they go; others, whenever they go.” —Oscar Wilde
- “I’ve had a perfectly wonderful evening. But I’m afraid this wasn’t it." —Groucho Marx
- “He has Van Gogh’s ear for music.” —Billy Wilder
- “His mother should have thrown him away and kept the stork.” —Mae West
Golf Stories
Phil: A gushy reporter told Phil Mickelson, “You’re spectacular; your name is synonymous with the game of ‘golf.’ You really know your way around the course. What’s your secret?” Mickelson replied, “The holes are numbered.”
Strategy: A young man and a priest are playing together. At a short par-3 the priest asks, “What are you going to use on this hole, my son?” The young man says, “An 8-iron, Father, how about you?” The priest says, “I’m going to hit a soft seven and pray.” The young man hits his 8-iron and puts the ball on the green. The priest tops his 7-iron and dribbles the ball out a few yards. The young man says, “I don’t know about you, Father, but in my church, when we pray, we keep our head down.”
Perspective: A golfer teed up his ball on the first tee, took a mighty swing and hit his ball into a clump of trees. He found his ball and saw an opening between two trees he thought he could hit through. Taking out his 3-wood, he took a mighty swing. The ball hit a tree, bounced back, hit him in the forehead and killed him. As he approached the gates of heaven, St. Peter asked, “Are you a good golfer?” The man replied, “Got here in two, didn’t I?”
Quote of the Month:
“To get something done, a committee should consist of no more than three people, two of whom are absent.” — Robert Copland

Small Act of Kindness Saves the Day Source
Come with me to a third grade classroom … There’s a 9-year-old kid sitting at his desk. All of a sudden, there’s a puddle between his feet and the front of his pants are wet. He thinks his heart is going to stop because he can’t possibly imagine how this has happened. It’s never happened before, and he knows that when the boys find out he’ll never hear the end of it. When the girls find out, they’ll never speak to him again.
The boy believes his heart is going to stop; he puts his head down and prays this prayer: “Dear God, this is an emergency! I need help now! Five minutes from now I’m dead meat!” He looks up from his prayer and sees the teacher coming toward him with a look in her eyes that says he’s been discovered.
As the teacher gets closer, a classmate named Susie is carrying a goldfish bowl filled with water. Susie trips in front of the teacher and inexplicably dumps the bowl of water in the boy’s lap. The boy pretends to be angry, but all the while he’s saying to himself, “Thank you, Lord! Thank you, Lord!”
Now all of a sudden, instead of being the object of ridicule, the boy is the object of sympathy. The teacher rushes him downstairs and gives him gym shorts to put on while his pants dry out. All the other children are on their hands and knees cleaning up around his desk. The sympathy is wonderful. But as life would have it, the ridicule that should’ve been his has been transferred to someone else—Susie.
She tries to help, but they tell her to get out. “You’ve done enough, you klutz!”
Finally, at the end of the day, as the kids are waiting for the bus, the boy walks over to Susie and whispers, “You did that on purpose, didn’t you?” Susie whispers back, “I wet my pants once too.”
Low PSAs to all,
Bob Marckini and Deb Hickey
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
NO MEDICAL ADVICE: Material appearing here represents opinions offered by non-medically-trained laypersons. Comments shown here should NEVER be interpreted as specific medical advice and must be used only as background information when consulting with a qualified medical professional.