 Dear Members:
Dear Members:
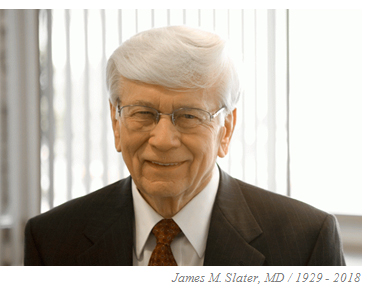
It is with deep sadness that we announce the passing of Dr. James Slater, the pioneer of hospital-based proton therapy. Dr. Slater was just a week away from celebrating his 90th birthday when he passed away at his home in California on the day after Christmas.
I first met Dr. James Slater when I was in treatment at the Loma Linda Proton Treatment Center in October 2000. Those who are aware of my story know that I pulled out all the stops to find the best treatment in the world for my prostate cancer. I had ruled out surgery because of my brother’s experience with that option. But there were so many non-surgical options, and the more I researched the more confused I became … until I discovered proton therapy. And the name that kept popping up in my research 20 years ago was “Dr. James M. Slater.” The more I studied the proton option, the more convinced I was that this was the treatment for me. And the more I learned about this incredible man, the more I was in awe of him. He became my hero even before I started treatment.
It wasn’t until a few years later that I learned about the extraordinary challenges and obstacles he faced from project conception, to funding, to team building, to solving insurmountable technological problems and even personal and political resistance along the way. The whole process began when Dr. Slater was deeply troubled by the collateral damage caused by the conventional radiation he was treating patients with in his early career. As a physicist and oncologist, he knew there had to be a better way to treat patients.
One by one he overcame all the obstacles in his journey, and in 1990 the first hospital-based proton treatment center opened. Since then more than 20,000 patients have been treated at Loma Linda, not to mention tens of thousands of others treated at some of the other 28 proton centers that followed in the U.S. as a result of his pioneering efforts.
Early in my treatment, I met my hero, Dr. Slater, in the hallway at the treatment center. I remember boldly walking up to him, introducing myself, and saying, “Dr. Slater, I’m so honored to meet you. I’ve researched all the treatment options, interviewed dozens of patients, and read everything I could find about proton therapy. And everywhere I looked I saw your name. Thank you, Dr. Slater, for what you have done for me and for countless other cancer patients around the world.”
I’ll never forget his answer. He smiled, thanked me for the kind words and said, “Call me Jim.” Imagine being on a first-name basis with the pioneer, the “guru” of proton therapy! That tells you a lot about the humility and humanity of this great man. From that point on, I called him “Jim.”
I served on the Advisory Council at Loma Linda for about 10 years along with several other BOB members. Dr. James Slater would routinely stop in at our semi-annual meetings to tell us about his passion: the basic and clinical proton therapy research under way at the proton center. I loved his presentations and admired the excitement, energy and optimism that came across when he and Dr. Jerry Slater spoke about new ways to use the “intelligent” proton particle to cure cancer and other diseases. There were always important projects sitting on the shelf waiting for funding to move forward.
 Golfing great Ken Venturi also served on the Advisory Council. Ken and Dr. Slater became close friends after Dr. Slater helped Ken’s mother with a health issue, and later treated Ken with protons for prostate cancer. When Dr. Slater asked Ken for help raising money for proton research, Venturi jumped in with both feet. Once a year, in May, he began hosting the Ken Venturi Proton Charity Golf Tournament at the beautiful Morningside Golf Club in Rancho Mirage, CA. I attended that event about 10 times. Millions of dollars have been raised for proton research thanks to Ken’s efforts and that thrilled Dr. Slater. It was at that golf tournament that I heard Venturi say on more than one occasion, “The world will not remember you for what you take with you, but for what you leave behind.” He certainly practiced what he preached.
Golfing great Ken Venturi also served on the Advisory Council. Ken and Dr. Slater became close friends after Dr. Slater helped Ken’s mother with a health issue, and later treated Ken with protons for prostate cancer. When Dr. Slater asked Ken for help raising money for proton research, Venturi jumped in with both feet. Once a year, in May, he began hosting the Ken Venturi Proton Charity Golf Tournament at the beautiful Morningside Golf Club in Rancho Mirage, CA. I attended that event about 10 times. Millions of dollars have been raised for proton research thanks to Ken’s efforts and that thrilled Dr. Slater. It was at that golf tournament that I heard Venturi say on more than one occasion, “The world will not remember you for what you take with you, but for what you leave behind.” He certainly practiced what he preached.
Quoting Dr. Richard Hart, president of Loma Linda University Health, “Dr. Slater will be memorialized by his development of proton therapy, but I will remember him even more as the consummate gentleman, always ready to listen and assist faculty and staff in pursuit of their dreams. His gentle spirit and deference to others made him a natural leader on our campus.”
One way we can honor this great man’s legacy is to make a gift to support his beloved proton therapy research efforts. Tribute gifts may be made on this memorial page.
Read the Loma Linda University Health press release.

I will surely miss my friend, Jim.
Bill Preston is a long-time friend of Dr. James Slater, and someone I’ve known for many years. He’s also a gifted writer. Very few people knew Jim better than Bill. Bill recently honored me by asking me to review the draft of a book he has written about Dr. Slater’s proton journey. It’s an extraordinary work that I am thoroughly enjoying. I asked Bill if he would write the featured article about Dr. James Slater for this month’s BOB Tales, special edition. I’m sure our members will learn much about this great man from Bill’s reflections.
As always, we welcome and appreciate your feedback on our newsletter. Just send an email to Deb Hickey at [email protected].
Bob Marckini
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
In this Issue:
- Hypo-fractionated Radiation Therapy Better for Intermediate Risk Prostate Cancer?
- Inflammatory Bowel Disease Linked to Prostate Cancer
- Proton Breast Cancer Benefits—Is There a Prostate Cancer Parallel?
- Complementary Therapies for Prostate Cancer
- YouTube—a Good Source for Misleading Information
- NAPT Launches New Website
- Preserving Your Vision Through a Balanced Diet
- Men Die Younger than Women—for Reasons that Are Preventable

Recalling Dr. Slater
By William Preston, EdD
James M. Slater, MD, FACR, died at his home in Rancho Mirage, CA, on Dec. 26, 2018. He was just a few days shy of his 90th birthday. Many members of the BOB knew him personally, and many more know of him as the inspiration, creator, and driving force behind the proton treatment and research center at Loma Linda University in California, a facility that has borne his name since 2007. To say that he will be missed by members of the BOB, especially by those who knew him personally, is probably a gross understatement.
 As a physician, Dr. Slater’s overarching quality was compassion. This sprang naturally from the man; he cared, and cared deeply. Lending a helping hand was as natural to him as breathing. In fact, in one discussion about solving problems, of whatever kind, he said that before anything else—recognizing a problem, formulating solutions, and implementing those solutions—one had to want to solve the problem; one had to care.
As a physician, Dr. Slater’s overarching quality was compassion. This sprang naturally from the man; he cared, and cared deeply. Lending a helping hand was as natural to him as breathing. In fact, in one discussion about solving problems, of whatever kind, he said that before anything else—recognizing a problem, formulating solutions, and implementing those solutions—one had to want to solve the problem; one had to care.
The great problem that Dr. Slater wanted to solve as a radiation oncologist was the suffering that cancer patients experienced, not only from the disease, but also from its treatment. When Dr. Slater began practicing radiation therapy in the mid-1960s, the latter was a significant concern. He was appalled and distressed at the side effects that radiation therapy could cause, effects that were sometimes so severe that treatments had to be suspended for a time, thus compromising the physician’s ability to treat the cancer successfully. He realized that the core reason for these side effects was exposure of too much normal tissue during radiation treatments. He was not willing to accept that this need be so; he thought there had to be better ways.
Not being willing to accept the status quo when something better might be possible was also characteristic of Dr. Slater. He developed that attitude when he was young. He once told me stories about working in logging camps in the Utah mountains when he was a teenager. When problems arose on the job sites, he said, people were expected to figure them out and solve them. “You didn’t just stand there,” he told me.
Dr. Slater understood that two things needed to happen to lessen the frequency and severity of side effects from radiation treatment: the actual extent of the cancer, and thus of the target volume needed to treat that cancer, needed to be defined as accurately as possible; and the ionizing radiation required to treat the cancer must conform to the target volume as precisely as possible. BOB members and others treated with protons are aware of Dr. Slater’s role in dealing with the second requirement, but many, perhaps, may not be aware of the leading role he played in dealing with the first. Yet, in some ways that role was even more important than his leadership in bringing proton therapy to the hospital environment.
Treatment planning, in essence, is writing the prescription for radiation treatment. The physician prescribes the total dose to be delivered, the volume to which it must be delivered, and the dose that must not be exceeded in nearby normal tissues. When Dr. Slater began his career as a radiation oncologist, treatment planning depended largely on diagnostic X-rays and the physician’s knowledge of cancer spread patterns; treatment fields often were larger than necessary, to avoid missing part of the spread pattern. While he was still a resident physician, Dr. Slater began working with a physicist at Loma Linda University to incorporate data from individual patients directly into a treatment-planning system. By 1971, shortly after Dr. Slater was recruited to Loma Linda to form a radiotherapy section, the new planning system was in operation. The first system used ultrasound data from patients; by the mid-1970s, when computed tomography (CT) scanning became available, Dr. Slater and his colleagues upgraded the system to use CT. This development was revolutionary at the time; one eminent British radiotherapist called it the “missing link” in radiation therapy. Dr. Slater’s achievement improved the accuracy and precision of radiotherapy plans and benefited all forms of radiotherapy, ultimately making feasible treatment methods, such as IMRT and proton therapy, that could exploit the precision of these plans. His pioneering planning system led to numerous national and international awards.
Important though improved treatment planning was, Dr. Slater knew that it addressed only part of the problem. There was still a need for a radiation-delivery system that could conform the dose to the target volume and avoid normal tissues as much as possible. He also knew that the photon—the elementary particle in X-rays—was not the particle to do it.
Before turning to medicine, Dr. Slater had studied to become a physicist. He therefore analyzed the problem from a physicist’s perspective, as well as a physician’s. He knew that the inherent characteristics of heavy-charged-particle beams, such as protons, gave them a great advantage over X-ray beams: the radiation oncologist could control them in three dimensions, whereas X-rays could be controlled in only two. This permitted the physician to conform the dose to the target volume without irradiating tissues downstream of the beam’s path, something not possible with X-rays, even sophisticated modalities such as IMRT. This brought them closer to what he called the “ideal beam.”
Dr. Slater was a visual thinker as well as a visionary. He was able to “see” the actions of particles as they interacted with the atoms within molecules, leading to the ionization process that could destroy cancer cells. He visualized the “ideal beam” as one that would deposit no radiation en route to the target volume, deposit the full dose in that volume, and irradiate nothing else. He said that such a beam did not exist and probably never would, but was a goal to aim for. After years of studying heavy-charged-particle beams of all kinds, he determined that the proton was the best particle for everyday radiation therapy because it permitted three-dimensional controllability yet would allow normal tissues that could not be excluded from the target to have a chance for self-repair. It wasn’t the “ideal beam” but was a clinically useful approximation that would allow for delivering needed doses while reducing side effects.
 Many BOB members are probably familiar with the rest of the story. Dr. Slater conceptualized and led a team of physicians, physicists, and health-care professionals to create and build the proton accelerator and treatment center at Loma Linda University. This facility was the first proton system in the world dedicated to treating patients. It, like the treatment-planning system, resulted in much national and international recognition for Dr. Slater and Loma Linda. More to the point, as far as Dr. Slater was concerned, it brought effective treatment, fewer side effects, and improved quality of life to thousands of patients. The James M. Slater, MD, Proton Treatment and Research Center continues to do so today, and that, I suspect, is what Dr. Slater would regard as his most important legacy.
Many BOB members are probably familiar with the rest of the story. Dr. Slater conceptualized and led a team of physicians, physicists, and health-care professionals to create and build the proton accelerator and treatment center at Loma Linda University. This facility was the first proton system in the world dedicated to treating patients. It, like the treatment-planning system, resulted in much national and international recognition for Dr. Slater and Loma Linda. More to the point, as far as Dr. Slater was concerned, it brought effective treatment, fewer side effects, and improved quality of life to thousands of patients. The James M. Slater, MD, Proton Treatment and Research Center continues to do so today, and that, I suspect, is what Dr. Slater would regard as his most important legacy.
The acclaim he received never changed Dr. Slater. He was a self-effacing, truly humble man who was genuinely uncomfortable with praise. His old friend, Ken Venturi, speaking at the dedication ceremony in 2007 at which the proton center was named for Dr. Slater, called him the “humblest man I’ve ever met.” For the rest of his life, Dr. Slater’s humility and concern for others remained the core of his practice as a physician and as a person.
That concern is still reflected in the care patients receive at the James M. Slater Center, as many BOB members can attest. In my opinion, that caring quality also traces back to Dr. Slater. In 1970, when he started what became the Department of Radiation Medicine, Dr. Slater instructed his staff to “treat every patient as it were your mother or father.”
In his lifetime Dr. Slater held many jobs and filled many positions, from working in logging camps in his youth to chairing a department in a major university. His variety of experiences enabled him to talk with anyone, anywhere, from day laborers to corporate presidents. He was always interested in what other people had to say, and he made every person he met feel as if he or she were welcome and appreciated. And he did it all with an appealing common touch.
I can relate one incident in that regard. My late first wife was one of Dr. Slater’s patients. During her treatments, her mother and father visited from New York state, and her father, an automobile mechanic, had a chance to talk with Dr. Slater about many things, including cars. Dr. Slater had much experience with car repair; his home, in fact, had what amounted to a repair shop, including a pit for working on automobile underbodies. Later, when her father talked with my wife and me about Dr. Slater, he said, “You’d never know that guy was a doctor.” I told Dr. Slater about that later, and he was genuinely pleased.
Another incident captures the combination of brilliance and humility that characterized Dr. Slater in all the years I knew him. The editor-in-chief of Loma Linda University School of Medicine’s Alumni Journal wrote an editorial about the proton treatment center; this was before the facility opened, but was nearing completion. He sent the editorial to Dr. Slater’s office for fact-checking, and Dr. Slater asked me to review it. It seemed fine to me, but I always made sure that Dr. Slater read documents too, in case I missed something. In this case, I did. The editor had praised Dr. Slater’s work, and somewhere in the editorial he equated Dr. Slater’s accomplishments with those of some of the great scientists of the past, including Albert Einstein. I can still see Dr. Slater asking his assistant to get the editor on the phone. I was in the room when Dr. Slater talked with him. I couldn’t hear what the editor was saying, but at some point he must have said something like, “You’re accomplishing something great.” Whatever it was, I can still see and hear Dr. Slater replying, “But not like those guys.”
In my opinion, James M. Slater was indeed like those guys. He was more than that. He was a good and kind man who did great things and did so because he cared so much about his fellows. He also was willing to do something, to not “just stand there” when problems needed to be solved. And he was willing to try what had not been tried before. His great achievements remind me of a quote from George Bernard Shaw’s “Back to Methuselah,” Part 1: “You see things; and you say, ‘Why?’ But I dream things that never were; and I say, ‘Why not?’”

Hypo-fractionated Radiation Therapy Better for Intermediate Risk Prostate Cancer?
We’ve reported in the past about ongoing clinical research showing excellent disease control and quality-of-life results when using hypo-fractionated proton therapy to treat early stage prostate cancer. Two reports, favorable to hypo-fractionation for prostate cancer, were recently published.
Hypo-fractionation refers to reducing the number of treatments (fractions) while increasing the dosage per treatment. Instead of the standard 40 to 44 treatment protocol, the hypo-fractionation trials typically call for 20 to 26 treatments.
An article published in Targeted Oncology reported that new clinical guidelines on the use of external beam radiation therapy (EBRT) have been developed by a panel of experts representing the American Society of Clinical Oncology, the American Society for Radiation Oncology and the American Urological Association. These guidelines encourage the use of hypo-fractionated EBRT for localized prostate cancer, on the basis that shortening the course of treatment does not materially impact disease free survival or quality of life after treatment. They also pointed out in the article that there are significant benefits to the patient in terms of convenience and cost associated with the current, standard, longer-course of treatment.
New research using conventional radiation, suggests that hypo-fractionation might even be the preferred protocol for treating intermediate- risk prostate cancer.
In this article, HRT refers to hypo-fractionated radiation therapy, and CRT refers to conventionally fractionated high-dose external beam radiation therapy.
Researchers at Brigham and Woman’s Hospital in Boston performed a systematic review and meta-analysis, pooling available data to determine if an improved risk of recurrence could be demonstrated using HRT vs. CRT while also evaluating the impact on bladder and rectal function. The HRT protocol was one-month duration, while the CRT was the standard two-month treatment plan. The study was published in European Urology Focus, and concluded the following:
“Our results provide evidence for clinicians to consider HRT as compared with CRT as a preferred radiation treatment in men with intermediate-risk prostate cancer and at low risk of other complications,” stated Trevor Royce, MD, MPH, radiation oncologist at Brigham and Women’s Hospital and first author of the study.
“Treatment with a shorter course of radiation and higher doses over fewer days may be the preferred approach in appropriately selected patients with localized prostate cancer, reducing treatment time and cost to the patient, and increasing patient convenience and access to treatment.”
The research involved three randomized studies involving more than 5,000 men, most of whom had intermediate-risk prostate cancer. No significant difference was found in overall survival rate between HRT and CRT, but researchers believe there could be an overall long-term survival benefit for those who had HRT. However, there did appear to be an increase in late bladder and urethra toxicities in the HRT group, which researchers believe could be mitigated by carefully choosing men who are not at risk for sustaining these side effects, according to Anthony D’Amico, MD, PhD, Chief, Genitourinary Radiation Oncology at Brigham and Woman’s Hospital and senior author of the study.
Previous HRT/CRT studies have also shown that the risk of recurrence may be lower with HRT treated patients than those treated using the standard CRT protocol.
Inflammatory Bowel Disease Linked to Prostate Cancer
According to a new 20-year study, men with inflammatory bowel disease are four to five times more likely to be diagnosed with prostate cancer. The report, from Northwestern Medicine, is the first to show men with IBD have higher than average PSA values; and this group also has a significantly higher risk of potentially dangerous prostate cancer.
IBD, a chronic condition that includes Crohn’s disease and ulcerative colitis, affects nearly one million men in the U.S. The study’s lead author, Dr. Shilajit Kundu, suggests men with IBD be screened more carefully for prostate cancer than men without the disease.
Proton Breast Cancer Benefits—Is There a Prostate Cancer Parallel?
Kimberly Corbin, MD, a radiation oncologist at Mayo Clinic reported that clear advantages have been seen in treating breast cancer patients with proton vs. conventional X-ray radiation. Because proton therapy is more precise, and spares surrounding healthy tissue, Dr. Corbin feels that it is the optimal approach for treating breast cancer, particularly in risky patients. Her study was reported in OncLive on Dec. 19, 2018.
Clinical trials are under way evaluating the safety and efficacy of proton therapy following lumpectomy in patients with early-stage breast cancer. Proton beam therapy is started two to four weeks following surgical excision and lasting two weeks. The target volume is the site of the lumpectomy with an additional margin.
 Post lumpectomy radiation has been shown to reduce cancer recurrence and improve survival. However, in the past, radiation exposure to the chest wall, lung and heart have produced radiation-induced complications. This is particularly true when treating women with cancers in their left breast. Because of the Bragg peak, the proton radiation dose drops to zero after treating the target volume. This spares healthy organs and tissues, such as the heart and lungs, beyond the target.
Post lumpectomy radiation has been shown to reduce cancer recurrence and improve survival. However, in the past, radiation exposure to the chest wall, lung and heart have produced radiation-induced complications. This is particularly true when treating women with cancers in their left breast. Because of the Bragg peak, the proton radiation dose drops to zero after treating the target volume. This spares healthy organs and tissues, such as the heart and lungs, beyond the target.
Complementary Therapies for Prostate Cancer
In the past, complementary therapies, or non-standard treatments, were described as alternative or even irrational by many in the medical field. Over the years, therapies such as acupuncture, meditation, and even prayer have become more widely accepted and often integrated into patient-treatment programs to help ease anxiety and lessen or even eradicate adverse side effects.
Treating the Whole Patient
BOB members treated at Loma Linda are familiar with their emphasis on whole person care. They treat patients “body, mind, and spirit”—physically, emotionally, and spiritually—with the goal of maintaining a positive, upbeat atmosphere and building a spirit that will keep patients connected and support healing. Other proton centers have also adopted complementary therapy programs.
Exercise: We’ve written about the importance of exercise in our BOB Tales newsletter for years. Hundreds of studies have shown real, tangible benefits of exercise for patients with a variety of cancers and at different stages. In one analysis of 28 trials involving over 1,000 participants with advanced cancers (including prostate) an exercise program during treatment was associated with significantly improved physical function, energy levels, weight/BMI, psychosocial function, sleep quality, and overall quality of life.
Mindfulness: Mindfulness is the practice of focusing on your thoughts, emotions, and feelings in the present moment with acceptance and without judgment. It’s known to reduce stress, boost energy, and improve well-being.
Researchers have found that mindfulness-based therapy, including yoga, meditation exercises, and other psychological techniques can help cancer patients direct their attention away from their worries causing them to become less anxious.
Spirituality: According to the US Centers for Disease Control and Prevention (CDC), 69 percent of cancer patients say they pray for their health. A study published in Cancer, a peer-reviewed journal of the American Cancer Society, suggests a link between religious or spiritual beliefs and better physical health reported among patients with cancer.
Vitamins and Supplements
Many cancer patients complement their treatment by taking vitamins and supplements. A recent study of men with prostate cancer revealed that 65 percent used herbal remedies and nutritional supplements during their conventional treatment. Common nutritional therapies include antioxidants, such as beta-carotene, lycopene, and vitamins A, C, and E. Patients with prostate cancer have commonly used antioxidants for both prevention and treatment.
Some nutritional supplements as complementary cancer therapies have been evaluated by experts and found to be safe and effective. Others have been found ineffective, and some even harmful.
It’s important to discuss any complementary therapies—especially dietary supplements—with your doctor no matter how safe you think they are. Note: Supplements don’t have to be approved by the federal government before being sold to the public and a prescription is not needed to buy them.
 YouTube—a Good Source for Misleading Information
YouTube—a Good Source for Misleading Information
You may or may not be surprised that many people go to social media—particularly YouTube—to get medical advice. According to researchers from New York University’s School of Medicine and its Perlmutter Cancer Center, that’s a bad idea. In a recent article, published in European Urology, they evaluated YouTube videos specifically created to educate people about prostate cancer.
What exactly is YouTube?
YouTube is a website designed to share videos. Users can upload, watch, like, rate, share, and comment on videos. When it was created in 2005, YouTube was intended for people to post and share original video content. Since then it’s become a place where users can view television clips, music videos, film trailers, tutorials on just about anything, news casts, and even presidential debates.
Users Beware
YouTube is a great place to discover new things and be entertained; however it has its downsides—especially when it comes to learning about your health. Numerous studies have examined the value of information on YouTube about various health topics and many have revealed poor quality, biased, and/or commercial content, which might have dangerous consequences for users.
If you perform a search on “prostate cancer” on YouTube, you could probably scroll through the results all day—600,000 results to be exact. And if you look closely, you’ll see that many of the videos have more than 100,000 views, illustrating YouTube’s popularity as a source for information about prostate cancer. The problem is, only a few official prostate cancer studies have reported results in YouTube videos.
There have been a number of studies on the value of YouTube content related to prostate cancer. A study of 51 videos performed in 2008 reported that 73 percent contained fair to poor information and 69 percent were biased toward screening or treatment. A more recent study found that of 150-viewed videos assessed, 77 percent were misleading in some significant way—either because they had factual errors or biased content. Of that biased content, 75 percent of the videos the researchers assessed laid out benefits of various treatment options, but only 53 percent mentioned any potential harms and side effects. Nineteen percent of the videos recommended unproven alternative therapies.
The extent to which the public receives biased, incorrect, or commercial information about prostate cancer through videos and/or interactions on YouTube that could affect decision-making is unknown.
NAPT Launches New Website
 The National Association for Proton Therapy (NAPT) website receives over 15,000 unique visits per month. For well over 20 years, the site has served cancer patients and the oncology community as the main educational resource for proton therapy across the country and the world. In order to continue to serve as the most informative proton therapy website available, on Nov. 12, NAPT launched a new site designed to work on computers, tablets, and smart phones.
The National Association for Proton Therapy (NAPT) website receives over 15,000 unique visits per month. For well over 20 years, the site has served cancer patients and the oncology community as the main educational resource for proton therapy across the country and the world. In order to continue to serve as the most informative proton therapy website available, on Nov. 12, NAPT launched a new site designed to work on computers, tablets, and smart phones.
The website, which is ADA compliant, provides visitors with quick-and-easy access to information about proton therapy. It includes an interactive map with links to educational videos as well as a monitored patient forum. You can find information on NAPT’s board of directors, Lifetime Achievement Award winners, and member blog posts. The newly expanded patient- resources section includes a media gallery and links to books on proton therapy. A “Protons for Kids” section includes videos, webinars, and a downloadable Proton Man comic book.
NAPT Executive Director Scott Warwick tells us they’ve received a lot of positive feedback from patients, members, and other stakeholders about the new site. He hopes others, including our members, will review it and recommend it to others who have an interest in proton therapy.

We’ve been producing BOB Tales newsletters monthly for 18 years. During this time there have been important articles that many new members haven’t seen, and some long-time members may have forgotten. So, we periodically re-run articles from past newsletters. The following is from May 2005.
Preserving Your Vision through a Balanced Diet
An article recently appeared in the San Bernardino (CA) Sun titled, “Preserving Your Vision through a Balanced Diet.” It was written by Dr. Howard Gimbel, a prominent physician in Canada and the U.S., Professor and Chairman of the Ophthalmology Department at Loma Linda School of Medicine. I had the pleasure of meeting Dr. Gimbel on a recent visit to Loma Linda.
Dr. Gimbel’s article was a real eye-opener (pun intended). Here are some of the things I learned from the article and my conversation with him: Most aging eye problems result from the slow deterioration of body cells, the biological equivalent of “rusting away.” But nutrients in select foods can counteract oxidation and slow down the aging effects.
Foods We Should Eat Most Often: According to Dr. Gimbel, we should eat mostly whole grains and grain products (whole grain breads, cereals, pasta, brown and wild rice, spelt, kamut, oats, barley, quinoa and other grain products).
Foods We Should Eat A Lot: Dr. Gimbel recommends a lot of fruits and vegetables—the full spectrum of colors, especially dark green leafy vegetables such as spinach, kale and broccoli. “These may reduce your chances of developing macular degeneration by more than 80 percent.” Also, by eating five to seven servings of fruits and vegetables each day, you greatly reduce your chances of developing cataracts, glaucoma, and other problems.
Foods We Should Eat Sometimes: Dr. Gimbel suggests eating protein-rich foods. Beans, lentils, chickpeas, split and black-eyed peas, and other legumes provide vitamin B and fiber. Nuts provide protein, vitamin E, and zinc. Eating unsalted nuts can keep your eyes healthy and reduce heart disease by 50 percent.
Foods to Eat Sparingly: Fats and sweets—foods high in saturated fat—aren’t good for your body. If you drink milk, Dr. Gimbel recommends skim or low fat. Women can get their calcium from oranges, figs, almonds, tofu, and beans.
Nuts, seeds, olives, and avocados provide certain oils that are essential for good nutrition. Steaming, boiling, or baking are all suggested ways to prepare food. Use small amounts of vegetable oil and no animal fats. Dr. Gimbel also recommends drinking at least eight glasses of water a day.
One final point: A diet high in fat and cholesterol can more than double your chances of developing retinal problems. “That which hurts the heart also hurts the eyes,” says Dr. Gimbel.

Conversations with Contributors
Every month, we receive a list of members who have made contributions to the Robert Marckini Chair for Proton Therapy Research or Loma Linda University Health’s Vision 2020 campaign, though we don’t know the exact amounts given. We make every attempt to get in touch with everyone on these lists to thank them for their generosity. We are in the midst of calling those who made 2018 year-end contributions and we thought we’d share a few quotes from our conversations.
I never answer my phone when I don’t recognize a number. But when I heard “Brotherhood of the Balloon” on the recording, I got excited … We donate every year to proton research and the Marckini Chair because I’m thankful to have been treated with protons back in 2001 at Loma Linda. At 84, I’m feeling fine and doing well … By the way, I had dinner with Bob Marckini many years ago somewhere in Seattle and I have very fond memories … Please send him my regards. And thank you for the fantastic job you do with the BOB. —BOB Member, Gig Harbor, WA
If we could have afforded to do so, we would’ve moved to Loma Linda … During our stay, I volunteered at the Children’s Hospital … At a Christmas party, I got to be Santa Claus’ assistant … We have friends all over the country due to my husband’s treatment… —BOB Member Spouse, Cottonwood, AZ
I look forward to the newsletter every month. Thank you for the effort you put into writing it—it’s clear to me that you don’t sleep much. —BOB Member, Erie, PA
How to Give to Proton Therapy Research
- Donate Online: Visit the LLUCC website.
- Send a Check: Make it out to “LLUCC Proton” with “Marckini Chair” on the memo line and send to: LLUH, Office of Philanthropy, P.O. Box 2000, Loma Linda, CA 92354.
- Make a Call: Contact Regina Joseph at 909-558-5010.
How to Give to Vision 2020
- Donate online: Visit the LLUH website.
- Send a check: Make it out to: “LLUH Vision 2020.” Mail to: LLUH, Office of Philanthropy, P.O. Box 2000, Loma Linda, CA 92354.
- Make a call: Call 909-651-2020.
How to Make a Future Gift
- Make a future gift: Contact Todd Mekelburg at the Office of Planned Giving at Loma Linda University Health at 909-558-5376 or [email protected].
2019 National Proton Conference: Miami, FL
The National Association for Proton Therapy (NAPT) is the voice of the proton community. The organization provides education and awareness for the public, professional, and governmental communities. Join NAPT for the 2019 National Proton Conference March 24 - 27, 2019, at The Biltmore Miami-Coral Gables in Coral Gables, FL. Attendees will include physicians, nurses, therapists, patients, proton therapy directors, and managers.

Men Die Younger than Women—for Reasons that Are Preventable
The Movember Foundation reports that men die an average of six years younger than women—and for reasons that are largely preventable. This was recently reported on KVUE ABC.
Men’s top health issues, according to the article, are heart disease, prostate cancer, and depression. Women have health issues too. But one significant difference between men and women is that men are more likely to put off going to the doctor for routine physicals or for screening tests. Some speculate it’s because their masculinity might be compromised by seeking medical attention, so they tend to keep health issues to themselves.
Most women are diligent about scheduling annual physicals and having screening tests, such as pap smears and mammograms. Men, on the other hand, are less conscientious about routine testing.
We regularly hear from men who are inquiring about proton therapy for prostate cancer. When we ask about PSA history, we are often shocked at the answer. Last month a gentleman told us, “I have no prior PSA readings.” Another inquirer, with a PSA of 9.2, when asked the same question said, “Last time I had a PSA test was about six years ago and it was normal.” As we all know, prostate cancer is curable if found early. It’s surprising how many men are not being screened for prostate cancer.
In Bob’s book, he wrote about one extreme example of this:
The wife of a recently diagnosed prostate cancer patient called. She was doing research on treatment options for her husband and wanted to learn all she could about proton treatment from me. I asked my typical opening questions: What is your husband’s age, his PSA, his Gleason Score, and is there a palpable tumor by DRE?
She told me he was 56 years old, his PSA was 37, his Gleason score was 10, and he has large tumors in both lobes of his prostate. My “knee-jerk” reaction was, “Surely this must have shown up in previous physical exams?” And she replied, “He’s never had any physical exams. We don’t believe in them. We prefer health food, meditation, and yoga to conventional western medicine.”
“Then how did you discover his cancer?” I asked. She replied, “He couldn’t urinate, so we went to the hospital emergency room where they discovered the tumors.”
Dr. Charles Osterberg is Chief of Urology at Dell Seton Medical Center at the University of Texas. He said in the article, “Men’s health needs to be discussed more openly in order to prevent men from developing undiagnosed issues, such as prostate cancer, which killed roughly 30,000 people last year.” He further stated, “It starts by having a good support system. So, having a spouse or a daughter or a son encourage their father-figure or their boyfriend, their husband, etc. to seek out care … Only when we have a good support system do we encourage men to seek out care and undergo routine screenings.”
The Movember movement is all about encouraging men to speak out about men’s health and create awareness about annual physicals and routine screening. It’s not just about prostate cancer awareness.
Series: “Make Vegetables Taste Good”
This is the 26th segment on a subject that’s consistent with our Anticancer series. We made it our mission to find recipes that make vegetables and other healthful foods taste delicious. And, we’ve tried them all!
Bob Marckini made this soup for Deb on her birthday this past October and Deb wouldn’t leave her parents’ house without a hand-written copy of the recipe. Do yourself a favor and make this for dinner tonight.
Bob Marckini’s Creamy Italian White Bean and Spinach Soup
Ingredients:
|
|
Directions:
In a large saucepan, heat oil over medium heat until hot. Add onion and celery and cook, stirring occasionally, until tender, about 7 minutes. Add garlic; cook about 30 seconds, stirring. Add beans, broth, water, pepper, salt and thyme. Heat to boiling over high heat. Reduce heat to low; simmer uncovered for 15 minutes.
Meanwhile, trim tough stems from spinach and discard.
With slotted spoon, remove about 2 cups bean-and-vegetable mixture from soup; set aside. Using an immersion blender, puree the remaining mixture of vegetables, beans and broth until smooth. If you don’t have an immersion blender, ladle the broth mixture into a blender to puree.
With the pureed soup in the saucepan, stir-in the reserved beans and vegetables. Heat to boiling, over high heat, stirring occasionally. Stir in the lemon and spinach, and immediately remove from heat. Let the soup sit for 15 minutes. Serve with grated parmesan cheese.
Feel free to experiment with the amount of beans, broth, and water.

“… I was given two years of life—
with the last six months living in extreme pain.”
A recent Amazon review titled, “Pass It On,” caught our attention. It’s well-written and genuine. Thank you, Niecie, for such a thorough and thoughtful review.
At the time of this writing, the book has nearly 380 reviews and it’s holding the No. 3 spot in Amazon on a search for “prostate cancer.” Eleven years after the publication date, this is astonishing. Again—
the book’s visibility in Amazon is proof that the content is still accurate
and valuable, and that readers are passionate about sharing it with others. Clearly that passion is leading to more and more people finding their way to proton therapy. THANK YOU, Amazon reviewers.
Following is Niecie’s five-star review:

Passing It On
In 2011 I was retired, healthy, and we finally had time to enjoy life. Then I was diagnosed with an aggressive form of prostate cancer. If I opted for no treatment, I was given two years of life—with the last six months living in extreme pain. My urologist gave me several options—robotic surgery, seeds, etc. But my wife and I had locked in on the two-year prognostication and our minds were not receiving much information after the first shock. Time was a critical factor and I was worrying, losing sleep and weight thinking about the upcoming surgery. I emailed an old golfing friend from the small town where we formerly lived who had prostate cancer years before to see what method of prevention he had chosen. He said he had chosen to go to Loma Linda, CA, for proton therapy, and was cancer free with no surgical intervention. He highly recommended them and advised reading this book, which I did. Reading this book was not only encouraging, it was uplifting. I was treated for prostate cancer using proton therapy at Loma Linda University Hospital, Loma Linda, CA, and have been cancer free and healthy since. My PSA has remained at 0.1. The “atmosphere” at the treatment center was positive—it was a 9-week treatment and my wife and I have many fond memories from the time we spent and the friends we met in the Loma Linda/Redlands area. If diagnosed with prostate cancer I strongly advise reading this book. It led to one of the best decisions I’ve ever made. —Niecie
We need your help.
Many medical professionals still aren’t informed about proton therapy and most mainstream media (and some doctors) discount proton therapy as a viable treatment option. We’re fighting daily for this to change. One way is through Bob’s book. Please help others find it by posting a review on Amazon and rating it from one to five stars.
Buy Bob's book online, in bulk, or in Spanish.
Online: Paperback: $19.00--•--Kindle: $7.99--•--NOOK Book: $9.99--•--Apple iBook: $9.99
In Bulk: Conctact us for a discount price list. Proceeds from book sales support proton therapy research through the Robert J. Marckini Endowed Chair at LLUCC.
In Spanish: Buy the print version or in eBook format.

Weather—Did You Know?
The weather is an intriguing natural phenomenon. Yet despite all of its wonder, we know very little about it. Following are 10 intriguing facts about weather. Next month, we’ll include another 10.
- Listening to the sound of crickets can give you an estimate of what the temperature is in Fahrenheit degrees. You can do this by counting the number of chirps you hear in 15 seconds and adding 37!
- During a hurricane, 76 percent of fatalities are caused by drowning.
- The highest temperature recorded in the U.S. occurred on July 10, 1913 in Death Valley. The official read was 134 degrees F, which is also the highest temperature recorded in the Western Hemisphere.
- The coldest temperature ever recorded was -128.6 degrees F at the Vostok Station, Antartica.
- In 1899, it was so cold the Mississippi River froze over its entire length.
- The biggest hailstones ever recorded fell on Bangladesh on April 14, 1986. They weighed up to 1kg (2.2 lbs) and killed 92 people.
- The greatest snowfall in a single storm was 189 inches at the Mount Shasta Ski Bowl in February 1959.
- The average lifespan of a tornado is less than 15 minutes.
- The U.S. uses an estimated 10 million tons of salt each year to melt ice on its roads.
- In 10 minutes, a hurricane releases more energy than all the world’s nuclear weapons combined.
Bizarre Sea Story—Is It True?
On Dec. 31, 1899, the passenger steamer SS Warrimoo was quietly knifing its way through the waters of the mid-Pacific on its way from Vancouver, British Columbia, Canada, to Sydney, Australia. The navigator had just finished working out a star fix and brought Captain John D. S. Phillips, the result. The SS Warrimoo’s position was 0º 31’ North Latitude and 179º 30’ West Longitude.
Captain Phillips asked, “Know what this means?” First Mate Payton broke in, “Yes—it means we’re only a few miles from the intersection of the equator and the International Date Line.”
 Captain Phillips decided to take full advantage of the opportunity to achieve the navigational freak of a lifetime, so he called his navigator to the bridge to check and double check the ship’s position.
Captain Phillips decided to take full advantage of the opportunity to achieve the navigational freak of a lifetime, so he called his navigator to the bridge to check and double check the ship’s position.
The captain then changed course slightly, so as to bear directly on his mark. Next, he adjusted the engine speed. The calm weather and clear night worked in his favor.
At the stroke of midnight, the SS Warrimoo lay on the equator at exactly the point where it crossed the International Date Line! The consequences of this bizarre position were many, as described below.
At this rare moment in time, these five things occurred:
- The date in the SS Warrimoo’s stern was 31 December 1899, New Year’s Eve.
- The date in the SS Warrimoo’s bow was 1 January 1900, New Year’s Day.
- The stern of the SS Warrimoo was in the Northern Hemisphere in the middle of winter.
- The bow of the SS Warrimoo was in the Southern Hemisphere in the middle of summer.
- Therefore, the SS Warrimoo was positioned in two different days, in two different months, in two different years, and in two different centuries, as well as in two different hemispheres, and in two different seasons!

Last Month’s Brain Teaser
Two boxers are in a match scheduled for 12 rounds (pure boxing only—no kicking, UFC takedowns, or anything else). One of the boxers gets knocked out after only six rounds, yet no man throws a punch. How is this possible?
Answer: Both boxers are female.
Winner: Our winner is BOB member Joe Estes of Emporia, KS. Joe was treated for his prostate cancer at the ProCure Proton Therapy Center in Oklahoma in 2010. Eight years later he’s healthy and feeling fine. “Proton therapy changed my life,” he says of his treatment. Joe was happy to be last month’s brain teaser winner because he’d given his copy of Bob’s book away. “I look forward to receiving this copy,” he said. “I hope to share it with someone else. Thank you to the BOB for all you do.”
Congratulations, Joe!
New Brain Teaser
This is an unusual paragraph. I'm curious as to just how quickly you can find out what is so unusual about it. It looks so ordinary and plain that you would think nothing is wrong with it. In fact, nothing is wrong with it! It is highly unusual, though. Study it and think about it, but you still may not find anything odd. But if you work at it a bit, you might find out. Try to do so without any coaching!
Send your answer to [email protected] for a chance to win a signed copy of Bob Marckini’s book, You Can Beat Prostate Cancer.
Silent Treatment
Mike and Joan were having some problems at home and were giving each other the silent treatment. But then Mike realized that he’d need his wife to wake him at 5:00 a.m. for an early morning drive with some pals to go golfing.
Not wanting to be the first to break the silence (and lose the “war”), he wrote on a piece of paper: “Please wake me at 5:00 a.m.”
The next morning, Mike woke up, only to discover it was 9:00 a.m. and his friends had left for the golf course without him. Furious, he was about to go and see why his wife hadn’t awakened him when he noticed a piece of paper by the bed. It read: “It’s 5:00 a.m. Wake up.”
Men simply are not equipped for these kinds of contests.
Phyllis Diller Humor
Phyllis Diller (1917 – 2012) was a stand-up comedian best known for her eccentric stage persona, her self-deprecating humor, her wild hair and clothes and her cackling laugh. Following are a few of her many humorous quotations:
- Housework can’t kill you, but why take a chance?
- Cleaning your house while your kids are still growing up is like shoveling the sidewalk before it stops snowing.
- The reason women don’t play football is because 11 of them would never wear the same outfit in public.
- Best way to get rid of kitchen odors: eat out.
- I want my children to have all the things I couldn’t afford. Then I want to move in with them.
- Any time three New Yorkers get into a cab without an argument, a bank has just been robbed.
- We spend the first 12 months of our children’s lives teaching them to walk and talk and the next 12 years telling them to sit down and shut up.
- We Californians are constantly accused of not having seasons, but we do—we have fire, flood, mud, and drought.
- You know you’re old if they have discontinued your blood type.
Quote of the Month:
“To err is human, but to really foul things up requires a computer.”
—Farmers Almanac, 1978

What it Means to be Poor
One day a father of a very wealthy family took his son on a trip to the country with the firm purpose of showing his son how poor people can be. They spent a couple of days and nights on the farm of what would be considered a very poor family.
On their return from their trip, the father asked his son, “How was the trip?”
“It was great, Dad.”
“Did you see how poor people can be?” the father asked.
“Oh, yeah,” said the son.
“So what did you learn?” asked the father.
The son answered, “I saw that we have one dog and they had four. We have a pool that reaches to the middle of our garden and they have a creek that has no end. We have imported lanterns in our garden and they have the stars at night. Our patio reaches to the front yard and they have the whole horizon. We have a small piece of land to live on and they have fields that go beyond our sight. We have servants who serve us, but they serve others. We buy our food, but they grow theirs. We have walls around our property to protect us; they have friends to protect them.”
The boy’s father was speechless. Then his son added, “Thanks, Dad, for showing me how poor we are.”
Too often, we forget what we have and concentrate on what we don’t have. One person’s worthless object is another’s prize possession. It’s all based on perspective. It makes you wonder what would happen if we all gave thanks for the bounty we have instead of worrying about wanting more. Take joy in all you have—especially your friends.
Low PSAs to all,
Bob Marckini and Deb Hickey
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
NO MEDICAL ADVICE: Material appearing here represents opinions offered by non-medically-trained laypersons. Comments shown here should NEVER be interpreted as specific medical advice and must be used only as background information when consulting with a qualified medical professional.