Dear Members:
Call me a softie, but there’s nothing I wouldn’t do for Sadie, our 11-pound Bichon Frise. Over the past 16 years, she’s always loved to be near “Daddy” and she also delights in looking out the window, so I did the only natural thing—I built a padded ramp in my office and a wooden frame to support a little bed on my desk next to the window. Now she can easily climb up and sit next to me any time she wants (which is just about all the time).
 Whenever I come home from running errands, Sadie’s in the window waiting patiently for me. She jumps for joy when I pull into the driveway (of course she also does this when I come in after taking out the trash).
Whenever I come home from running errands, Sadie’s in the window waiting patiently for me. She jumps for joy when I pull into the driveway (of course she also does this when I come in after taking out the trash).
We can learn a lot from our pets—intense loyalty, enduring devotion, and unconditional love. They don’t ask for much in return—food, a soft place to sleep, a scratch behind the ears, and some play time.
“Take Your Dog to Work Day” is June 24. I don’t think much about that, because I bring Sadie to work every day. But, some of you may want to do this—I know a lot of our members have special dogs in their lives. Tell us about them—maybe we’ll do a special “Members and Their Dogs” segment in an upcoming issue.
June is also the month of some pretty bizarre holidays including National Doughnut Day, Repeat Day (I said, “Repeat Day”), National Yo-Yo Day, and my favorite, Insurance Awareness Day. As we mentioned last month, we are quickly approaching the submission date of the full proposal for “A Prospective Comparative Study of Outcomes with Proton and Photon Radiation in Black and White Men.” The team, headed up by Dr. Nancy Mendenhall, Medical Director at University of Florida Health Proton Therapy Institute, is in the final stages of preparing a detailed, formal proposal requesting funding from the Patient Centered Outcomes Research Institute (PCORI). If the proposal is accepted, the study could resolve disagreements that restrict patients’ access to proton therapy, particularly with regard to private medical insurer’s coverage and reimbursement policies. Stay tuned.
We have another terrific BOB Tales this month. We reported back in 2011 that the United States Preventive Service Task Force (USPSTF) shook our world a few years ago when they strongly recommended against prostate cancer screening. They claimed it resulted in over-treating and was harming men who would otherwise have led normal lives without any prostate cancer symptoms. Our members and many in the medical community were outraged. We have since learned that the USPSTF is made up of, and led by people who know very little about prostate cancer. And with the rapidly increasing rate of aggressive prostate cancer diagnoses in the past few years, the USPSTF is beginning to change their position. We cover these developments in this month’s newsletter.
We also report this month on new developments in proton therapy, and some important projections from the National Proton Conference as to where proton therapy is going over the next five years. Exciting stuff!
Many of the articles we present in the BOB Tales are prompted by news stories and suggestions sent to us by our members. We encourage you to continue doing this as well as providing us with feedback on each issue.
We hope you enjoy the June issue.
Bob Marckini
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
In This Issue:
- USPSTF Changing Position on Prostate Cancer Screening
- Six Reasons Why Prostate Cancer Screening is Important
- Sleep and Prostate Cancer – the Connection
- Low-Dose Aspirin May Cut Prostate Cancer Risk
- The Future of Protons: What the Experts Said at the National Proton Conference
- Why We All May Want to Move to Arizona …
- Re-treating with the Proton Beam is Becoming a Reality
- Member’s Testosterone Level Way Off the Charts
- Need Volunteers for Two New Proton Patient Reference Lists
- Why is it not good if Agave Nectar, Panocha, Sweet Sorghum, and Treacle are in Your Food?
.jpg)
USPSTF Changing ("Somewhat") Position on Prostate Cancer Screening
We received an overwhelming number of emails from BOB members around the world when several media outlets reported the United States Preventive Service Task Force (USPSTF) was changing its position on prostate cancer screening. So we asked BOB member Dr. Pat Greany if he would distill these published articles for our readers. Pat is a retired USDA research entomolgist and courtesy professor at the University of Florida. Here is his analysis, which we feel covers the subject well.
Background on the USPSTF Position
In 2012 the USPSTF recommended against PSA-based screening for prostate cancer for men of all ages. The rationale was that reduced screening would lead to fewer men being over-diagnosed and over-treated, with potentially serious consequences including biopsy-related blood loss, infection, and treatment-related ED and incontinence. There was a huge outcry against this recommendation because prostate cancer experts—who actually take care of prostate cancer patients—anticipated this would lead to many men being diagnosed eventually, but at a much more advanced stage!
One of the most vocal experts protesting this recommendation is Dr. Patrick Walsh of Johns Hopkins University, who said this would set prostate cancer care back 25 years, to the pre-PSA days! The American Urological Association and many other groups also protested this recommendation. Dr. Charles “Snuffy” Myers, a world-class medical oncologist who focuses entirely on men with advanced stage prostate cancer, stated that the recommendation, “regrettably would be good for his business.”
Dr. Peter Scardino, Chief of Surgery at Memorial Sloan Kettering, indicates in an excellent video that rather than suppressing screening altogether, we should “test smarter.” He endorses the use of the Opko 4k Score as a follow-up test if there are indications such as an elevated PSA or abnormal DRE. This is a blood test that has been extensively tested and it is able to determine whether the PSA elevation is due to prostate cancer or another cause, and if cancer is present, how aggressive it is likely to be. He says use of this test could reduce the number of biopsies by 50 percent with few or no ill consequences.
If a biopsy is indicated, genomic tests such as the Oncotype Dx and Prolaris can be used for biopsy specimens to determine whether a tumor is sufficiently aggressive to warrant treatment.
The Department of Defense Prostate Cancer Research Program (PCRP) is interested in research dealing with use of biomarkers to improve prostate cancer diagnosis and treatment and has spent millions on this over the years. Surely the USPSTF must have been aware of research on the development of better tools to reduce over-diagnosis and over-treatment. Rather than denying prostate cancer screening, they should have encouraged and supported the development of improved tests, such as the Opko 4k Score.
The Makeup of the USPSTF and the Leader's Qualifications (Or Lack Thereof)
Amazingly, according to the 2012 USPSTF statement, there were no urologists on their panel! Here’s an excerpt from this statement:
17. Were any urologists involved in the development of this recommendation?
The Task Force is made up of 16 volunteer members who are experts in prevention and evidence based medicine. Almost all currently care for primary-care patients as family physicians, general internal medicine physicians, nurses, obstetrician-gynecologists, occupational medicine physicians, and pediatricians.
The Task Force does not have any members who are urologists (emphasis added). However, several are respected cancer researchers. In this case, the Task Force evaluated evidence on whether primary-care practitioners should recommend PSA screening—a decision the Task Force members are expertly qualified to make. Expert urologists provided peer review of the systematic evidence review for the Task Force.
The makeup of the USPSTF panel similarly is deficient in its composition, with no urologists and no prostate cancer specialists included. The chairman of the Task Force, Dr. Kirsten Bibbins-Domingo, has an impressive background, but not in prostate cancer care. Her focus has been on cardiovascular epidemiology and “health disparities” in her personal research. She was recently interviewed on PBS in regard to the partial reversal of the 2012 panel’s recommendations.
Her explanation of the change in position leaves a lot to be desired, as it simply recommends that 55-69-year-old men speak with their doctors about the advisability of getting a PSA test. They still recommend against PSA testing for men 70 and over! The 2017 recommendation draft statement is available here. Astonishingly, she makes no mention of advances in use of biomarkers and genomic testing that can greatly reduce the chance of over-diagnosis and overtreatment.
Increase in Aggressive Prostate Cancer as well as Prostate Cancer Deaths
 As anticipated by prostate cancer specialists, there has been a significant increase in the number of older men reported to have distant metastases at diagnosis, as reported in JAMA Oncology last year. A good synopsis of the report is provided here. According to the article, “The incidence of metastatic prostate cancer in older men is rising after reaching an all-time low in 2011 … The findings suggest a correlation between the increase and a change in prostate cancer screening guidelines recommending against routine prostate-specific antigen (PSA) testing.” Many prostate cancer experts believe that once prostate cancer metastasizes, it may be manageable but is not curable. At the least, treatment after metastasis is much more expensive and generally more onerous than when it is detected early and still organ-confined. So, the USPSTF recommendations have, and will continue to inevitably and needlessly condemn many men to very tragic consequences!
As anticipated by prostate cancer specialists, there has been a significant increase in the number of older men reported to have distant metastases at diagnosis, as reported in JAMA Oncology last year. A good synopsis of the report is provided here. According to the article, “The incidence of metastatic prostate cancer in older men is rising after reaching an all-time low in 2011 … The findings suggest a correlation between the increase and a change in prostate cancer screening guidelines recommending against routine prostate-specific antigen (PSA) testing.” Many prostate cancer experts believe that once prostate cancer metastasizes, it may be manageable but is not curable. At the least, treatment after metastasis is much more expensive and generally more onerous than when it is detected early and still organ-confined. So, the USPSTF recommendations have, and will continue to inevitably and needlessly condemn many men to very tragic consequences!
Paying Doctors for Not Screening?
In the course of discussion re: prostate screening with a family practice doctor, I learned that some insurers actually PAY doctors to forego screening! This is apparently a widespread but little-known practice. Presumably, the insurers would rationalize this as in keeping with the USPSTF guidelines. The ethical issues this raises are foreboding! Last year, Medicare proposed that doctors be fined for performing PSA tests, but this notion was abandoned due to significant pushback from the medical community. As patients, we’d like to think that our doctors are looking out for our interests, rather than accepting payment for non-treatment or being fearful of being fined for doing so.
One Example of the Consequences of the USPSTF Position
One example with which I am personally acquainted is that of a patient in his 60s who was denied PSA testing by his urologist for two consecutive years. When he became symptomatic, he insisted on getting tested and learned that his PSA had climbed to 21! A targeted biopsy revealed a Gleason score of 8 to 10 in all 12 samples! If only he had been tested annually, it’s likely his disease would have been detected much earlier, with a much-improved prognosis.
The BOB Opinion
Like Dr. Pat Greany, we believe that despite being less than perfect, the PSA is still a useful, inexpensive, and non-invasive test. False positives can be invalidated by additional non-invasive tests (including multi-parametric MRI) and we believe PSA testing should be done annually for all men who are 50 or older and beyond 70 if their life expectancy warrants it. For men with a family history of prostate cancer and/or ethnic predisposition, such as African-American men, it should be considered for men over 40. With the availability of post-PSA tests, the incidence of over-diagnosis and overtreatment should be greatly diminished. In addition, it is still a useful means of monitoring one’s situation after treatment as it can be indicative of a recurrence. In our opinion, there is no longer any valid reason for the USPSTF to inhibit use of this valuable test and screening for prostate cancer in general.
Six Reasons Why Prostate Cancer Screening is Important
We know that one in six men will be diagnosed with prostate cancer in his lifetime and, even with USPSTF restrictions on PSA testing, the American Cancer Society predicts that 160,000 new cases will be diagnosed in 2017.
Two simple prostate cancer tests, the digital rectal exam (DRE) and the PSA blood test help doctors detect prostate cancer early, before symptoms appear greatly increasing the odds of long-term survival.
Daton Physicians Network recently published an article titled, Six Reasons a Prostate Cancer Screening is Important. Here is a summary of the six reasons:
- Screening tests may detect prostate cancer early. Begin testing at age 50 unless you are at higher risk, in which case you should begin at age 40.
- Tests are quick and easy: PSA is a simple blood draw, and DRE is simple and effective.
- Testing can uncover prostate cancer before the symptoms appear. This is almost always the case. If left undetected, the disease can then spread to the lymph nodes and bones …” according to Dr. Mark Monsour, a urologist at Dayton Physicians Network.
- Prostate cancer is easier to treat and is more likely to be cured if it is diagnosed in the early stages of the disease. Several treatment options are available for early stage prostate cancer.
- Sometimes knowing is better than not knowing. Knowledge is power. Under certain circumstances early stage disease requires no treatment at all, other than periodic monitoring of PSA.
- Cutting-edge technology makes diagnosis and treatments more successful. In addition to PSA and DRE, other pre-biopsy tests are available. Also new imaging technology helps provide the most accurate diagnosis as well as information to help the patient and doctor choose the best treatment option.
Reirradiating Tumors with Proton Therapy
Cancer Network reported on March 20, 2017 that a study has shown the use of reirradiation with intensity modulated proton therapy (IMPT) yielded strong overall survival with limited toxicity in patients with thoracic tumors. Patients with recurrent lung cancer, for example, often have minimal to no treatment options. This study offers new hope for these patients.
In the past, doctors were reluctant to treat previously radiated tissue with any form of radiation because of toxicity concerns resulting in side effects that could significantly impact quality of life. But as the proton beam becomes more and more precise, with
pencil beam scanning and now IMPT, re-treating with protons is becoming a reality.
A retrospective study was conducted at MD Anderson on patients treated between 2011 and 2016. Most of the patients had non-small-cell-lung cancer (NSCLC) and were treated with IMPT roughly 30 months after initial radiation therapy. Median progression-free survival was 19.3 months after reirradiation.
There was minimal serious toxicity seen in the study, with no grade 4 or 5 events.
“We conclude that IMPT is an excellent choice for reirradiation,” said Dr. Jennifer Ho of MD Anderson Cancer Center. Dr. Pranshu Mohindra of the University of Maryland in Baltimore noted that, “These findings offer hope for patients with the challenging and often incurable diagnosis of recurrent lung cancer.”
We can’t help but wonder if reirradiation of recurrent prostate cancer may become a reality some day.
Another Study Shows: Low-Dose Aspirin May Cut Prostate Cancer Risk by 23%
 This is not new; we wrote about this back in June, 2016. However, more studies are confirming the connection between taking aspirin to reduce your chances of dying from prostate cancer (and other cancers). More information was presented last month at the American Association for Cancer Research in Washington, DC. Yin Cao, an instructor at Mass General Hospital and Harvard Medical School, studied data from over 43,000 men from 1986 to 2012.
This is not new; we wrote about this back in June, 2016. However, more studies are confirming the connection between taking aspirin to reduce your chances of dying from prostate cancer (and other cancers). More information was presented last month at the American Association for Cancer Research in Washington, DC. Yin Cao, an instructor at Mass General Hospital and Harvard Medical School, studied data from over 43,000 men from 1986 to 2012.
Over that 32-year period, 8,200 women and 4,600 men in the study died of cancer. The risk of death overall was 7 percent lower in women and 11 percent lower for men who took aspirin regularly, compared with those who did not. The risk of dying from cancer was 7 percent lower for women and 15 percent lower for men who took aspirin regularly, compared with those who didn’t take a regular dose. Taking regular aspirin lowered women’s risk of dying from breast cancer by 11 percent and lowered men’s risk of dying from prostate cancer by 23 percent.
The biggest benefit was with colorectal cancer, where there was a 31 percent lower risk with women and 30 percent for men who were regular aspirin takers.
Although a very safe drug, there is some risk of ulcers and gastrointestinal bleeding, but the benefits outweigh the risk for most people. Cao said, “It’s good to remember, if a person wants to take a low-dose aspirin, especially if a person has had cancer, they will want to have an initial conversation with their doctor.”

Recap Continued: National Proton Conference 2017—the Future of Protons
Yogi Berra once said, “It’s tough to make predictions, especially about the future.” Well, when some of the best minds in the proton world come together and share information about their research and clinical developments, you can bet their predictions are based on solid science.
 Last month we wrote about the annual National Proton Conference (NPC) that was organized by the National Association for Proton Therapy (NAPT) and held at the Renaissance Hotel in Orlando, FL, March 6 through 9. This event was attended by proton clinical and administrative leaders from the U.S. and some from overseas as well as proton-related vendors and medical centers interested in building proton treatment centers.
Last month we wrote about the annual National Proton Conference (NPC) that was organized by the National Association for Proton Therapy (NAPT) and held at the Renaissance Hotel in Orlando, FL, March 6 through 9. This event was attended by proton clinical and administrative leaders from the U.S. and some from overseas as well as proton-related vendors and medical centers interested in building proton treatment centers.
In addition to numerous panels and presentations during the four-day conference, there was an exhibition hall with 25 displays highlighting the latest in proton treatment center design and other related technologies.
In last month’s BOB Tales we reviewed a number of the panels and presentations as well as the well-deserved Lifetime Achievement Awards given to Dr. James M. Slater (Loma Linda University Cancer Center) and Dr. James Cox (MD Anderson Cancer Center). We also showed some interesting comparisons between proton therapy and IMRT for treating prostate cancer. And, while they were not head-to-head prospective studies, the data presented showed somewhat better disease-free survival for proton patients, especially for intermediate and high-risk patients. It also showed better outcomes with regard to gastrointestinal and genitourinary toxicity (side effects) for proton therapy.
Proton Therapy in 2021
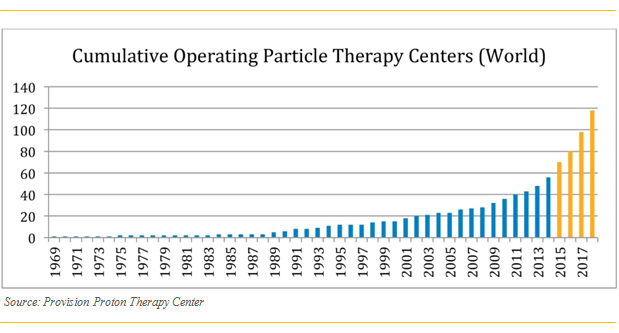
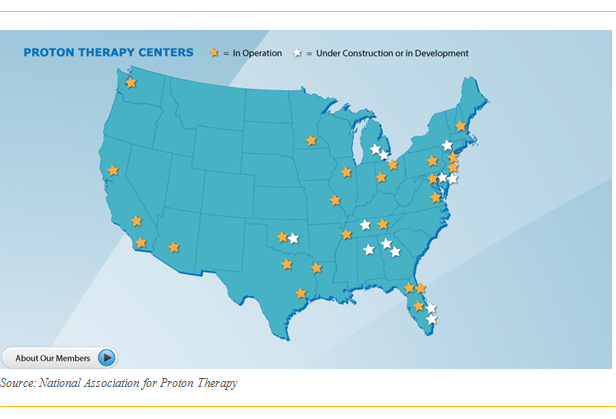
The final half-day of the conference was dedicated to anticipating what the proton therapy world might look like in 2021. Proton technology is changing rapidly with smaller, less costly proton centers being designed and built, newer patient positioning systems, new and improved beam delivery systems and more. There are 25 proton centers in the U.S. with 12 more under construction or in the planning stages. And we report almost monthly, announcements of new proton centers being constructed all over the world.
Physicians, physicists, and other scientists are continually working to improve proton therapy and plan for future generations of particle therapy treatment centers. Many were represented at the conference. The progress they are making is breathtaking and their predictions are bold.
The following figure shows the explosive growth of proton therapy worldwide (Wouldn’t you like your investment portfolio to look like this?).
Specific topics covered during this part of the conference included:
Proton Accelerators of the Future: Jay Flanz, PhD, Technical Director, Burr Proton Therapy Center, Associate Professor, Harvard Medical School, Mass. General Hospital.
Clinical Treatments in 2021: Andrew K. Lee, MD, MPH, Medical Director Texas Center for Proton Therapy.
Proton Biology in 2021: Michael Story, PhD, Professor, David M. Pistenmaa, MD, PhD, Distingjuished Chairman in Radiation Oncology, Vice-Chairman, Department of Radiation Oncology, Chief, Division of Molecular Radiation Biology University of Texas, Southwestern Medical Center.
Physics in 2021: Martin Bues, PhD, Lead Proton Physicist, Mayo clinic, Arizona, Anthony Mascia, Director, Medical Physics, Cincinnati Children’s/UC Health Proton Therapy Center, Neik Schreuder, M Sc DABR, Vice President & Chief Medical Physicist, ProVision Healthcare. From the speakers’ credentials, you can imagine the technical depth covered in these presentations.
We do not have the space to properly cover these topics in much detail, but here are a few highlights.
First Generation
First generation proton treatment centers pioneered by Loma Linda University Cancer Center were based on a physic lab model. They are extremely large, very expensive and scattered-beam based. They are still viable today, but very expensive to replicate.
First generation systems consist of a particle accelerator, a beamline, multiple gantries, beam-delivery system and patient set-up, imaging and positioning systems.
And keep in mind that, while a new, multi-room, gantry-based proton center costs in the $150 million range, the primary “competition,” a photon (X-ray based) treatment room costs about $4 million.
Second, Third, and Fourth Generation
The focus for newer generation proton systems is lower cost, both scattered and pencil beam systems, smaller footprint, and next-generation imaging. The goal seems to be to work toward targeting the cost and footprint of X-ray therapy systems.
Newer single-room proton centers are getting smaller and smaller. As mentioned in last month’s BOB Tales, we visited the UF Health Cancer Center at Orlando Health, where they have a new, Mevion single-treatment room proton system. This is a unique, small-footprint facility where the cyclotron actually rotates around the patient.
Great strides are being made in hypo-fractionation [higher dose, fewer fractions (treatments)], dealing with organ motion, improving conformity of the beam, increasing throughput and lowering cost of both capital equipment and patient treatment.
Progress is being made in dealing with tumor-target movement, caused by breathing, with beam delivery precisely timed to pulse during the pause between breaths.
Cyclotrons and synchrotrons have been used to accelerate protons since the beginning, but emerging technologies may be better. Laser accelerators are being considered by researchers. They would be smaller, cheaper, and an improvement over current cyclotron technology.
Better beam focusing is allowing doctors to treat smaller and smaller margins around the target volume. There is debate on how tight the margins should be, as cancer in the margins can be destroyed with the proton beam.
Other improvements anticipated for 2021 include improved patient positioning and imaging—including in-room imaging, significant improvements in treatment planning software, faster beam delivery, more fixed beam systems, heavier ion systems, such as carbon, helium, and lithium, possibly multiple ions per treatment field, and superconducting gantries. The advantage of heavier ions, such as helium and carbon, are even greater relative biologic effectiveness (RBE) vs. X-rays.
The following figure shows the locations and growth of proton centers in the U.S.
Gantry vs. Fixed Beam
Gantries are large; they take up considerable space (three stories tall), and add considerable cost. But gantry technology allowed physicians to treat patients and tumor sites that fixed-beam systems did not. That may be changing with new beam delivery systems tailored for fixed-beam applications.
Clinical Proton Therapy
According to Dr. Andrew Lee, by some estimates the U.S. needs almost 100 proton gantries. We are far from that number for several reasons: cost, complex technology, need for more clinical studies, lack of education (medical community and patients), lack of medical insurer coverage, and resistance from non-particle therapy centers. These barriers are coming down and the number of proton centers and treatment rooms will increase rapidly in the coming years.
In addition to what is mentioned above, the future of proton therapy will include:
- Increased number of pencil beam facilities
- Intensity modulated proton therapy (IMPT)
- Better treatment planning software
- Smaller and less expensive proton facilities
- On-board volumetric imaging
- Increased utilization of stereotactic body radiation therapy (SBRT)
The results of these achievements will result in significantly improved conformity of the beam and a dramatic improvement in limiting normal tissue exposure. Treatment sites likely to see the most benefits include cranio-spinal (where thyroid, heart, lungs and other body parts are protected); breast and breast lymph nodes (where the heart is protected, reducing the risk of coronary events); Hodgkin’s lymphoma, lung cancer (better targeting, managing respiratory motion, reducing heart dose); liver cancer, brain cancer and yes, prostate cancer.
Improvements in conformity will also allow physicians to use protons to treat oligo-metastatic disease (small number of metastatic tumor sites originating from the primary tumor). Future treatment with proton therapy is projected to be faster and safer.
Physics 2021
This report was highly technical in nature and covered topics such as log file quality assurance, knowledge-based treatment planning, “at console” dose evaluation and adapting and biological dose calculation. It is far too technical and complex for this journal. Suffice to say, some very smart people are working on all aspects of proton therapy for the future.
According to the American Society of Clinical Oncology (ASCO), there were 14 million cancer survivors in the U.S. in 2013. Within the next 10 years, estimated cancer survivors are expected to exceed 20 million. Proton therapy will undoubtedly play a significant role in achieving this objective.
In Summary
Henry Ford once said, “If I had asked people what they wanted, they would have said “faster horses.”
We truly believe that the analogy holds true: The emergence of particle therapy versus X-ray radiotherapy for treating cancers and other diseases is analogous to the invention of the automobile versus horses for personal travel.
If we look back on early automobiles we can conclude that, while they were a great improvement over horseback riding, over the years they have revolutionized travel. The same can be said about proton therapy. We are still in the early stages of particle therapy evolution. The best is yet to come, and the right people and institutions are working on it. Stay tuned.
Pacific Northwest BOB Reunion
When: Thursday, May 25, 2017: Golf during the day and dinner at 5:30 p.m.
Where: Portland Adventist Medical Center, 10123 S.E. Market Street, Portland, OR 97216
What: Enjoy a buffet dinner and an evening of reflection on our proton therapy treatment. During the event, there will be a presentation on new happenings in proton therapy at Loma Linda University Health. The price is $20.00 per person. Register here for the dinner.
If you’re interested in playing golf earlier in the day, email Gary Brown at [email protected] for more information.
Fargo, ND BOB Reunion
When: Thursday, June 15, 2017: Golf during in the morning and luncheon at 1:00 p.m.
Where: The golf course is to be determined. A reunion luncheon will be held at the SpitFire Bar and Grill located at 1600 13th Ave. E. West Fargo, ND.
What: The construction of new towers at the Loma Linda University Children’s Hospital and the university’s main hospital are underway. Billie Baker, Senior Development Officer, Philanthropy, will update attendees on Vision 2020 and also a report on recent activities at the proton center. Invite your friends and family; mingle with fellow patients, former and current; and enjoy wood fired and smoked “food with attitude.”
If you’re interested in playing golf or attending the luncheon, please RSVP to Billie Baker: Email [email protected] or call 909-558-3228.
Member’s Testosterone Level Way Off Charts
We heard from one of our members that a recent blood test reported his testosterone level was dangerously high, significantly out of the normal range and “way off the charts.”
“I was stunned,” he said. Knowing that high testosterone levels can feed prostate cancer, he contacted his doctor to determine what might be the cause of the problem.
When his doctor called him back, he said, “Well, I’ve got good news and bad news. The bad news is your testosterone is considerably out of the normal range. The good news is you’re not a woman.”
It seems that when his blood work was submitted, he was listed as “F” for female, rather than “M” for male. The normal testosterone range for women is 30 to 95 ng/mL, and for men … 300 to 1200 ng/mL. His testosterone level was 598, which is more than 500 percent above the top of the range for a woman, but comfortably in the middle of the normal range for a man.
“It’s not often we get a smile or a belly laugh when we visit our doctor, but this time certainly was one,” he said. “Problem solved.”
Your Story
We have learned that our member testimonials are a major factor in the treatment decision making process of newly diagnosed men. Reading the stories of men who have “been there” are comforting and often inspirational to those who are scared and confused about what to do after being diagnosed. If you feel your experience of prostate cancer and proton therapy could be helpful to someone else, please consider sending us your testimonial to post on our website. For more information, please send an email to Deb Hickey.
Intraductal Prostate Cancer Reference List
Part of our mission is to spread the word and educate others about proton therapy; to share our stories and the benefits we received as a result of our treatment decision. One way members can help is by volunteering to be on one of our former proton patient reference lists, making themselves available by phone or email to men who are seeking information about proton therapy. We have more than 35 reference lists.
Thousands of our members have reported that talking with former patients about their experience of proton therapy was a major factor in their treatment decision.
We are looking to create a reference list of members who were diagnosed with intraductal prostate cancer. If you were diagnosed with intraductal prostate cancer, had proton therapy, and are willing to communicate with prospective proton patients about your experience and outcome, please let us know.
Kidney Transplant Reference List
We are also looking to create a reference list of members who had kidney transplants prior to being treated with proton therapy for prostate cancer. If you had a kidney transplant and are willing to communicate with prospective proton patients about your experience and outcome, please let us know.

Gift of Shares from US Ambassador: A Savvy Donor Investment Strategy
By Lynn McDowell, Planned Giving Officer, Loma Linda University Health
By all accounts, Ambassador Joseph Verner Reed was an outstanding and discerning person. “He was a man of elegance, grace, wit, flamboyance and razor sharp intellect,” said David Rockerfeller, chairman of Chase Manhattan Bank, “a diplomat’s diplomat.” After transitioning from his position as a vice president of the Chase Manhattan Bank to life as a diplomat, the US ambassador to the United Nations became undersecretary-general of the UN, chief of protocol for President George H.W. Bush, a humanitarian, a loyal member of the BOB and a financially-savvy contributor to proton therapy research through the James M. Slater Chair at Loma Linda University Health (LLUH).
.jpg) Ambassador Reed chose his charities and giving methods carefully. After he was treated with proton therapy for his prostate cancer in 1997, he felt deeply about the treatment and the institution for sparing his life and maintaining the quality of his life. He wanted to give back; he used gifts of stock to make donations—a tax-efficient way to move dollars to charity.
Ambassador Reed chose his charities and giving methods carefully. After he was treated with proton therapy for his prostate cancer in 1997, he felt deeply about the treatment and the institution for sparing his life and maintaining the quality of his life. He wanted to give back; he used gifts of stock to make donations—a tax-efficient way to move dollars to charity.
“Planned Giving is a well-kept secret in many quarters,” said Todd Mekelburg, Director of Planned Giving at LLUH. “Ambassador Reed’s example is helping to change that. When a man of the Ambassador’s financial experience and discernment chooses to use planned giving methods, people take note. He’s a good example of the thoughtful, big-picture donor who explores ways to ‘grow’ their donation dollar, which planned giving methods so often do.”
Ambassador Reed’s financial acumen and support of proton therapy research made him the donor of choice to kick off a new education and planned giving awareness “Powerful Strategies” campaign in LLUH’s newly-redesigned Scope magazine. Scope is sent to all alumni and supporters of LLUH.
Ambassador Reed’s choice of causes illustrates his foresight. Proton therapy is becoming more widely used, with many institutions modeling their programs on the work of LLUH. LLUH is also expanding its research capabilities. Research, including proton therapy research, is a transformative part of LLUH’s comprehensive effort called Vision 2020—The Campaign for a Whole Tomorrow, which will continue to keep LLUH at the forefront of healthcare.
 Reed, who passed away last year, is fondly remembered at LLUH. Dr. Jerry Slater, who heads the proton therapy center, recalls unannounced visits to his office by the ambassador, whom he considered a friend. Ever gracious, Reed’s diplomatic comments on the “visual filing system” on Slater’s desk made the busy doctor smile. At home, Dr. Slater is reminded of Reed’s talent for observation by a package of US stamps in collector-worthy condition—a gift from the Ambassador when he learned Slater was a collector.
Reed, who passed away last year, is fondly remembered at LLUH. Dr. Jerry Slater, who heads the proton therapy center, recalls unannounced visits to his office by the ambassador, whom he considered a friend. Ever gracious, Reed’s diplomatic comments on the “visual filing system” on Slater’s desk made the busy doctor smile. At home, Dr. Slater is reminded of Reed’s talent for observation by a package of US stamps in collector-worthy condition—a gift from the Ambassador when he learned Slater was a collector.
On the donation side, the gifts of stock used by Reed provide several benefits. These include avoiding capital gains tax on appreciation. At the same time, a tax receipt is issued for the full present value of the stock, and donors take an income tax charitable deduction when they itemize. This can be used to offset other income and further reduce taxes. The key is to have the stock itself gifted in kind to the charity. Typically, the charity will immediately sell the stock and receive more than if the donor had sold the stock and given what was left after tax.
 How to Contribute to Proton Research
How to Contribute to Proton Research
- Donate Online: Visit the LLUCC website. Make sure the “Designation Type” is set to “Proton” and the “Designation” is set to “Robert J. Marckini Chair."
- Send a Check: Make your check out to “LLUCC Proton” with “Marckini Chair” on the memo line and send to: LLUH, Office of Philanthropy, P.O. Box 2000, Loma Linda, CA 92354.
- Make a Call: Contribute by phone. Contact Elvia DeHaro at 909-558-5010
- Make a Future Gift: Contact Todd Mekelburg at the Office of Planned Giving at Loma Linda University Health at 909-558-5376 or [email protected].
- Other Ways to Give: Contact Matt Miller at the Office of Philanthropy at Loma Linda University Health at 909-558-3582 or [email protected].

Beware of Hidden Sugar
 We’ve written extensively on the dangers of too much sugar in your diet. The Anticancer book by Dr. David Servan-Schreiber covers this topic in great detail.
We’ve written extensively on the dangers of too much sugar in your diet. The Anticancer book by Dr. David Servan-Schreiber covers this topic in great detail.
You know that sugar can be bad for you, so you’ve probably done the right thing and cut back on cakes, candies, and desserts. You may also have stopped adding sugar to your coffee and switched to diet soda (not that artificial sweeteners are better for you!). And you probably pay more attention to food labels, checking on the amount of sugar in products you are buying.
The problem is, sugar is often hidden on product labels. Food manufacturers know that health-conscious people are trying to avoid sugar, so their labels often have sugars identified in ways we might not recognize, such as agave nectar, barley malt, caramel, cane juice, molasses, panocha, sweet sorghum, and treacle. In fact, there are at least 61 names for sugar additives often found in foods we buy every day. You can find all 61 here.
As Francis Bacon said, “Knowledge is power.”
Series: “Make Vegetables Taste Good”
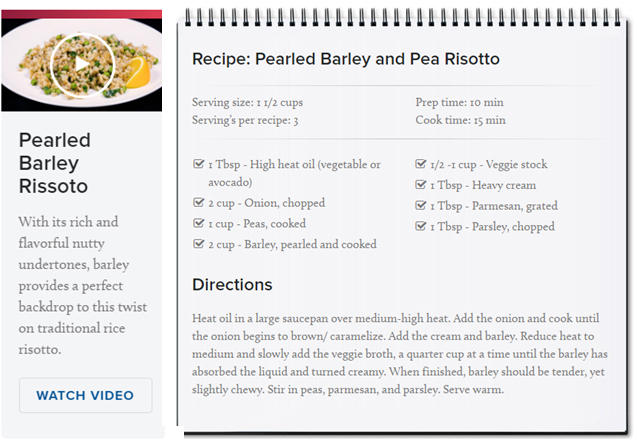
This is the tenth segment on a subject that’s consistent with our Anticancer series that began in October 2016. We made it our mission to find recipes that make the most healthful vegetables (and other foods, in this case) taste delicious.
Loma Linda University Health has a series on their website called, “LIVE IT: In the Kitchen” that features short videos inspiring healthful, wholesome home cooking. In less than a minute, each episode demonstrates how to make quick-and-easy meals. Below each video, you’ll find the full recipe and cooking directions.
Below is a recipe Deb tried last week and loved. Note that although barley may not be as popular as other whole grains (e.g. oats, wheat, quinoa), it has some impressive health benefits. Some of them are listed below:
- Controls blood sugar
- Lowers glucose levels
- Reduces blood pressure
- Lowers cholesterol
- Fewer calories
- Many more
Pearled Barley and Pea Risotto
Want to share your healthful cooking tips and/or recipes? Write to us!

Amazon Reviews: No Signs of Slowing Down
Though BobMarckini’s book, You Can Beat Prostate Cancer: And You Don’t Need Surgery To Do It was published in 2007, readership is still strong. Technology has advanced and there are new-and-improved imaging techniques, but the bottom line remains—proton therapy cures cancer at least as (or better than) any other option, and the quality of life after treatment is best by a wide margin. And people are interested and excited about that; we’ve just surpassed 315 Amazon reader reviews! A few excerpts from the latest reviews are on the following page.
 Get this book if you want the best overview of WHAT to do now and in the future for prostate cancer or increasing PSA scores.
Get this book if you want the best overview of WHAT to do now and in the future for prostate cancer or increasing PSA scores.
This is a MUST buy if you think you may be developing prostate cancer or have been diagnosed with prostate cancer. It is VERY, VERY helpful ... It is my go-to book and I felt after reading this that I knew as much, if not more, than my doctor regarding protocols and therapies and the risks associated with each one … My doc doesn’t really seem to care or know about all of the possible therapies nor does he want to recommend one, so I decided to figure it out for myself. You must take control of your own health when it comes to making a decision about prostate cancer or increasing levels of PSA. Get educated ... this book started me on a one-year search of new therapies and all sorts
of ways to live in a more healthy way, from exercise to eating right. Get the book and follow Robert’s advice! —Msquared, 4/17/17
 His plan is easy to follow and undated …
His plan is easy to follow and undated …
In my opinion, this is the first book that any man (or woman that is concerned about their father or other man in their life) should read after being diagnosed with prostate cancer … Although his book was published over 10 years ago, and there are a few more treatment options available, his plan is easy to follow and undated … —Uncle Ray, 4/1/17
Buy Online, in Bulk or in Spanish
Online: Paperback: $19.00--•--Kindle: $9.99--•--NOOK Book: $9.99--•--Apple iBook: $9.99
In Bulk: Conctact us for a discount price list. Proceeds from book sales support proton therapy research through the Robert J. Marckini Endowed Chair at LLUCC.
In Spanish: Buy the print version or in eBook format.

Last Month’s Brain Teaser
Say you catch a fish that weighs five pounds plus half its weight. How much does the fish weigh?
Answer: 10 Pounds. Couldn’t be anything else!
Winner: The May brain teaser winner is Ken Osbourn of Chesterfield, MO.
In June 2000, Ken retired after 35 years with IBM as a Systems Engineer and Software Sales Representative. At that time, he began an exercise routine and lost 50 pounds. “I was looking pretty buff right before I had a heart attack 18 months later,” he told us. “Six months after completing cardio rehab, I was diagnosed with prostate cancer.”
Ken, 59, began researching the Internet; there, he found Loma Linda University Cancer Center’s proton therapy program. His urologist recommended surgery, dismissing proton as “experimental,” but after learning about the benefits of proton therapy, Ken’s decision was made.
 Ken and his wife, Jan, traveled to Loma Linda in early 2003 to begin his treatment. To this day, they consider the two and a half months they spent in Loma Linda as “the best vacation of our lives.” Each morning, Ken got up early for treatment and then the two spent their days touring southern California—beaches, mountains, deserts, museums, wineries, etc. They enjoyed weekly support group lunches, dinners, and meetings. Ken also spent a lot of time doing water aerobics at Loma Linda’s Drayson Center for health and fitness.
Ken and his wife, Jan, traveled to Loma Linda in early 2003 to begin his treatment. To this day, they consider the two and a half months they spent in Loma Linda as “the best vacation of our lives.” Each morning, Ken got up early for treatment and then the two spent their days touring southern California—beaches, mountains, deserts, museums, wineries, etc. They enjoyed weekly support group lunches, dinners, and meetings. Ken also spent a lot of time doing water aerobics at Loma Linda’s Drayson Center for health and fitness.
“Something about Loma Linda and proton therapy makes people wax poetic; upon my ‘graduation,’ I composed a song parody and a group of us performed to Sonny and Cher’s ‘The Beam Goes On.’”
Fourteen years after treatment, Ken is in fine health. He and Jan enjoy travel, reading, and most of all, spending time with their twin grandsons. Ken also spreads the word about his proton therapy experience and has led many to Loma Linda for treatment.
New Brain Teaser
Say a painter can paint a garage in a day. His friend can paint a garage in two days. Working together, how long will it take for them to paint two garages?
Send your answer to [email protected] for a chance to win a signed copy of Bob Marckini’s book, You Can Beat Prostate Cancer.
 Communication Barriers
Communication Barriers
A wife asks her husband, “Could you please go shopping for me and buy a carton of milk? And if they have avocados, get six.”
A short time later the husband comes back with six cartons of milk.
The wife asks him, “Why did you buy six cartons of milk?”
He replied, “They had avocados.”
If you’re a woman, I’m sure you’re going back to read it again. Men will get it the first time.
Great Truths
“In my many years I have come to a conclusion that one useless man is a shame; two is a law firm; and three or more is a congress.” —John Adams
“If you don’t read the newspaper you are uninformed. If you do read the newspaper you are misinformed” —Mark Twain
“Suppose you were an idiot. And suppose you were a member of Congress. But then I repeat myself.” —Mark Twain
“I contend that for a nation to try to tax itself into prosperity is like a man standing in a bucket and trying to lift himself up by the handle.” —Winston Churchill
“Government’s view of the economy could be summed up in a few short phrases: If it moves, tax it. If it keeps moving, regulate it. And if it stops moving, subsidize it.” —Ronald Reagan
“I don’t make jokes. I just watch the government and report the facts.” —Will Rogers

Quote of the Month:
“To succeed in life, you need three things: a wishbone, a backbone and a funny bone.”
— Reba McEntire


Six Little Stories —Nancy Friedman
Once all the villagers decided to pray for rain. On the day of prayer all the people gathered. But only one boy came with an umbrella.
That’s FAITH.
When you throw babies in the air, they laugh because they know you will catch them.
That’s TRUST.
Every night we go to bed without any assurance of being alive the next morning, but still we set the alarms to wake up.
That’s HOPE.
We plan big things for tomorrow, in spite of zero knowledge of the future.
That’s CONFIDENCE.
We see the world suffering, but still we get married and have children.
That’s LOVE.
On an old man’s shirt there was a sentence, “I am not 80 years old; I am sweet 16 with 64 years of experience.”
That’s ATTITUDE.
Have a happy day and live your life like the six stories.
When I was a child, I thought nap time was punishment. Now, it’s like a mini-vacation.
Low PSAs to all,
Bob Marckini and Deb Hickey
To print the BOB Tales newsletter or view the newsletter with a larger font size, click here for the PDF file.
NO MEDICAL ADVICE: Material appearing here represents opinions offered by non-medically-trained laypersons. Comments shown here should NEVER be interpreted as specific medical advice and must be used only as background information when consulting with a qualified medical professional.