Myth #7: There are no studies or documentation that support the success or superiority of proton therapy for prostate cancer.
We often hear from recently diagnosed men that their urologist is pressuring them to have surgery. When they bring up the subject of proton, they are often told some of the stories we have already addressed in Myths 1 through 6, such as “Proton therapy is ‘experimental’ or ‘investigational,’” or “it’s no better than advanced forms of conventional radiation.” Another story they are often told is that there are no published studies, documentation, or articles on proton therapy for prostate cancer showing the benefits, or no statistics to back-up claims of proton’s superiority. This is not true.
Over the past 20+ years there have been dozens of studies and articles on this subject. A partial list is below.
What do these studies, surveys, and articles tell us? They tell us that:
- Proton therapy is the most precise form of radiotherapy available today.
- Two to three times less radiation is deposited on healthy tissue with proton than with any form of photon (X-ray) radiation.
- Higher doses of radiation do a better job of killing cancer, and, contrary to experience with conventional x-ray radiation, when proton doses are increased there is no corresponding increase in collateral damage and side effects.
- Cure rates with proton therapy are at least as good as surgery or conventional radiation.
- Genitourinary and gastrointestinal complications are lower with proton therapy than with other treatment modalities.
- Sexual function is better preserved with proton therapy.
- Proton therapy is an excellent treatment choice for young men with prostate cancer.
Here is a sampling of some of the studies, articles, and surveys relating to proton therapy for prostate cancer:
- Comparative effectiveness study of patient-reported outcomes after proton therapy or IMRT for prostate cancer. Cancer. 2014. Hoppe, Michalski, Mendenhall, et al.
- Four-year Outcomes from a Prospective Phase II Clinical Trial of Moderately Hypofractionated Proton Therapy for Localized Prostate Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2019. Grewal, Schoenewolf, Jeong Min E, et al.
- Five-year outcomes from 3 prospective trials of image-guided proton therapy for prostate cancer. Int. J Radiat. Oncol. Biol Phys. 2014. Mendenhall, Hoppe, Nichols, et al.
- Ten Year Study: Proton Therapy for Prostate Cancer: The Initial Loma Linda University Experience. Int. J. Radiation Oncology Biol. Phys. Vol 59, No. 2, pp, 348-352, 2004. Jerry F. Slater, M.D., et. al.
- Fifteen Year Report: Clinical Applications of Proton Radiation Treatment at Loma Linda University: Review of Fifteen-year Experience. Technology in Cancer Research and Treatment ISSN 1533-0346, Vol. 5, No. 2, April 2006. Jerry D. Slater, M.D.
- Randomized Trial Comparing Conventional-Dose With High-Dose Conformal Radiation Therapy in Early-Stage Adenocarcinoma of the Prostate: Long-Term Results From Proton Radiation Oncology Group/American College of Radiology 95-09. J Clin Oncol 28.2010, American Society of Clinical Oncology. Anthony L. Zietman, M.D. et. al.
- Conformal Proton Beam Radiation Therapy of Prostate Cancer. Prostate Cancer Communication Newsletter. Vol 23 No 1, March 2007. Carl J. Rossi Jr. M.D.
- Urinary functional outcomes and toxicity five years after proton therapy for low- and intermediate-risk prostate cancer: Results of two prospective trials. Acta Oncol. 2013; April; 52(3):463-469. Randal H. Henderson, et. al
- Early Outcomes From Three Prospective Trials Of Image-Guided Proton Therapy For Prostate Cancer. Int. J. Radiation Oncology Biol. Phys., 2010. Nancy P. Mendenhall, MD et. al.
- Proton-beam Rx reduces prostate cancer recurrence. Oncology NEWS International. Vol. 19 No. 1
- Clinical evidence demonstrates good disease control with minimal early adverse events. By Ed Susman | January 20, 2010
- Study: Majority of Men Report Being Sexually Active After Proton Therapy for Prostate Cancer. WebMD Health News Nov. 5, 2010
- Proton Therapy for Prostate Cancer. Oncology. June 2011. Bradford Hoppe, M.D. MPH, et. al
- Proton-beam Rx Reduces Prostate Cancer Recurrence. Clinical Evidence Demonstrates Good Disease Control With Minimal Early Adverse Events. Oncology News International, Vol. 19 No. 1. January 2010
- Proton Beam Therapy Affects Less Healthy Tissue Than Standard Radiation. Medical Edge Newspaper. Mayo Clinic. January 27, 2012
- Hypofractionated passively scattered proton radiotherapy for low- and intermediate-risk prostate cancer is not associated with post-treatment testosterone suppression. Acta Oncol 52(3):492-7 (2013) PMID 23477360
- A Phase II Study of Hypofractionated Proton Therapy for Prostate Cancer. Acta Oncol (2013) PMID 23398594. Yeon-Joo Kim, et. al.
- Outcomes in Men with Large Prostates (>60 cc) Treated with Definitive Proton Therapy for Prostate Cancer. Acta Oncol (2012) PMID 23244673. Lisa McGee, et. al
- Erectile Function, Incontinence, and Other Quality of Life Outcomes Following Proton Therapy for Prostate Cancer in Men 60 Years Old and Younger. Cancer.September 15, 2012. Bradford S. Hoppe, MD MPH, et. al.
- 2009 Survey of Brotherhood of the Balloon Membership Reports 94% Cure Rates and Minimal Side Effects. The BOB represents more than half the men who have been treated with proton therapy for prostate cancer.
- Second Survey of Brotherhood of the Balloon Membership Using Standardized EPIC Survey Tool Confirms Results of 2009 Survey. Reported at ASTRO and NAPT.
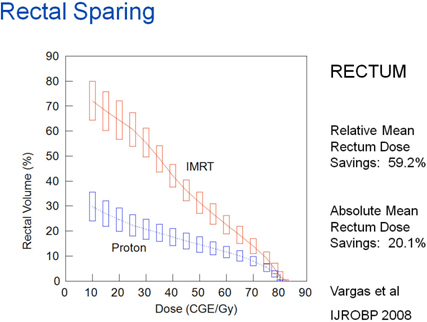
The graph below titled, “Rectal Sparing,” shows considerably higher doses of radiation to the rectum with IMRT vs. proton.
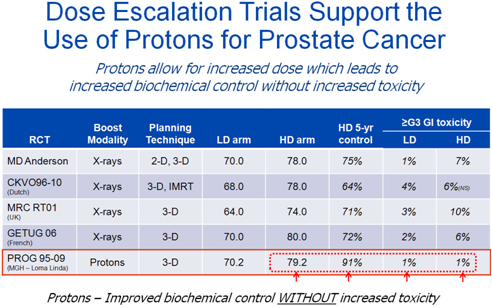
The chart below titled, “Dose Escalation Trials Support the Use of Protons for Prostate Cancer,” shows better disease control with proton and significantly lower GI (gastrointestinal) toxicity.
More Research Showing the Benefits of Proton Therapy:
There are over 800 published peer reviewed journal articles and more than 30 active clinical trials evaluating the benefits of proton therapy. The following is a small sample of recent research supporting the value of proton therapy for diseases other than prostate cancer.
Proton therapy has fewer side effects across all cancers than photon therapy, reducing costly side effects and hospitalizations during the course of treatment.
1) Baumann BC, Mitra N, Harton JG, Xiao Y, Wojcieszynski AP, Gabriel PE, Zhong H, Geng H, Doucette A, Wei J, O'Dwyer PJ, Bekelman JE, Metz JM. Comparative Effectiveness of Proton vs Photon Therapy as Part of Concurrent Chemoradiotherapy for Locally Advanced Cancer. JAMA Oncol. 2019 Dec 26. Epub ahead of print] PubMed PMID: 31876914.
Proton therapy better preserves quality of life across all cancers compared with photon therapy. Cancer survivors are living longer due to effective treatments developed in the last few years. It is more important than ever to preserve quality of life for long-term survivors.
1) Verma V, Simone CB 2nd, Mishra MV. Quality of Life and Patient-Reported Outcomes Following Proton Radiation Therapy: A Systematic Review. J Natl Cancer Inst. 2018;110(4).
Proton therapy improves overall survival and reduces high grade complications for head and neck cancers compared with photon therapy. Side effects of radiation for head and neck cancer can cause malnutrition, need for feeding tubes, dehydration, and other costly side effects that can require hospitalizations. Proton therapy delivers less radiation to healthy tissue and thus reduces the incidence of these costly side effects.
1) Patel SH, Wang Z, Wong WW, Murad MH, Buckey CR, Mohammed K, Alahdab F, Altayar O, Nabhan M, Schild SE, Foote RL. Charged particle therapy versus photon therapy for paranasal sinus and nasal cavity malignant diseases: a systematic review and meta-analysis. Lancet Oncol. 2014;15(9):1027-38.
2) McDonald MW, Liu Y, Moore MG, Johnstone PA. Acute toxicity in comprehensive head and neck radiation for nasopharynx and paranasal sinus cancers: cohort comparison of 3D conformal proton therapy and intensity modulated radiation therapy. Radiat Oncol. 2016;11:32.
3) Blanchard P, Garden AS, Gunn GB, Rosenthal DI, Morrison WH, Hernandez M, Crutison J, Lee JJ, Ye R, Fuller CD, Mohamed AS, Hutcheson KA, Holliday EB, Thaker NG, Sturgis EM, Kies MS, Zhu XR, Mohan R, Frank SJ. Intensity-modulated proton beam therapy (IMPT) versus intensity-modulated photon therapy (IMRT) for patients with oropharynx cancer - A case matched analysis. Radiother Oncol. 2016;120(1):48-55.
4) Romesser PB, Cahlon O, Scher E, Zhou Y, Berry SL, Rybkin A, Sine KM, Tang S, Sherman EJ, Wong R, Lee NY. Proton beam radiation therapy results in significantly reduced toxicity compared with intensity-modulated radiation therapy for head and neck tumors that require ipsilateral radiation. Radiother Oncol. 2016;118(2):286-92.
Proton therapy is the treatment of choice for base of skull cancers and chordomas, where sensitive brain and ocular structures prevent safe treatment with conventional radiation. Proton therapy has been shown to improve tumor control and overall survival for these cancers compared with photon therapy.
1) Zhou J, Yang B, Wang X, Jing Z. Comparison of the effectiveness of radiotherapy with photons and particles for chordoma after surgery: a meta-analysis. World Neurosurg. 2018;117:46-53.
2) Amichetti M, Cianchetti M, Amelio D, Enrici RM, MinnitiG. Proton therapy in chordoma of the base of the skull: a systematic review. Neurosurg Rev. 2009;32(4):403- 16.
Proton therapy can improve outcomes when used to treat brain tumors, offering reduced side effects and treatment options where no safe options exist in the treatment of recurrent brain tumors. Proton therapy can also decrease injury to normal brain tissues in primary brain tumor treatment.
1) Hug EB, DeVries A, Thornton AF, Munzenrider JE, Pardo FS, Hedley-Whyte ET, Bussiere MR, Ojemann R. Management of atypical and malignant meningiomas: Role of high-dose, 3D-conformal radiation therapy. J Neurooncol. 2000;48(2):151-160.
2) Combs SE, Debus J, Schulz-Ertner D. Radiotherapeutic alternatives for previously irradiated recurrent gliomas. BMC Cancer. 2007;7:167.
Proton therapy improves survival for locally advanced stage non-small cell lung cancer compared with photon therapy.
1) Higgins KA, O'Connell K, Liu Y, Gillespie TW, McDonald MW, Pillai RN, Patel KR, Patel PR, Robinson CG, Simone CB 2nd, Owonikoko TK, Belani CP, Khuri FR, Curran WJ, Ramalingam SS, Behera M. National Cancer Database Analysis of Proton Versus Photon Radiation Therapy in Non-Small Cell Lung Cancer. Int J Radiat Oncol Biol Phys. 2017;97(1):128-137.
Proton therapy improves survival for early stage non-small cell lung cancer compared with photon therapy.
1) Nantavithya C, Gomez DR, Wei X, Komaki R, Liao Z, Lin SH, Jeter M, Nguyen QN, Li H, Zhang X, Poenisch F, Zhu XR, Balter PA, Feng L, Choi NC, Mohan R, Chang JY. Phase 2 Study of Stereotactic Body Radiation Therapy and Stereotactic Body Proton Therapy for High-Risk, Medically Inoperable, Early-Stage Non-Small Cell Lung Cancer. Int J Radiat Oncol Biol Phys. 2018;101(3):558-563.
2) Chi A, Chen H, Wen S, Yan H, Liao Z. Comparison of particle beam therapy and stereotactic body radiotherapy (SBRT) for early stage non-small cell lung cancer: A systematic review and hypothesis-generating meta-analysis. Radiother Oncol. 2017;123(3):346-354.
Proton therapy improves overall survival and reduces high grade complications and resulting costly hospitalizations for esophageal cancer compared with photon therapy.
1) Lin SH, Hobbs B, Thall P, Tidwell RS, Wei X, Komaki RU, Chang JY, Chun SG, Jeter MD, Hahn SM, Swisher SG, Ajani JA, Blum Murphy M, Vaporciyan AA, Mehran R, Koong AC, Gandhi S, Hofstetter W, Liao Z, Mohan R. Results of a Phase II Randomized Trial of Proton Beam Therapy vs Intensity Modulated Radiation Therapy in Esophageal Cancer. Int J Radiat Oncol Biol Phys. 105(3):S680-681.
2) Xi M, Xu C, Liao Z, Chang JY, Gomez DR, Jeter M, Cox JD, Komaki R, Mehran R, Blum MA, Hofstetter WL, Maru DM, Bhutani MS, Lee JH, Weston B, Ajani JA, Lin SH. Comparative Outcomes After Definitive Chemoradiotherapy Using Proton Beam Therapy Versus Intensity Modulated Radiation Therapy for Esophageal Cancer: A Retrospective, Single-Institutional Analysis. Int J Radiat Oncol Biol Phys. 2017;99(3):667-676.
3) Lin SH, Merrell KW, Shen J, Verma V, Correa AM, Wang L, Thall PF, Bhooshan N, James SE, Haddock MG, Suntharalingam M, Mehta MP, Liao Z, Cox JD, Komaki R, Mehran RJ, Chuong MD, Hallemeier CL. Multi-institutional analysis of radiation modality use and postoperative outcomes of neoadjuvant chemoradiation for esophageal cancer. Radiother Oncol. 2017;123(3):376-381.
4) Wang J, Wei C, Tucker SL, Myles B, Palmer M, Hofstetter WL, Swisher SG, Ajani JA, Cox JD, Komaki R, Liao Z, Lin SH. Predictors of postoperative complications after trimodality therapy for esophageal cancer. Int J Radiat Oncol Biol Phys. 2013;86(5):885- 91.
5) Lin SH, Hobbs B, Thall P, Tidwell RS, Wei X, Komaki RU, Chang JY, Chun SG, Jeter MD, Hahn SM, Swisher SG, Ajani JA, Blum Murphy M, Vaporciyan AA, Mehran R, Koong AC, Gandhi S, Hofstetter W, Liao Z, Mohan R. Results of a Phase II Randomized Trial of Proton Beam Therapy vs Intensity Modulated Radiation Therapy in Esophageal Cancer. Int J Radiat Oncol Biol Phys. 2019;105(3):680-681.
Proton therapy improves survival for hepatocellular carcinoma compared with photon therapy and stereotactic body radiation therapy.
1) Sanford NN, Pursley J, Noe B, Yeap BY, Goyal L, Clark JW, Allen JN, Blaszkowsky LS, Ryan DP, Ferrone CR, Tanabe KK, Qadan M, Crane CH, Koay EJ, Eyler C, DeLaney TF, Zhu AX, Wo JY, Grassberger C, Hong TS. Protons versus Photons for Unresectable Hepatocellular Carcinoma: Liver Decompensation and Overall Survival. Int J Radiat Oncol Biol Phys. 2019;105(1):64-72.
2) Hasan S, Abel S, Verma V, Webster P, Arscott WT, Wegner RE, Kirichenko A, Simone CB 2nd. Proton beam therapy versus stereotactic body radiotherapy for hepatocellular carcinoma: practice patterns, outcomes, and the effect of biologically effective dose escalation. J Gastrointest Oncol. 2019;10(5):999-1009.
Proton reduces side effects for pancreatic and gastrointestinal tumors compared with photon therapy.
1) Verma V, Lin SH, Simone CB, et al. Clinical outcomes and toxicities of proton radiotherapy (PT) for gastrointestinal neoplasms: a systematic review. J Gastrointest Oncol. 2016;7(4):644-664.
Proton therapy offers a curative option not available with photon therapy for recurrent tumors. When cancers recur, traditional radiation is often not a safe treatment option, leaving cancer patients with limited treatment options and prognosis. Proton therapy gives patients with cancer recurrence a treatment option they would not have with conventional radiation and can lead to cures in select patients.
1) Verma V, Rwigema JM, Malyapa RS, Regine WF, Simone CB 2nd. Systematic assessment of clinical outcomes and toxicities of proton radiotherapy for reirradiation. Radiother Oncol. 2017;125(1):21-30.
2) Chao HH, Berman AT, Simone CB 2nd, Ciunci C, Gabriel P, Lin H, Both S, Langer C, Lelionis K, Rengan R, Hahn SM, Prabhu K, Fagundes M, Hartsell W, Mick R, Plastaras JP. Multi-Institutional Prospective Study of Reirradiation with Proton Beam Radiotherapy for Locoregionally Recurrent Non-Small Cell Lung Cancer. J Thorac Oncol. 2017;12(2):281-292.
Proton therapy is the preferred treatment for pediatric patients needing curative radiotherapy. Proton radiotherapy decreases the risks for cancers caused by radiotherapy, decreases brain injury and improves neurocognitive function after treatment, and significantly reduces overall acute and acute and chronic life-long side effects.
1) Kahalley LS, Peterson R, Ris MD, et al. Superior Intellectual Outcomes After Proton Radiotherapy Compared With Photon Radiotherapy for Pediatric Medulloblastoma. J Clin Oncol. 2019 Nov 27: [Epub ahead of print] PubMed PMID: 31774710.
2) Chung CS, Yock TI, Nelson K, Xu Y, Keating NL, Tarbell NJ. Incidence of second malignancies among patients treated with proton versus photon radiation. Int J Radiat Oncol Biol Phys. 2013;87(1):46-52. 3) Yock TI, Yeap BY, Ebb DH, Weyman E, Eaton BR, Sherry NA, Jones RM, MacDonald SM, Pulsifer MB, Lavally B, Abrams AN, Huang MS, Marcus KJ, Tarbell NJ Long-term toxic effects of proton radiotherapy for paediatric medulloblastoma: A phase 2 single-arm study. Lancet Oncol. 2016;17(3):287-298.
Are More Studies Really Needed?
Dr. James Cox, a prominent researcher from MD Anderson commented on this subject in an article in the Journal of Clinical Oncology. In the article he pointed out the fact that there is considerable documented evidence that with protons, there is two to three times less radiation deposited on healthy tissue, and radiation delivered to normal tissue causes damage to this tissue, and the severity of damage increases with increasing dose.
He states that, “We doubt that many of us, while healthy, would agree to receive, for example, 25 Gy to a large fraction of our brain or abdomen in exchange for some thousands of dollars, with no known or credibly hypothesized medical benefit. If we would not, how can we ask our sick patients to do so? Once proton beam therapy has become clinically available, is not the burden of proof on conventional x-ray therapy? Should not its advocates have to demonstrate that the cost savings achieved by using x-rays are not accompanied by undesirable additional morbidity? Do the users of x-ray therapy have the evidence to support such a claim?”
Myth #7: BUSTED!
Questions? Just ask.